The best fruits for diabetics are those with a low glycemic index (GI), specifically berries, citrus fruits, apples, and stone fruits like peaches. These options are packed with fiber, essential vitamins, and antioxidants that help regulate the body’s absorption of sugar, preventing dangerous glucose spikes. By focusing on whole, fresh fruits rather than juices or dried varieties, you can enjoy sweet flavors while maintaining healthy blood sugar levels. For individuals managing diabetes, fruit often represents a source of confusion; however, eliminating it entirely is unnecessary and potentially detrimental. Fruit provides essential micronutrients that support cardiovascular health and immune function. The key lies in strategic selection—choosing produce that releases glucose slowly into the bloodstream—and understanding how fiber acts as an internal regulatory system for metabolic health.
Understanding the Glycemic Index of Fruits

To navigate dietary choices effectively, one must first understand the metric used to evaluate them: the Glycemic Index (GI). The GI is a ranking system that assigns a numeric value (0 to 100) to foods based on how slowly or quickly they cause increases in blood glucose levels. Pure glucose serves as the reference point with a score of 100. When a person with diabetes consumes a high-GI fruit, the sugar is rapidly absorbed into the bloodstream, demanding a swift insulin response that a compromised metabolic system may struggle to provide.
For effective diabetes management, fruits with a low GI score—typically defined as 55 or less—are the safest and most beneficial choices. These foods undergo digestion and absorption at a slower rate, resulting in a gradual rise in blood sugar and insulin levels rather than a sharp spike. This “slow-release” energy is crucial for maintaining glycemic stability throughout the day. It is important to note that the GI is not the only factor; the Glycemic Load (GL), which accounts for the serving size, also plays a role. However, prioritizing low-GI fruits is the foundational step in constructing a diabetes-friendly diet that supports long-term health outcomes.
Berries: The Antioxidant Powerhouse
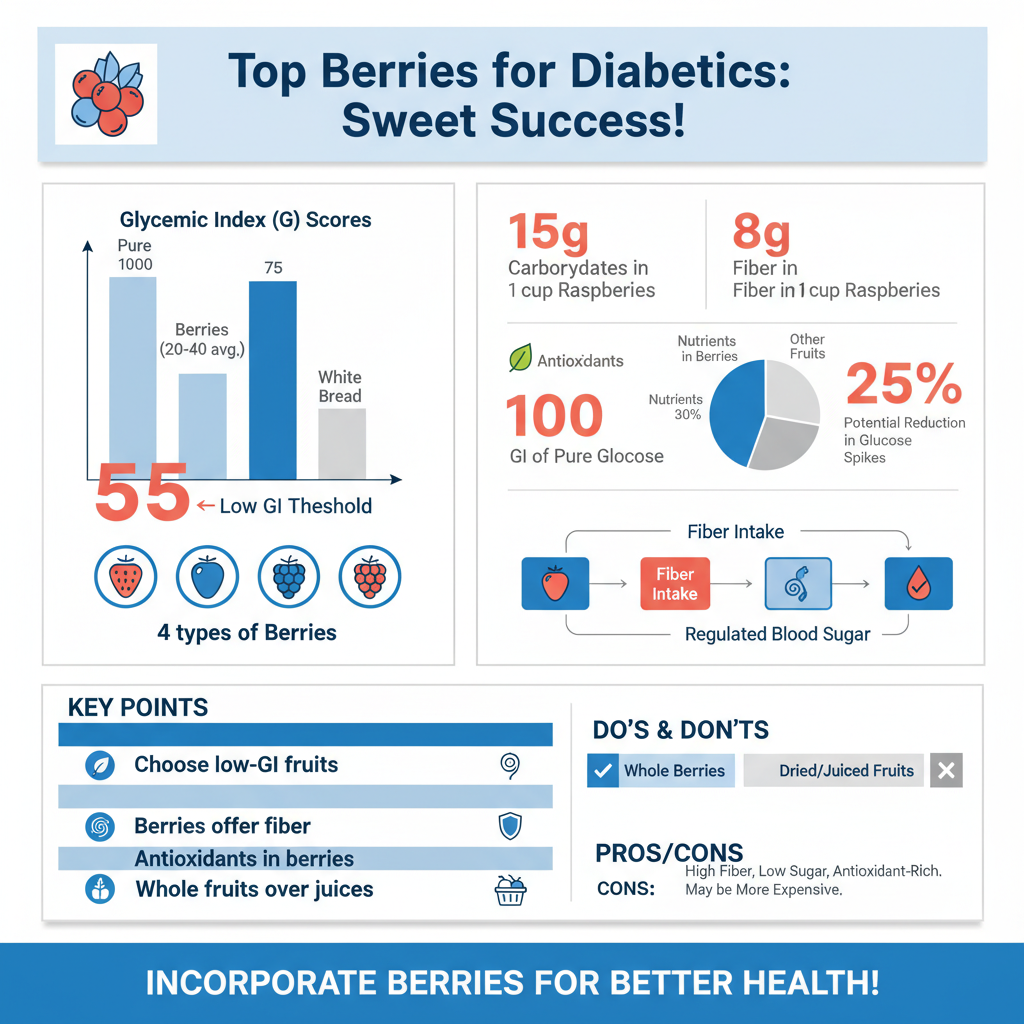

When categorized by nutritional density and glycemic impact, berries—specifically strawberries, blueberries, blackberries, and raspberries—consistently rank as the premier choice for diabetics. These fruits are naturally low in sugar compared to other varieties; for instance, a cup of raspberries contains approximately 15 grams of carbohydrates but boasts an impressive 8 grams of fiber. This high fiber-to-carb ratio drastically reduces the net impact on blood sugar, allowing for a sweet treat without the metabolic consequences associated with higher-sugar foods.
