For the vast majority of patients, Metformin is considered the “best” first-line medicine for type 2 diabetes due to its safety, affordability, and effectiveness at lowering blood sugar without causing weight gain. However, for patients prioritizing weight loss or heart health, newer GLP-1 receptor agonists (like Ozempic or Mounjaro) and SGLT2 inhibitors are increasingly viewed as top-tier options. Ultimately, the best medication depends on your specific A1C levels, cardiovascular health, and tolerance for side effects. While the medical community has relied on established protocols for decades, the landscape of diabetes management has shifted dramatically in recent years. The focus has moved beyond simply lowering glucose numbers to a more holistic approach that prioritizes organ protection and weight management. Understanding the strengths and mechanisms of each medication class is essential for patients to engage in informed discussions with their healthcare providers.
Metformin: The Gold Standard First-Line Treatment

For decades, Metformin has maintained its position as the foundational therapy for type 2 diabetes management globally. Its status as the “gold standard” is endorsed by major organizations, including the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD).
Mechanism of Action
Metformin primarily works by targeting the liver. In people with type 2 diabetes, the liver often continues to release glucose into the bloodstream even when blood sugar levels are already high. Metformin inhibits this process, known as hepatic gluconeogenesis. Additionally, it acts as an “insulin sensitizer,” improving the body’s sensitivity to its own insulin, thereby helping muscle tissue absorb glucose more effectively.
Key Benefits and Safety Profile
The enduring popularity of Metformin is driven by a unique combination of clinical benefits:
* Affordability: As a generic medication, Metformin is widely available at a very low cost, making it accessible to patients regardless of insurance status.
* Weight Neutrality: Unlike older medications that often spurred weight gain, Metformin is weight-neutral and may even promote modest weight loss in some patients.
* Safety History: With over 60 years of clinical use, its long-term safety profile is well-documented. It does not cause hypoglycemia (dangerously low blood sugar) when used as a monotherapy.
* Cardiovascular Safety: While not as potent as newer drugs regarding heart protection, Metformin has shown potential benefits in reducing cardiovascular events in overweight patients.
While some patients experience gastrointestinal side effects, such as nausea or diarrhea, these can often be mitigated by starting with a low dose, taking the medication with food, or utilizing extended-release formulations.
GLP-1 Receptor Agonists (Injectables)
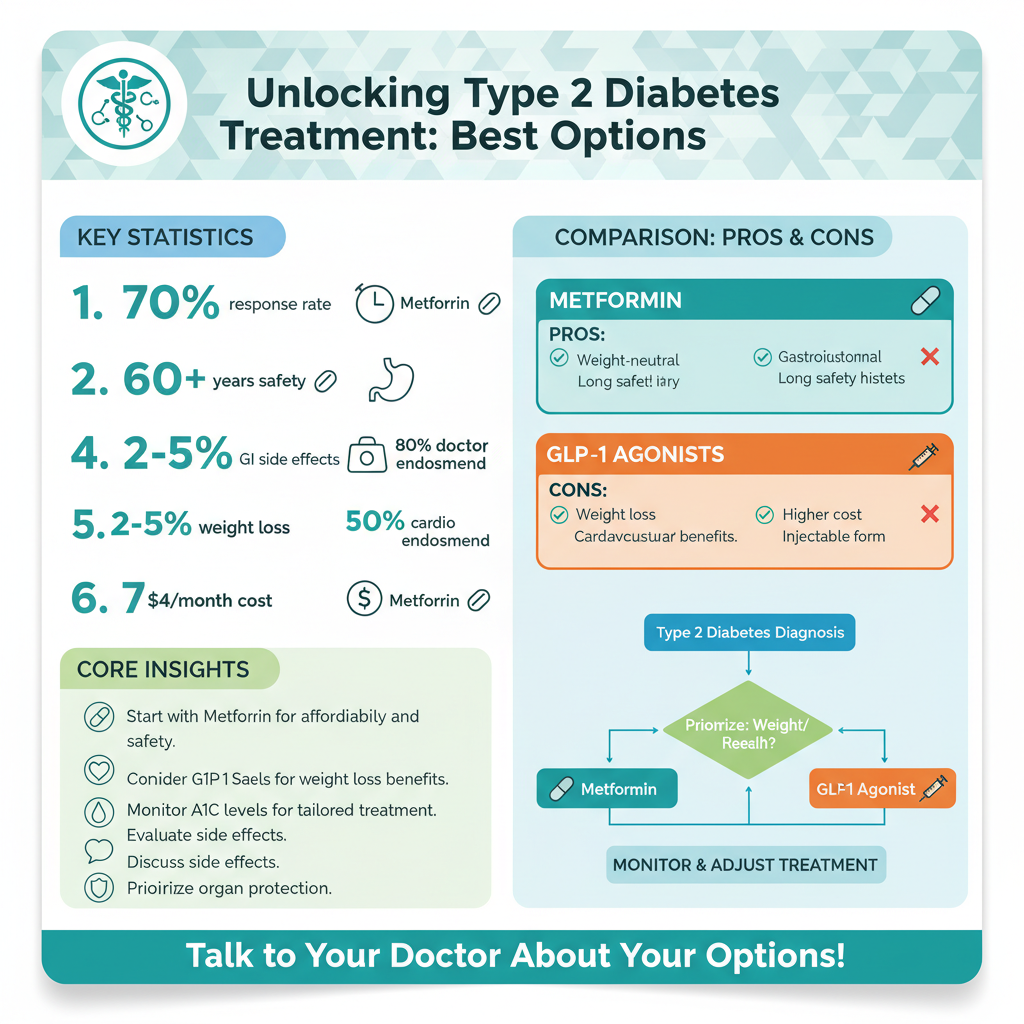

The introduction of Glucagon-like Peptide-1 (GLP-1) receptor agonists has revolutionized diabetes care. Originally designed strictly for glucose control, these medications have emerged as powerful tools for weight management, changing the paradigm of how type 2 diabetes is treated, particularly in patients with obesity.
