While no supplement can cure Type 2 Diabetes, certain options like Berberine, Alpha-Lipoic Acid, Chromium, and Magnesium have shown promising potential in supporting blood sugar management and overall metabolic health when integrated responsibly with conventional medical treatments. This guide will help you understand these options and the critical considerations for their use, empowering you to make informed decisions with your healthcare provider.
The Role of Supplements in Type 2 Diabetes Management

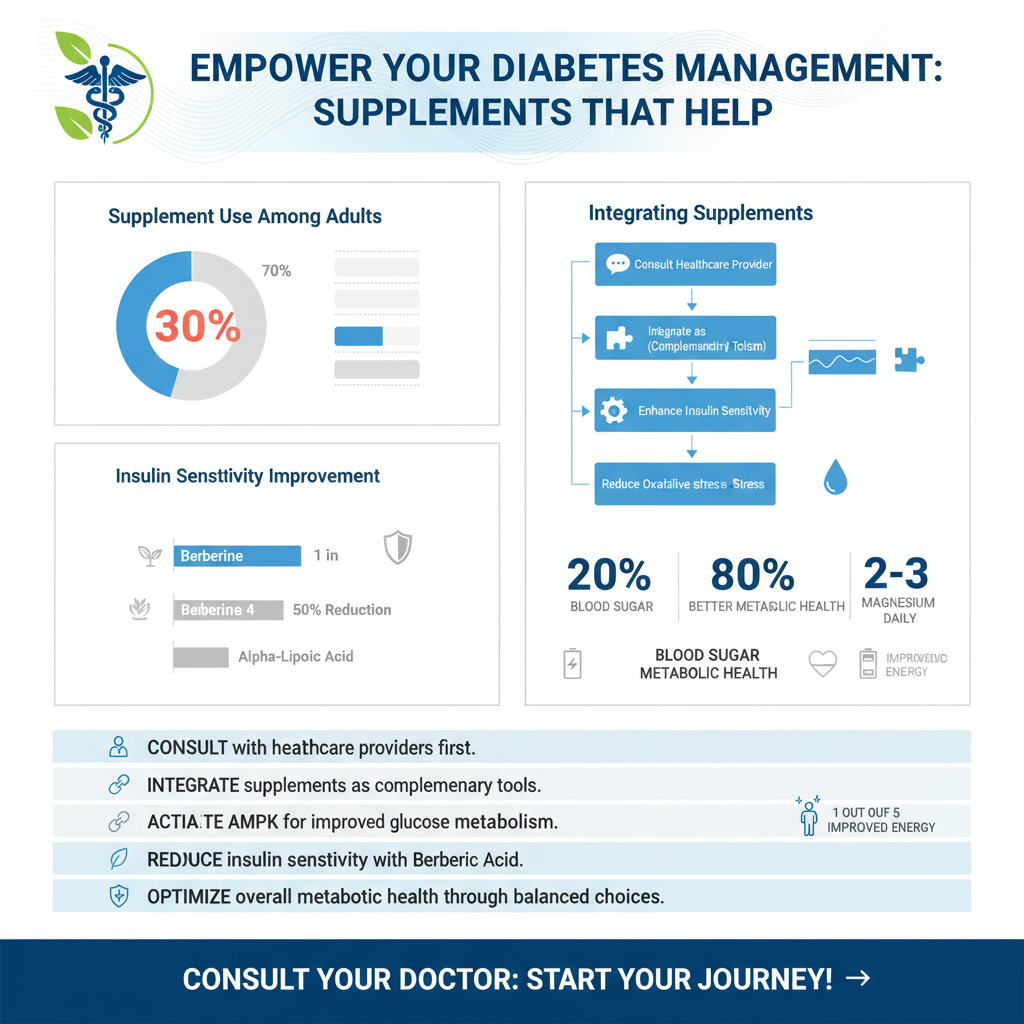
Living with Type 2 Diabetes often involves a multi-faceted approach, combining medication, dietary adjustments, and regular exercise. In this comprehensive strategy, supplements can play a valuable, yet supporting, role. It’s really important to view them as complementary tools, not as substitutes for your prescribed medications or the fundamental lifestyle changes that form the bedrock of diabetes management. Think of them as additional allies in your journey towards better health.
