The best fruits for diabetics include berries, citrus fruits, tart cherries, apples, and pears because they have a low glycemic index and are packed with fiber. While living with diabetes requires careful monitoring of carbohydrate intake and maintaining awareness of blood glucose trends, you do not have to eliminate fruit entirely; focusing on these nutrient-dense options can actually help regulate blood sugar levels. Navigating a diabetic diet is about making strategic choices rather than absolute restrictions. This article breaks down the nutritional benefits of each fruit and how to safely incorporate them into your meal plan to maximize health benefits while minimizing glycemic variability.
1. Berries: Powerhouses of Antioxidants

When consulting nutritionists regarding diabetes management, berries are almost universally the first recommendation. Blueberries, strawberries, raspberries, and blackberries are distinguished not only by their nutritional density but by their exceptionally low glycemic load (GL). Unlike the Glycemic Index (GI), which measures how a carbohydrate affects blood sugar, the Glycemic Load accounts for the serving size. Berries score low on both fronts, meaning a standard serving produces a minimal rise in blood glucose compared to tropical fruits like bananas or pineapples.
The primary mechanism making berries suitable for diabetic diets is their high fiber content. Raspberries, for instance, contain an impressive amount of fiber—roughly 8 grams per cup. This dietary fiber, particularly the soluble variety, forms a gel-like substance in the gut that slows down the digestion process. Consequently, the release of glucose into the bloodstream is delayed, preventing the rapid spikes that can be dangerous for individuals with insulin resistance.
Furthermore, berries are rich in anthocyanins, the pigments that give them their red, blue, and purple hues. Research suggests that anthocyanins may improve insulin sensitivity and glucose metabolism. By reducing oxidative stress and inflammation—two conditions often exacerbated by high blood sugar—berries serve as a functional food that supports long-term metabolic health. Incorporating a cup of mixed berries into morning oatmeal or yogurt provides a safe, sweet flavor profile without compromising glycemic control.
2. Citrus Fruits: Oranges and Grapefruits
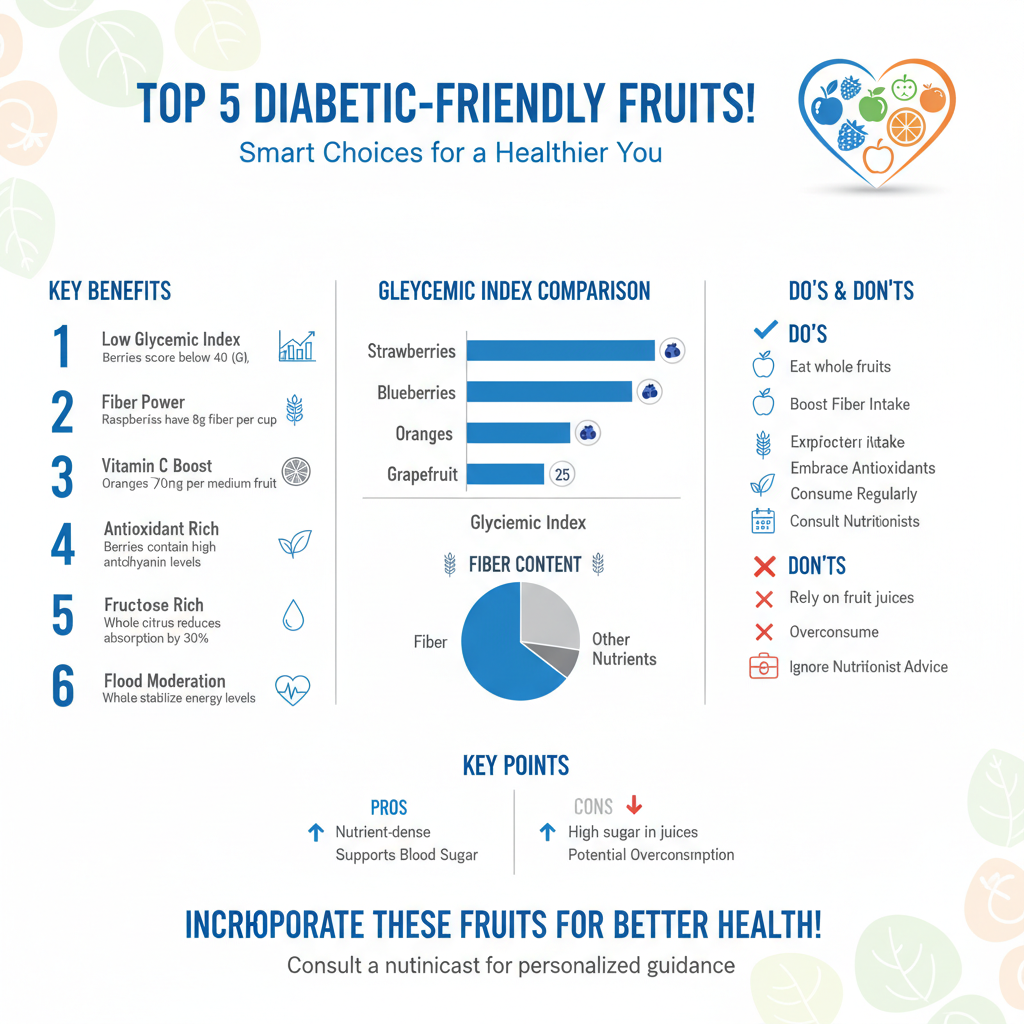

Citrus fruits are often misunderstood in the context of diabetes due to the high sugar concentration found in their juices. However, whole citrus fruits like oranges and grapefruits are excellent choices for blood sugar management. The distinction lies in the delivery method: consuming the whole fruit provides essential fiber that is stripped away during the juicing process. This fiber is critical for moderating the absorption of fructose and stabilizing energy levels.
