The “best” medicine for Type 2 Diabetes is not a one-size-fits-all solution; instead, it’s a personalized treatment plan developed with your healthcare provider. While Metformin is often the initial and cornerstone therapy, a range of advanced medications exists today, offering diverse mechanisms to manage blood sugar, protect vital organs, and improve overall health. This guide explores the current leading options to help you understand your choices and why a tailored approach is crucial for effective Type 2 Diabetes management.
The Foundation: Metformin as First-Line Therapy

Metformin stands as the undisputed champion for initial Type 2 Diabetes management, and for good reason. It’s often the first medication prescribed, not just because it’s effective and well-understood, but also because it addresses some of the core issues of Type 2 Diabetes with a favorable safety profile.
* Core Action: Metformin works primarily by reducing glucose production by the liver and improving insulin sensitivity in muscle cells. Think of your liver as a sugar factory; Metformin essentially tells it to slow down production, especially at night. At the same time, it helps your body’s cells, particularly those in your muscles, become more responsive to the insulin you do produce, allowing them to absorb glucose more efficiently from your bloodstream. This dual action is incredibly effective at lowering blood sugar levels without overstimulating insulin production.
* Key Benefits: It’s often the first-line medication due to its proven efficacy in lowering A1c, its generally safe profile, and a very low risk of causing hypoglycemia ( dangerously low blood sugar), which is a common concern with some other diabetes medications. Beyond blood sugar control, Metformin has also been associated with potential cardiovascular benefits, like reducing the risk of heart disease in some individuals, and can even contribute to modest weight loss or at least be weight-neutral, which is a significant advantage for many. It’s also widely available and relatively inexpensive, making it accessible to a broad range of patients.
* Considerations: Like any medication, Metformin isn’t without its potential drawbacks. The most common side effects are gastrointestinal issues such as nausea, diarrhea, stomach upset, or gas, especially when you first start taking it. These often improve over time or can be minimized by taking Metformin with meals and gradually increasing the dose. It’s also not suitable for everyone, particularly those with severe kidney disease, as it can accumulate in the body and potentially cause lactic acidosis, a rare but serious condition. Your doctor will always check your kidney function before starting Metformin and monitor it regularly.
Expanding Oral Options: SGLT2 Inhibitors & DPP-4 Inhibitors
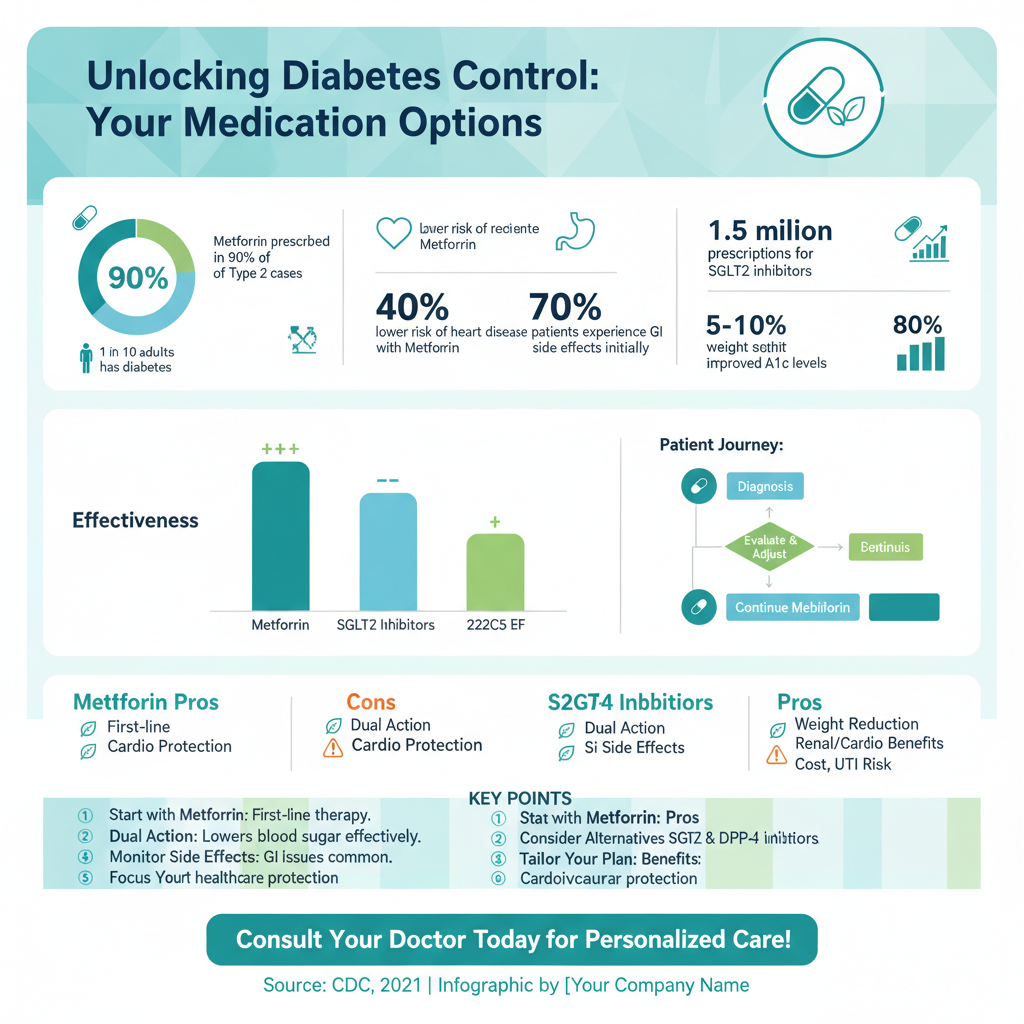

Once Metformin is in place, or if it’s not suitable, your healthcare provider might consider other powerful oral medications. Two classes, SGLT2 inhibitors and DPP-4 inhibitors, have become increasingly prominent, each with unique benefits and patient profiles.