The primary aim of integrating supplements into a Type 2 Diabetes regimen is to support various aspects of the condition, helping your body function more efficiently. This includes areas like improving insulin sensitivity, which means your cells respond better to the insulin your body produces, thus utilizing glucose more effectively. They can also aid in optimizing glucose metabolism, ensuring that the sugars you consume are processed and used for energy rather than accumulating in your bloodstream. Furthermore, many supplements offer antioxidant protection, which is particularly beneficial for individuals with diabetes, as chronic high blood sugar can lead to increased oxidative stress and inflammation, potentially damaging cells and tissues over time.
Given their potential impact on your body and their interaction with other treatments, the golden rule for anyone considering supplements is to always consult your healthcare provider first. This step is absolutely non-negotiable. Your doctor can help you determine if a particular supplement is safe for you, considering your overall health status, existing medications, and any potential allergies or sensitivities. They can also advise on appropriate dosages and help you avoid adverse interactions, ensuring that any supplement you choose works with your current treatment plan, not against it. It’s all about making informed, safe choices that support your well-being.
Top-Researched Supplements for Blood Sugar Support

When it comes to specific supplements with significant research backing for blood sugar support, two stand out: Berberine and Alpha-Lipoic Acid. These aren’t magic bullets, but they have mechanisms that could be very beneficial.
* Berberine: This is a natural compound found in several plants, and it has garnered considerable attention in the diabetes community. Berberine is primarily known for its remarkable ability to activate AMPK (AMP-activated protein kinase), which is often referred to as a “metabolic master switch.” Think of AMPK as your body’s energy sensor. When activated, it helps improve insulin sensitivity, making your cells more receptive to insulin and better able to absorb glucose from the blood. Critically, Berberine also helps reduce glucose production in the liver, which is a major contributor to high fasting blood sugar levels in people with Type 2 Diabetes. By doing this, Berberine essentially helps your body manage glucose more efficiently from multiple angles, leading to potentially lower blood sugar levels. Many studies have compared its efficacy to some conventional diabetes medications, showing promising results, but it’s vital to discuss appropriate dosages and potential side effects with your doctor.
* Alpha-Lipoic Acid (ALA): ALA is a powerful antioxidant that your body naturally produces, and it’s also found in certain foods. It’s a bit of a superstar because it’s both water- and fat-soluble, allowing it to work throughout the body. For individuals with Type 2 Diabetes, ALA offers several potential benefits. Firstly, it may improve insulin sensitivity, similar to Berberine, by enhancing glucose uptake into cells. Secondly, its potent antioxidant properties are crucial for combating oxidative stress, which is often elevated in diabetes and can contribute to complications. By neutralizing harmful free radicals, ALA can help protect cells and tissues from damage. Thirdly, and perhaps most notably, ALA has been widely studied for its potential to alleviate symptoms of diabetic neuropathy, a type of nerve damage that can cause pain, tingling, and numbness, especially in the hands and feet. While it won’t cure neuropathy, many people report a reduction in discomfort. When considering ALA, it’s often recommended in the R-ALA form for better bioavailability, and your doctor can guide you on the right dosage.
Essential Vitamins and Minerals for Metabolic Health

Beyond specific compounds, several essential vitamins and minerals play foundational roles in our metabolic health, and deficiencies can exacerbate issues for those managing Type 2 Diabetes. Ensuring adequate levels of these micronutrients can be a smart move.
* Chromium: This trace mineral plays a truly vital role in carbohydrate and lipid metabolism. It’s a key component of a molecule called chromodulin, which is believed to enhance the action of insulin. Think of chromium as a helpful assistant that makes insulin’s job easier. By potentially improving the efficiency of insulin, chromium can lead to better glucose tolerance, meaning your body can handle sugar more effectively after meals. While severe chromium deficiency is rare, marginal deficiencies might impair glucose metabolism. Supplementation is often considered, but it’s important to remember that too much can also be problematic, so always check with your doctor before starting.