Beyond their macronutrient profile, berries are rich in bioactive compounds known as antioxidants, particularly anthocyanins, which give them their vibrant red and blue hues. Clinical studies suggest that anthocyanins may improve insulin sensitivity and glucose metabolism. By reducing oxidative stress and inflammation within the body, these antioxidants help preserve the function of beta-cells in the pancreas, which are responsible for producing insulin. Consequently, integrating a daily serving of berries is not merely a safe dietary choice; it is a proactive strategy for improving the body’s physiological response to sugar.
Citrus Fruits: Oranges, Grapefruit, and Lemons

Citrus fruits are renowned for their Vitamin C content, but for individuals with diabetes, their value lies in their fiber composition. Oranges, grapefruits, and lemons are excellent sources of soluble fiber. Unlike insoluble fiber, which adds bulk to stool, soluble fiber dissolves in water to form a gel-like substance in the gastrointestinal tract. This gel encapsulates food particles and slows down the emptying of the stomach, thereby delaying the entry of glucose into the bloodstream. This mechanism is vital for preventing post-prandial (post-meal) blood sugar spikes.
However, the method of consumption is critical when it comes to citrus. To gain these benefits, one must consume the whole fruit—pulp and segments included. The structural integrity of the fruit is where the fiber resides. Drinking fruit juice, even if freshly squeezed, removes this fiber matrix, leaving behind a concentrated sugar solution that enters the bloodstream rapidly. For example, eating a whole orange provides steady energy and satiety, whereas drinking a glass of orange juice can cause a rapid glycemic excursion similar to that of a sugary soda. Therefore, the professional recommendation is strictly to eat, not drink, your citrus.
Apples and Pears: High-Fiber Staples
Apples and pears are ubiquitous, affordable, and highly effective staples for a diabetic diet, provided they are consumed with their skins intact. The skin of these fruits houses the majority of their insoluble fiber and beneficial nutrients. An average-sized apple or pear provides a significant portion of the recommended daily fiber intake, acting as a physical barrier to rapid digestion. This fiber buffers the fructose naturally present in the fruit, ensuring a moderate glycemic response.
A specific component found in apples and pears is pectin, a type of soluble fiber that has been shown to improve glycemic control. Pectin creates a viscous environment in the gut, which not only slows glucose absorption but also feeds beneficial gut bacteria. A healthy gut microbiome is increasingly linked to better metabolic health and weight management. By promoting satiety, apples and pears also help prevent overeating, addressing the weight management aspect that is often central to Type 2 diabetes treatment plans.
Stone Fruits: Peaches, Plums, and Apricots
Stone fruits—named for the hard pit or “stone” at their center—include peaches, nectarines, plums, and apricots. These fruits are excellent low-carb options, particularly during the summer months when they are in season. A medium-sized peach, for example, typically contains fewer than 15 grams of carbohydrates and has a GI score well within the low range. They contain bioactive compounds like phenolic acids and flavonoids, which contribute to cardiovascular health—a primary concern for those managing diabetes.
The distinction between fresh and processed stone fruits is paramount. While fresh peaches and apricots are healthy choices, canned varieties require careful scrutiny. Many canned stone fruits are packed in “heavy syrup,” a solution of water and high-fructose corn syrup or sucrose. Consuming fruit in this medium negates the natural benefits of the fruit and introduces a massive load of free sugars that will spike blood glucose levels. When fresh options are unavailable, one should only select canned fruits packed in water or their own natural juice, and even then, draining the liquid is a prudent measure to reduce sugar intake.
Fruits to Limit or Avoid
While fruit is generally healthy, certain forms of fruit can be detrimental to diabetes management due to their caloric density and sugar concentration. Dried fruits, such as raisins, dates, dried cranberries, and figs, should be strictly limited or avoided. The drying process removes the water content, shrinking the fruit and concentrating the sugars. Consequently, a small handful of raisins contains the same amount of carbohydrates as a much larger volume of fresh grapes, but without the volume to signal fullness to the brain. This makes it incredibly easy to overconsume carbohydrates in a very short sitting, leading to rapid hyperglycemia.