* SGLT2 Inhibitors (e.g., empagliflozin, canagliflozin, dapagliflozin): These medications represent a significant leap forward in diabetes care, offering benefits far beyond just blood sugar control. They work by blocking a protein in your kidneys called SGLT2 (Sodium-Glucose Co-Transporter 2). Normally, your kidneys reabsorb most of the glucose from your urine back into your bloodstream. SGLT2 inhibitors disrupt this process, causing excess glucose to be excreted in your urine, effectively lowering blood sugar. But here’s the exciting part: these drugs offer significant cardiovascular and kidney protection. They’ve been shown to reduce the risk of heart attack, stroke, hospitalization for heart failure, and slow the progression of chronic kidney disease in people with Type 2 Diabetes, even those without pre-existing heart or kidney conditions. Common side effects can include urinary tract infections or yeast infections due to the increased sugar in the urine.
* DPP-4 Inhibitors (e.g., sitagliptin, linagliptin, saxagliptin): If SGLT2 inhibitors are the “sugar flushers,” DPP-4 inhibitors are the “hormone helpers.” They work by increasing the levels of natural incretin hormones (like GLP-1 and GIP) in your body. These hormones are released after you eat and signal your pancreas to produce more insulin when blood sugar levels are high, and to reduce the amount of glucose produced by the liver. The beauty of DPP-4 inhibitors is that this action is glucose-dependent, meaning they primarily work when blood sugar is elevated, which helps reduce the risk of hypoglycemia. They are generally well-tolerated, cause little to no weight gain, and have a neutral effect on cardiovascular outcomes.
* Patient Profile: SGLT2 inhibitors are increasingly favored and often recommended as a second-line therapy for patients who have established cardiovascular disease (like a history of heart attack or stroke) or chronic kidney disease, due to their profound protective benefits for these vital organs. They can also be a good choice for individuals needing weight loss. DPP-4 inhibitors, on the other hand, are often chosen for patients who need milder blood sugar control, prioritize a low side effect profile (especially avoiding GI issues or potential for genital infections), or those for whom weight neutrality is important. They are a good option for people who need effective blood sugar lowering with minimal fuss.
Powerful Injectables: GLP-1 Receptor Agonists

When oral medications alone aren’t quite enough, or if specific additional benefits are desired, GLP-1 receptor agonists often step into the spotlight. These powerful injectables have revolutionized diabetes care, offering significant benefits beyond just blood sugar control.
* Mechanism: GLP-1 receptor agonists (like semaglutide, liraglutide, dulaglutide, and tirzepatide) mimic a natural gut hormone called Glucagon-Like Peptide-1 (GLP-1). This hormone plays several crucial roles: it stimulates the pancreas to release more insulin when blood sugar levels are high, suppresses the release of glucagon (a hormone that raises blood sugar), slows down gastric emptying (which helps you feel full longer and prevents sharp blood sugar spikes after meals), and acts on the brain to reduce appetite and promote satiety. This multi-pronged approach makes them incredibly effective.