Oranges and grapefruits are renowned for their Vitamin C content, but they also contain a wealth of other bioactive compounds. For example, grapefruits contain naringenin, a flavonoid that has been shown to improve insulin sensitivity and help the liver burn fat rather than store it. This can be particularly beneficial for individuals managing Type 2 diabetes, where insulin resistance is a primary concern. Additionally, the fiber pectin found in citrus fruits is effective in lowering LDL cholesterol levels, addressing the cardiovascular risks often associated with diabetes.
It is important to note that while whole citrus fruits promote glycemic control and fight inflammation, grapefruits can interact with certain medications, including statins and blood pressure drugs. Therefore, individuals on prescription regimens should consult their healthcare provider before adding grapefruit to their regular diet. For most, however, a medium-sized orange or half a grapefruit serves as a refreshing, low-glycemic snack that supports immune function and metabolic stability.
3. Tart Cherries: Low-Sugar Inflammation Fighters

Not all cherries are created equal when it comes to diabetes management. It is essential to distinguish between sweet cherries (such as Bing cherries) and tart cherries (such as Montmorency). While sweet cherries can be part of a healthy diet in moderation, they possess a higher sugar content. Tart cherries, conversely, have a significantly lower glycemic index and lower sugar density, making them a superior option for minimizing postprandial glucose spikes.
The true value of tart cherries lies in their potent anti-inflammatory properties. Diabetes is often characterized as a pro-inflammatory state, which can lead to complications affecting the heart, kidneys, and nerves. Tart cherries are rich in antioxidants, specifically anthocyanins, which have been shown to reduce markers of inflammation and oxidative stress in the body. Regular consumption can support heart health—a critical consideration given the correlation between diabetes and cardiovascular disease.
Moreover, tart cherries contain naturally occurring melatonin, which can improve sleep quality. Poor sleep patterns are known to disrupt hormones that regulate hunger and blood sugar, such as ghrelin and cortisol. by promoting better rest and reducing systemic inflammation, tart cherries offer a dual-approach benefit to managing the physiological stress of diabetes. They can be consumed fresh, frozen, or dried (provided there is no added sugar), offering versatility in meal planning.
4. Apples: The Ultimate Fiber Source
The adage about “an apple a day” holds particular weight for those managing diabetes, provided the fruit is consumed correctly. Apples are a premier source of fiber, but the majority of this nutrient—as well as the highest concentration of antioxidants—is found in the skin. Peeling an apple removes the insoluble fiber needed to blunt the absorption of the fruit’s natural sugars. Therefore, eating the apple intact is non-negotiable for maximizing its health potential.
Apples are particularly high in pectin, a soluble fiber that dissolves in water to form a viscous substance in the intestines. This process is highly effective at slowing gastric emptying, which means sugar enters the bloodstream at a manageable trickle rather than a flood. Furthermore, the skin contains quercetin, a flavonoid that may help reduce the risk of Type 2 diabetes and improve carbohydrate metabolism.
Portion control remains a key factor when consuming apples. Modern agriculture has produced apple varieties that are significantly larger than their historical counterparts. For a diabetic meal plan, selecting small to medium-sized apples (roughly the size of a tennis ball) is advisable to keep the carbohydrate load within a target range (usually 15 to 20 grams of carbs). To further mitigate any potential rise in blood sugar, apples should be viewed as a vehicle for protein; pairing apple slices with a handful of walnuts or a slice of cheddar cheese creates a macronutrient balance that sustains energy levels for hours.
5. Pears: High Fiber and Vitamin K
Pears are frequently overlooked in favor of apples, yet they are structurally one of the most beneficial fruits for blood glucose management. A medium-sized pear offers approximately 6 grams of fiber—one of the highest counts per serving in the fruit kingdom. This high fiber-to-sugar ratio makes pears an excellent tool for inducing satiety. Feeling full longer helps prevent overeating and snacking on less healthy options, assisting with weight management, which is often a crucial component of diabetes care.
Beyond fiber, pears provide a good source of Vitamin K and copper, micronutrients that support bone health and metabolic function. However, the glycemic impact of a pear can change depending on its ripeness. As a pear ripens and becomes soft, its starch content converts into simple sugars, potentially increasing its glycemic index. For the best blood sugar control, it is advisable to select pears that are firm to the touch.