Similarly, fruit juices and smoothies purchased from commercial vendors often pose a significant risk. Even smoothies that appear healthy can contain massive amounts of fruit puree, removing the necessary chewing process and fiber breakdown that signals satiety. Without the fiber to slow digestion, the sugar from juice hits the bloodstream almost instantly. Furthermore, many commercial smoothies include added syrups or sweeteners. For a diabetic, the glycemic load of a 16-ounce fruit smoothie can be equivalent to a large dessert, making these items generally unsuitable for blood sugar control.
Tips for Pairing Fruit with Protein
The metabolic impact of fruit can be further optimized through the strategic pairing of macronutrients. Eating carbohydrates in isolation causes a sharper rise in blood sugar than eating them alongside protein or healthy fats. These macronutrients take longer to digest, effectively slowing down the entire digestive process. For example, pairing an apple with a tablespoon of almond butter, or adding berries to a serving of plain Greek yogurt, significantly blunts the glucose spike compared to eating the fruit alone.
Portion control and timing are also essential best practices. Even low-GI fruits contain carbohydrates, and total carbohydrate load matters. A general guideline is to limit fruit servings to contain roughly 15 grams of carbohydrates per sitting—equivalent to a small apple or a cup of berries. Spreading fruit consumption throughout the day helps maintain stable energy levels, rather than consuming multiple servings at once. Many dietitians also recommend avoiding fruit late at night to prevent elevated fasting blood sugar levels the following morning.
Incorporating fruit into a diabetic diet is not only possible but beneficial when you choose options rich in fiber and low in sugar. Focus on whole berries, citrus, and apples, and always remember to pair them with protein to ensure steady energy levels. Consult with your dietitian to determine the best portion sizes for your specific health needs and start enjoying nature’s candy safely today. By moving away from restrictive thinking and toward educated selection and pairing, individuals with diabetes can harness the nutritional power of fruit to support a balanced, healthy, and flavorful lifestyle.
Frequently Asked Questions
What are the best fruits with a low glycemic index for diabetics?
Berries, including strawberries, blueberries, and raspberries, are among the best choices because they are packed with fiber and antioxidants while having a very low glycemic load. Tart fruits like green apples, cherries, and citrus fruits (oranges and grapefruit) are also excellent options as they release natural sugars slowly into the bloodstream. These fruits help satisfy sweet cravings without causing sudden spikes in blood glucose levels.
Can people with diabetes eat bananas and grapes safely?
Yes, diabetics can eat higher-sugar fruits like bananas and grapes, but strict portion control and timing are essential to manage blood sugar impact. Because these fruits have a higher carbohydrate density, it is best to stick to a small serving, such as half a banana or a small handful of grapes (about 15 grapes). Pairing these fruits with a healthy fat or protein, like nuts or Greek yogurt, can further help slow down digestion and glucose absorption.
Why is eating whole fruit better than drinking fruit juice for blood sugar control?
Whole fruits contain essential dietary fiber, specifically in the skin and pulp, which acts as a natural barrier to slow down the absorption of sugar into the bloodstream. Fruit juice strips away this fiber, resulting in a concentrated dose of liquid sugar that can cause rapid and dangerous blood glucose spikes. For optimal diabetes management, always prioritize fresh or frozen whole fruit over juiced alternatives.
How many servings of fruit should a diabetic eat per day?
Most dietary guidelines for diabetes suggest consuming 2 to 3 servings of fruit per day, provided they are spaced out rather than eaten all at once. A standard serving typically contains about 15 grams of carbohydrates, which looks like one small apple, one cup of berries, or half a cup of canned fruit in water. Counting carbohydrates is the most effective way to ensure fruit intake fits within your personal daily limits.
Which dried fruits are safe for a diabetic diet?
Dried fruits should generally be consumed with extreme caution because the dehydration process concentrates the sugar and calories into a very small volume. If you choose to eat dried fruit, strictly limit the portion to about two tablespoons and ensure there are no added sugars or syrups listed on the package. Options like dried apricots or prunes can be acceptable in moderation, but fresh fruit is almost always the superior choice for glycemic control.
References
- Best Fruit Choices for Diabetes | ADA
- https://health.clevelandclinic.org/what-are-the-best-fruits-for-you-if-you-have-diabetes
- Healthy Living with Diabetes – NIDDK
- Diabetes diet: Create your healthy-eating plan – Mayo Clinic
- Fruit, vegetables and diabetes | Eating with diabetes | Diabetes UK
- Healthy Eating | Diabetes | CDC
- Diabetes Teaching Center