* Magnesium: Often overlooked, magnesium is absolutely essential for over 300 enzymatic reactions in the human body, and a significant number of these are involved in glucose metabolism and insulin secretion. From breaking down glucose for energy to producing and releasing insulin, magnesium is a silent workhorse. Unfortunately, deficiency is remarkably common in the general population, and even more so in individuals with Type 2 Diabetes. This is because high blood sugar can increase magnesium excretion through the kidneys, creating a vicious cycle. Addressing a magnesium deficiency might improve insulin sensitivity, help with blood sugar control, and even reduce the risk of diabetes complications. Incorporating magnesium-rich foods like leafy greens, nuts, seeds, and whole grains is a great start, and supplementation might be recommended under medical guidance, especially if a deficiency is confirmed.
* Vitamin D: More than just a vitamin for bone health, Vitamin D is increasingly recognized for its widespread impact on overall health, including its strong links to insulin sensitivity and pancreatic beta-cell function. The beta cells in your pancreas are responsible for producing and secreting insulin, and adequate Vitamin D levels appear to support their healthy function. Studies have consistently suggested that optimizing Vitamin D levels may benefit blood sugar control, and deficiency has been associated with an increased risk of developing Type 2 Diabetes and poorer outcomes for those who already have it. Given that many people are deficient in Vitamin D, especially in less sunny climates, checking your levels through a simple blood test and supplementing under your doctor’s supervision is a sensible step for comprehensive diabetes management.
Herbal Options and Antioxidants
Nature provides a wealth of compounds that have been traditionally used for health support, and some herbs and plant-derived antioxidants show promise in complementing diabetes management.
* Cinnamon: This beloved spice isn’t just for adding flavor to your morning oatmeal; some studies suggest it may offer benefits for blood sugar control. Certain compounds in cinnamon are believed to help improve insulin sensitivity, meaning your cells become more responsive to insulin. This can lead to a more efficient uptake of glucose from the blood. While the effects are generally considered modest, particularly after meals, some research indicates a potential for lowering fasting blood glucose and improving lipid profiles. It’s worth noting that not all cinnamon is created equal; Ceylon cinnamon is often preferred over Cassia cinnamon (which contains higher levels of coumarin, potentially harmful in large doses) for regular therapeutic use. Discussing the appropriate type and dosage with a healthcare professional is key.
* Bitter Melon: This unique fruit, often used in traditional medicine, particularly in Asian countries, has a long history of use for lowering blood sugar. It contains several bioactive compounds, including charantin, vicine, and polypeptide-p, which are thought to act similarly to insulin or improve glucose uptake and utilization by the cells. Some researchers even refer to polypeptide-p as “plant insulin.” Bitter melon may help improve insulin secretion, reduce intestinal glucose absorption, and enhance glucose metabolism in various tissues. While more robust clinical trials are still needed to fully understand its full potential and optimal dosing, it represents an intriguing natural option that many individuals find beneficial for blood sugar management. It can be consumed as a food, juice, or supplement, but its strong flavor might not appeal to everyone.
* Green Tea Extract: A powerhouse of antioxidants, green tea extract is rich in compounds called catechins, particularly epigallocatechin gallate (EGCG). These antioxidants are well-known for their ability to combat oxidative stress and inflammation, which are significant concerns for individuals with diabetes. Beyond its general health benefits, green tea extract may offer modest benefits for blood sugar regulation by improving insulin sensitivity and reducing glucose absorption. Furthermore, its positive impact on cardiovascular health—a critical consideration for people with Type 2 Diabetes—is also well-documented. Regular consumption of green tea or supplementation with green tea extract can be a simple, pleasant addition to a holistic health strategy, but as always, discuss dosage and potential interactions with your doctor, especially if you have liver conditions or are on certain medications.