Prominent Options and Mechanisms
Leading medications in this class include Semaglutide (marketed as Ozempic for diabetes) and the newer dual-agonist Tirzepatide (Mounjaro), which mimics both GLP-1 and GIP hormones. These drugs function by mimicking the natural incretin hormones released by the gut after eating. They perform three critical functions:
1. Stimulating the pancreas to release insulin when blood sugar is high.
2. Suppressing glucagon secretion (which signals the liver to release stored sugar).
3. Slowing gastric emptying, which creates a prolonged feeling of fullness.
Dual Benefits: Glycemic Control and Weight Loss
GLP-1 receptor agonists are frequently cited as the “best” option for patients who need to lose significant weight to manage their condition. Clinical trials have demonstrated that medications like Tirzepatide can lead to substantial reductions in body weight—sometimes exceeding 15%—which directly improves insulin sensitivity. Furthermore, these medications are highly effective at lowering A1C levels, often outperforming oral medications. Due to their potent efficacy, they are increasingly prescribed as a second-line treatment immediately following, or sometimes in place of, Metformin for eligible patients.
SGLT2 Inhibitors: For Heart and Kidney Health

Sodium-Glucose Cotransporter-2 (SGLT2) inhibitors represents a distinct class of medication that manages blood sugar through the renal system rather than the pancreas or liver. Options such as Empagliflozin (Jardiance) and Dapagliflozin (Farxiga) have become vital in treating patients with specific comorbidities.
Mechanism of Action
These medications work by inhibiting the reabsorption of glucose in the kidneys. Instead of the sugar returning to the bloodstream, it is excreted from the body through urine. This unique mechanism lowers blood glucose levels independently of insulin, meaning it carries a very low risk of hypoglycemia.
Cardiovascular and Renal Protection
SGLT2 inhibitors are widely considered the “best” specific choice for patients with established cardiovascular disease, heart failure, or chronic kidney disease (CKD), regardless of their A1C levels. Clinical studies have shown that these drugs:
Significantly reduce the risk of hospitalization for heart failure.
Slow the progression of kidney disease, delaying the need for dialysis.
Lower blood pressure and induce modest weight loss due to the excretion of calories via urine.
For a patient with type 2 diabetes who has a history of heart issues, an SGLT2 inhibitor is often prioritized in the treatment regimen, sometimes even before considering glycemic targets.
DPP-4 Inhibitors and Sulfonylureas
While Metformin, GLP-1s, and SGLT2s dominate current guidelines, other oral medications remain important tools, particularly when cost or tolerance issues arise.
DPP-4 Inhibitors (The Gentle Alternative)
Medications like Sitagliptin (Januvia) act by blocking the enzyme DPP-4, which destroys incretin hormones. By preserving these hormones, the body can produce more insulin when needed.
* Best For: Patients who cannot tolerate Metformin due to gastrointestinal issues or those who need a well-tolerated add-on therapy.
* Pros: They are weight-neutral, come in pill form, and have very few side effects.
* Cons: They are generally less potent at lowering A1C compared to GLP-1 agonists or Metformin.
Sulfonylureas (The Traditional Option)
Drugs such as Glipizide and Glimepiride have been used for decades. They work by directly stimulating the beta cells in the pancreas to release more insulin.
* Best For: Patients who require an extremely low-cost medication to rapidly lower blood sugar.
* Risks: Because they squeeze insulin out of the pancreas regardless of glucose levels, they carry a higher risk of hypoglycemia and can cause weight gain. Consequently, they have largely been relegated to third-line therapy in modern treatment algorithms.
Insulin Therapy Options
Despite the efficacy of newer drugs, insulin remains a critical and life-saving component of type 2 diabetes treatment. Diabetes is a progressive condition; over time, the body’s beta cells may lose the ability to produce sufficient insulin, making replacement therapy necessary.
When Insulin is the Best Choice
Insulin is typically introduced when oral medications and non-insulin injectables (like GLP-1s) fail to keep A1C levels within target range, or when a patient presents with extremely high blood sugar levels (severe hyperglycemia) and symptoms of catabolism (unexplained weight loss).