Eating the skin is just as important with pears as it is with apples. The skin contains the bulk of the fruit’s phenolic phytonutrients. When shopping, consider varieties like D’Anjou or Bartlett, and store them in the refrigerator to slow the ripening process. Slicing a firm pear into a salad with leafy greens and a vinaigrette is an excellent way to introduce natural sweetness to a savory meal without spiking insulin levels.
6. Tips for Eating Fruit with Diabetes
Successfully incorporating fruit into a diabetic diet requires more than just selecting the right types; it requires a strategic approach to consumption habits. The most critical concept to master is portion control. Even low-glycemic fruits contain carbohydrates that eventually convert to glucose. Understanding that a “serving” of fruit generally equates to about 15 grams of carbohydrates allows for better calculation of daily intake. Using a food scale or familiarizing oneself with visual comparisons (e.g., a serving of berries is about one cup) ensures that “healthy” eating does not inadvertently lead to hyperglycemia.
Another vital strategy is the utilization of the Glycemic Index (GI) as a guide, though not the sole determinant. The GI ranks foods on a scale of 0 to 100 based on how much they raise blood sugar. Aiming for fruits with a GI of 55 or lower helps ensure a slower release of energy. However, this must be paired with the concept of food synergy.
Eating fruit on an empty stomach can sometimes lead to faster sugar absorption. The most effective way to stabilize blood sugar is to pair carbohydrates with healthy fats and proteins. This combination slows down digestion significantly. For example, rather than eating an apple alone, consume it with almond butter. Instead of a bowl of berries, mix them into Greek yogurt. These pairings buffer the impact of fructose, flattening the glucose curve and preventing the “crash” that often follows a sugar spike. Finally, timing matters; spacing fruit intake throughout the day prevents carbohydrate loading at any single meal.
Managing diabetes doesn’t mean saying goodbye to nature’s candy; it simply requires choosing fruits like berries, citrus, cherries, apples, and pears that support stable blood sugar. By focusing on whole fruits rich in fiber and monitoring your portion sizes, you can enjoy a varied and nutritious diet. Start by adding a small serving of these fruits to your breakfast or snack time today to boost your nutrient intake safely.
Frequently Asked Questions
Which fruits have the lowest glycemic index (GI) for managing diabetes?
The best fruits for diabetics with a low glycemic index include berries (strawberries, blueberries, raspberries), tart cherries, apples with the skin on, pears, and citrus fruits like grapefruit. These fruits release glucose into the bloodstream slowly, preventing dangerous blood sugar spikes while providing essential vitamins and fiber. Choosing fruits with a GI score of 55 or less is generally recommended for maintaining stable insulin levels.
Why are berries often recommended as the number one fruit for diabetics?
Berries are considered a diabetes superfood because they pack a high amount of fiber and antioxidants called anthocyanins into a low-carbohydrate package. The fiber content helps slow down digestion and sugar absorption, while the antioxidants may help improve insulin sensitivity. Whether fresh or frozen, berries like blackberries and raspberries offer sweetness without the heavy glycemic load found in tropical fruits.
Can people with diabetes still eat bananas and melons safely?
Yes, diabetics can eat higher-sugar fruits like bananas and melons, but portion control and ripeness are key factors to consider. It is best to choose slightly green bananas, which contain resistant starch that acts less like sugar, and to limit melon servings to small portions. To minimize blood sugar spikes, try pairing these higher-carb fruits with a source of protein or healthy fat, such as a handful of nuts or Greek yogurt.
Is it better for diabetics to drink fruit juice or eat whole fruit?
Medical experts almost universally recommend eating whole fruit rather than drinking fruit juice for blood sugar management. Whole fruits contain soluble fiber, which is crucial for slowing down the absorption of sugar, whereas juice is a concentrated source of sugar that enters the bloodstream rapidly. Drinking juice can lead to immediate glucose spikes, while whole fruit promotes satiety and steady energy levels.
How can I prevent fruit from spiking my blood sugar levels?
The most effective way to enjoy fruit without a glucose spike is to never eat it on an empty stomach and always pair it with a protein or fat source. For example, eating apple slices with peanut butter or berries with cottage cheese slows down digestion and blunts the insulin response. Additionally, sticking to specific serving sizes—typically one cup of berries or one medium-sized piece of fruit—helps keep carbohydrate intake within a safe range.
References
- https://health.clevelandclinic.org/what-are-the-best-fruits-for-a-diabetic
- Diabetes diet: Should I avoid sweet fruits? – Mayo Clinic
- Fruit, vegetables and diabetes | Eating with diabetes | Diabetes UK
- Vegetables for diabetes: Choices, benefits, and meal tips
- Healthy Living with Diabetes – NIDDK
- https://www.health.harvard.edu/staying-healthy/the-truth-about-fruit-and-diabetes
- Healthy Eating | Diabetes | CDC