* Major Advantages: The benefits of GLP-1 receptor agonists are truly impressive. They are highly effective in lowering blood sugar (A1c reduction can be substantial), and many patients experience significant weight loss, which is a major advantage for individuals with Type 2 Diabetes who often struggle with excess weight. Furthermore, several GLP-1 receptor agonists have shown proven cardiovascular benefits, reducing the risk of major adverse cardiovascular events like heart attack and stroke, similar to SGLT2 inhibitors. Some, like tirzepatide, are even more potent, acting on both GLP-1 and GIP receptors, leading to even greater A1c and weight reductions.
* Administration: While they are powerful, one consideration is their administration: they are given via subcutaneous injection, meaning just under the skin. Depending on the specific medication, this might be a daily injection or a convenient weekly injection. While the idea of injections can be daunting for some, the needles are very fine, and the process is usually quick and relatively painless. Common side effects include gastrointestinal issues like nausea (especially when starting), vomiting, or diarrhea, but these often lessen over time as your body adjusts to the medication.
When Insulin Therapy Becomes Necessary
Despite the many advances in oral medications and GLP-1 receptor agonists, for some individuals, insulin therapy remains a vital and often necessary part of managing Type 2 Diabetes. It’s important to understand that needing insulin is not a sign of failure, but rather a progression of the disease or a vital tool to achieve optimal blood sugar control.
* Indications: Insulin is typically introduced when other medications, including oral therapies and GLP-1 agonists, are no longer sufficient to achieve target blood glucose levels. This often happens as Type 2 Diabetes progresses over time and the pancreas becomes less capable of producing enough insulin on its own. It may also be used temporarily in situations like severe illness, surgery, or pregnancy, or in cases of severe insulin deficiency from the outset of diagnosis.
* Types of Insulin: Insulin regimens are highly individualized. The two main types often used in Type 2 Diabetes are:
* Basal insulin (long-acting or intermediate-acting): This provides continuous background coverage to keep blood sugar levels stable between meals and overnight. It mimics the small, steady amount of insulin your body naturally produces. Examples include insulin glargine or insulin detemir.
* Prandial (bolus or short-acting) insulin: This type is taken before meals to cover the carbohydrate intake and manage the rise in blood sugar that occurs after eating. Examples include insulin lispro or insulin aspart. Some people may use a combination of both to mimic the body’s natural insulin release more closely.
* Management: Insulin therapy requires careful monitoring of blood sugar levels, often multiple times a day, to adjust doses and prevent hypoglycemia. While the potential for hypoglycemia is a consideration, modern insulins are designed to be more predictable, and advanced delivery devices like insulin pens and continuous glucose monitors (CGMs) have made managing insulin much easier and safer. Your healthcare team will work closely with you to teach you how to administer insulin, monitor your levels, and adjust your doses based on your lifestyle and blood sugar readings, empowering you to take control.
Beyond Blood Sugar: Addressing Co-morbidities
Modern Type 2 Diabetes management has evolved significantly. It’s no longer just about lowering blood sugar; it’s about a comprehensive strategy that protects your entire body and addresses the common co-morbidities that often accompany diabetes. This holistic approach is key to improving long-term health and quality of life.
* Cardiovascular Protection: Heart disease is the leading cause of death for people with diabetes. Excitingly, several newer medications, specifically SGLT2 inhibitors and GLP-1 receptor agonists, offer significant benefits for heart health. They have been shown to reduce the risk of major cardiovascular events like heart attack and stroke, and critically, reduce the risk of hospitalization for heart failure. This means your diabetes medication can pull double duty, managing your blood sugar while actively protecting your heart, which is a game-changer in diabetes care.
* Kidney Health: Diabetic kidney disease (nephropathy) is another common and serious complication. Here again, SGLT2 inhibitors have shown remarkable benefits. They can significantly slow the progression of diabetic kidney disease, reducing the risk of kidney failure and the need for dialysis. This kidney-protective effect is independent of their blood sugar-lowering ability, making them invaluable for patients at risk of or already experiencing kidney complications. Managing blood pressure and cholesterol also plays a crucial role in preserving kidney function.