Crucial Considerations Before Supplementation
Embarking on a journey with supplements can feel empowering, but it’s essential to approach it with careful consideration and an informed perspective. The world of supplements isn’t always as straightforward as it seems, especially when managing a condition like Type 2 Diabetes.
* Consult Your Doctor: This cannot be stressed enough – it is absolutely paramount! Before you even think about adding any new supplement to your regimen, you must discuss it thoroughly with your healthcare provider. Why? Because they know your complete medical history, your current medications, and your specific health needs. They can help you weigh the potential benefits against any risks, advise on the correct dosages (which can vary widely), and crucially, identify any potential interactions with your existing medications. For example, some supplements can amplify or diminish the effects of prescribed drugs, leading to dangerous highs or lows in blood sugar. Your doctor’s guidance ensures that your supplement choices are safe, effective, and truly complementary to your overall diabetes management plan.
* Quality and Purity: The supplement industry is vast and not as tightly regulated as the pharmaceutical industry. This means that the quality and purity of supplements can vary dramatically between brands. It’s incredibly important to choose supplements from reputable brands that are transparent about their sourcing and manufacturing processes. Look for brands that undergo third-party testing, often indicated by certifications from organizations like USP (U.S. Pharmacopeia), NSF International, or ConsumerLab.com. These certifications confirm that the product contains what its label claims, is free from harmful contaminants (like heavy metals or pesticides), and dissolves properly for absorption. Investing in high-quality supplements protects your health and ensures you’re getting the active ingredients you expect.
* Potential Side Effects & Interactions: The misconception that “natural” equals “safe” can be dangerous. Even natural supplements can have significant side effects or interact negatively with other drugs or existing health conditions. For instance, Berberine can cause gastrointestinal upset, and large doses of Chromium can be problematic for individuals with kidney issues. Some herbal supplements can thin the blood, interacting dangerously with anticoagulant medications. It’s vital to be aware of these possibilities and to monitor your body closely when introducing a new supplement. If you experience any unusual symptoms or side effects, stop taking the supplement immediately and contact your doctor. Open communication with your healthcare team is key to navigating these potential challenges safely.
Holistic Approach to Diabetes Management
While supplements can offer valuable support, it’s crucial to remember that they are just one piece of a much larger, more integrated puzzle. A truly effective strategy for managing Type 2 Diabetes is always holistic, encompassing multiple aspects of your lifestyle and medical care.
* Lifestyle Foundations: The absolute cornerstones of effective Type 2 Diabetes management remain consistent: a healthy diet, regular physical activity, and maintaining a healthy weight. No supplement, no matter how promising, can replace these fundamental lifestyle changes. A balanced diet, often emphasizing whole foods, controlled carbohydrate intake, plenty of fiber, and healthy fats, directly impacts blood sugar levels. Regular exercise, whether it’s walking, cycling, or strength training, improves insulin sensitivity and helps with weight management. And achieving and maintaining a healthy weight significantly reduces the burden on your body’s metabolic system. These lifestyle factors are your primary tools for taking control of your health and are non-negotiable for long-term well-being.
* Regular Monitoring: Knowledge is power, and when it comes to Type 2 Diabetes, that means continuously monitoring your blood glucose levels. This includes checking your fasting blood sugar, post-meal levels, and periodically reviewing your A1C (which gives an average blood sugar reading over 2-3 months). Regular monitoring is essential because it provides immediate feedback on how your body is responding to your management plan, including your diet, exercise, medications, and any supplements you might be taking. This data empowers you and your healthcare team to make informed adjustments, ensuring your plan remains effective and tailored to your evolving needs. Don’t underestimate the power of seeing your numbers and understanding what impacts them.
* Personalized Strategy: Every individual’s journey with Type 2 Diabetes is unique, and what works wonderfully for one person might not be suitable for another. This is why developing a personalized strategy is so critical. Work closely and collaboratively with your healthcare team—your doctor, a registered dietitian, a certified diabetes educator, or even a personal trainer. Together, you can integrate medical treatments (medications, insulin), lifestyle modifications (diet, exercise), and carefully selected supplements into a cohesive plan that is specifically designed for *you*. This personalized approach takes into account your preferences, challenges, existing health conditions, and lifestyle, ensuring the most effective and sustainable path towards optimal health and blood sugar control.