Basal vs. Mealtime Insulin
* Basal Insulin: Long-acting formulations (such as Lantus, Levemir, or Tresiba) provide a steady background level of insulin to control fasting blood sugar. This is often the first step in insulin therapy, involving just one injection a day.
* Rapid-Acting (Mealtime) Insulin: As the disease progresses, patients may need “bolus” insulin (such as Humalog or Novolog) taken before meals to manage post-prandial glucose spikes.
Modern insulin analogs are designed to mimic the body’s natural release patterns more closely than older human insulins, reducing the risk of overnight lows.
How Doctors Determine the Best Choice for You
Prescribing the “best” medication is no longer a one-size-fits-all process. Physicians now utilize a patient-centered approach guided by the American Diabetes Association’s Standards of Care.
Critical Decision Factors
Doctors evaluate several key pillars when selecting a regimen:
1. Cardiovascular and Renal Risk: If a patient has heart failure or kidney disease, SGLT2 inhibitors are the priority. If atherosclerotic cardiovascular disease is the concern, GLP-1 agonists are often favored.
2. Weight Management Needs: For patients with a high Body Mass Index (BMI), GLP-1 agonists and dual agonists (like Tirzepatide) are preferred due to their superior weight-loss efficacy.
3. A1C Levels: The distance between a patient’s current A1C and their goal determines the potency required. A patient with an A1C of 9.0% may need combination therapy immediately, whereas someone at 7.0% might succeed with lifestyle changes and Metformin alone.
Practical Considerations
Beyond clinical data, practical elements dictate the choice:
* Cost and Coverage: Newer drugs (GLP-1s and SGLT2s) can be expensive. Physicians must navigate insurance formularies to find covered options.
* Route of Administration: Some patients have a phobia of needles, making oral options like Metformin, SGLT2 inhibitors, or oral Semaglutide (Rybelsus) preferable to injectables.
Finding the right medication is a personalized journey that may involve combining therapies to reach your glucose goals. While Metformin is the standard starting point, the rise of medications that offer heart protection and weight management has expanded the definition of the “best” treatment. What works best for one patient may be entirely different for another based on their unique physiology and lifestyle. Consult with your healthcare provider to review your blood work and medical history to select the regimen that offers the most protection for your long-term health.
Frequently Asked Questions
What is considered the first-line medication for treating type 2 diabetes?
Metformin is widely considered the gold standard and is almost always the first medication prescribed for type 2 diabetes due to its proven safety, low cost, and effectiveness. It works by reducing the amount of sugar your liver releases and improving how your body responds to insulin without causing weight gain. Most doctors start patients on Metformin unless there are specific medical reasons, such as severe kidney issues, that prevent its use.
Which type 2 diabetes medications are best for helping with weight loss?
GLP-1 receptor agonists, such as semaglutide (Ozempic) and tirzepatide (Mounjaro), are currently the most effective diabetes medications for inducing weight loss while controlling blood sugar. These injectable drugs mimic natural hormones that slow digestion and signal fullness to the brain, leading to significant appetite reduction. While SGLT2 inhibitors (like Jardiance) also promote modest weight loss, GLP-1s typically produce the most dramatic results.
How do SGLT2 inhibitors compare to other diabetes treatments?
SGLT2 inhibitors, such as Farxiga and Jardiance, are unique because they lower blood sugar by helping the kidneys filter excess glucose out of the body through urine. They are often the best choice for patients who have heart failure or chronic kidney disease, as they offer protective cardiovascular and renal benefits that other drug classes do not. Unlike insulin or sulfonylureas, SGLT2 inhibitors carry a very low risk of causing hypoglycemia (low blood sugar).
What is the most effective medication for lowering A1C levels quickly?
While insulin remains the most potent agent for rapidly bringing down extremely high blood sugar levels, tirzepatide (Mounjaro) has shown the highest efficacy among non-insulin medications for lowering A1C in clinical trials. By targeting both GIP and GLP-1 receptors, it delivers a dual-action approach that drastically improves glycemic control. However, the “best” choice varies by patient, and doctors will assess current A1C levels before recommending high-potency injectables versus oral medications.
What are the best alternatives if I cannot tolerate Metformin side effects?
If you experience severe gastrointestinal issues with Metformin, doctors often prescribe “extended-release” versions to mitigate symptoms or switch to SGLT2 inhibitors or DPP-4 inhibitors (like Januvia). DPP-4 inhibitors are oral medications that are generally weight-neutral and well-tolerated by patients with sensitive stomachs. It is crucial to consult your healthcare provider to find an alternative that manages glucose effectively without impacting your quality of life.
References
- Type 2 diabetes – Diagnosis and treatment – Mayo Clinic
- Insulin, Medicines, & Other Diabetes Treatments – NIDDK
- https://www.nhs.uk/conditions/type-2-diabetes/medicine/
- What Are My Options for Type 2 Diabetes Medications? | ADA
- https://my.clevelandclinic.org/health/treatments/13902-type-2-diabetes-treatment
- Type 2 diabetes: Which medication is best for me? – Harvard Health
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes/type-2-diabetes-treatment