While supplements like Berberine, Alpha-Lipoic Acid, Chromium, Magnesium, and Vitamin D show promise in supporting blood sugar control for individuals with Type 2 Diabetes, they are complements, not cures. The most effective approach always combines prescribed medications, a healthy diet, regular exercise, and consistent monitoring. Before initiating any new supplement, always consult your healthcare provider to ensure it’s safe and appropriate for your specific health needs and medication regimen. Remember, your healthcare team is your best resource for building a comprehensive, personalized plan that helps you thrive with Type 2 Diabetes.
Frequently Asked Questions
What are the most commonly recommended supplements to help manage blood sugar for Type 2 diabetes?
Several supplements are frequently discussed for their potential role in supporting blood sugar management for Type 2 diabetes. Popular choices include berberine, known for its ability to activate AMPK, an enzyme that regulates metabolism and glucose uptake; chromium picolinate, which may enhance insulin sensitivity; and alpha-lipoic acid, an antioxidant that can improve glucose utilization. These supplements are often explored as complementary tools alongside conventional treatments and lifestyle adjustments.
How do specific supplements like berberine or chromium picolinate actually work to improve glucose control in Type 2 diabetes?
Berberine helps improve glucose control by activating AMP-activated protein kinase (AMPK), often called the “metabolic master switch,” which leads to increased glucose uptake by cells and reduced glucose production by the liver. Chromium picolinate, on the other hand, is believed to enhance the action of insulin, thereby improving insulin sensitivity and helping the body process glucose more effectively. Both can contribute to more stable blood sugar levels for individuals with Type 2 diabetes.
Are there any important safety considerations or potential side effects when taking supplements for Type 2 diabetes?
Yes, ensuring safety is crucial when considering supplements for Type 2 diabetes. Some supplements can interact with prescribed diabetes medications, potentially leading to dangerously low blood sugar (hypoglycemia) or other adverse effects. For instance, berberine can lower blood sugar significantly, and high doses of alpha-lipoic acid might also impact glucose levels. Always consult your doctor or a registered dietitian before starting any new supplement to discuss potential interactions, appropriate dosages, and monitor for side effects.
Can supplements alone effectively treat Type 2 diabetes, or do they need to be combined with lifestyle changes and medication?
Supplements should not be considered a standalone treatment for Type 2 diabetes, nor can they replace prescribed medications or a healthy lifestyle. They are best viewed as complementary tools that can support overall blood sugar management when integrated into a comprehensive plan. Effective control of Type 2 diabetes fundamentally relies on dietary changes, regular physical activity, and often, pharmaceutical interventions, with supplements potentially offering additional support to these core strategies.
Which vitamins and minerals are often found to be deficient in individuals with Type 2 diabetes, and can supplementation help?
Individuals with Type 2 diabetes often experience deficiencies in certain vitamins and minerals, notably magnesium and Vitamin D, which play roles in insulin sensitivity and glucose metabolism. Some research also suggests potential deficiencies in B vitamins and zinc. Supplementing these nutrients, especially if a deficiency is confirmed by a doctor, might help address underlying issues that contribute to insulin resistance or nerve damage, but it’s essential to get levels checked before starting supplementation.
References
- Hypothyroidism: Should I take iodine supplements? – Mayo Clinic
- https://diabetes.org/health-wellness/complementary-alternative-medicine
- https://www.nccih.nih.gov/health/diabetes-and-dietary-supplements-what-the-science-says
- https://www.health.harvard.edu/diseases-and-conditions/is-there-a-role-for-supplements-in-treating-type-2-diabetes
- https://health.clevelandclinic.org/can-supplements-help-you-manage-type-2-diabetes/
- https://medlineplus.gov/druginfo/natural/932.html
- Type 2 diabetes