* Holistic Approach: A truly effective treatment strategy for Type 2 Diabetes extends beyond just glucose control. It actively focuses on managing weight, blood pressure, and cholesterol levels, which are all interconnected with diabetes and overall cardiovascular health. Your healthcare provider will likely discuss a plan that integrates medication with lifestyle changes like diet and exercise. The goal is not just to prevent immediate complications but to protect vital organs, reduce long-term risks, and ultimately, improve your overall health and well-being, helping you live a full and vibrant life.
Personalizing Your Treatment Plan
Navigating the array of diabetes medications can seem complex, but that’s where the personalization aspect comes in. The “best” plan is the one uniquely tailored to you, your body, and your life. It’s a collaborative journey with your healthcare provider.
* Individual Factors: The “best” medication choice is deeply personal and depends on a multitude of individual factors. Your doctor will consider your age, your current weight, the health of your kidneys and liver, your cardiovascular history (whether you’ve had a heart attack or stroke), and your overall lifestyle. For instance, if you have established heart disease, an SGLT2 inhibitor or GLP-1 agonist might be prioritized for their organ-protective benefits. If weight loss is a key goal, a GLP-1 agonist could be an excellent fit. Your current blood sugar levels and how long you’ve had diabetes also play a role in determining the intensity and type of therapy needed.
* Shared Decision-Making: This is where you come in! Open and honest communication with your doctor is absolutely crucial. You should feel comfortable discussing your preferences, potential concerns about side effects, the convenience of different administration methods (e.g., daily pills vs. weekly injections), and your ability to adhere to a specific regimen. For example, if you travel frequently, a weekly injection might be more convenient than a daily pill or vice-versa. Your doctor will explain the pros and cons of each option, empowering you to make informed decisions that align with your values and lifestyle.
* Evolving Care: It’s important to remember that your treatment plan isn’t set in stone. Type 2 Diabetes is a progressive condition, and your needs may change over time. What works today might need adjustment a few years down the line. Your treatment plan is dynamic and often evolves as the disease progresses, as new health goals emerge (like losing more weight), or as new medications become available that offer even better benefits. Regular check-ups with your healthcare team are essential to continuously review your progress, address any new challenges, and adjust your treatment to ensure you’re always on the optimal path.
Understanding the array of medications available for Type 2 Diabetes empowers you to have informed discussions with your doctor. From foundational Metformin to advanced injectables and insulin, each option plays a crucial role in managing the condition and preventing complications. Remember, the ultimate goal is a personalized plan that fits your health profile and lifestyle, focusing not only on blood sugar control but also on protecting your heart and kidneys. Always consult with your healthcare provider to determine the best course of treatment for you, continuously reviewing and adjusting as needed to achieve optimal health outcomes and a better quality of life.
Frequently Asked Questions
What is generally considered the first-line medicine for type 2 diabetes?
Metformin is widely recognized as the initial and often the most effective first-line medication for managing type 2 diabetes. It works by decreasing glucose production by the liver and improving the body’s sensitivity to insulin, which helps lower blood sugar levels. Doctors typically prescribe metformin alongside lifestyle changes, making it a foundational treatment for many newly diagnosed patients with type 2 diabetes.
Which newer medications for type 2 diabetes offer benefits beyond blood sugar control, like weight loss or cardiovascular protection?
Newer classes of type 2 diabetes medications, such as GLP-1 receptor agonists (e.g., Ozempic, Trulicity) and SGLT2 inhibitors (e.g., Farxiga, Jardiance), offer significant advantages beyond just lowering blood sugar. These advanced medicines have been shown to provide cardiovascular and renal benefits, reducing the risk of heart attack, stroke, and kidney disease progression. Many also promote weight loss, making them a preferred choice for comprehensive type 2 diabetes management in eligible patients.
Why might a doctor prescribe insulin for type 2 diabetes, and is it always necessary?
A doctor might prescribe insulin for type 2 diabetes when oral medications or other injectables are no longer sufficient to control blood sugar levels, or if blood glucose is extremely high at diagnosis. Insulin helps the body utilize glucose for energy, preventing complications from chronic hyperglycemia. While not always necessary initially, insulin can become a vital component of type 2 diabetes treatment as the disease progresses and the pancreas’s ability to produce its own insulin diminishes.
How do doctors determine the best medicine or combination of medicines for an individual with type 2 diabetes?
Doctors determine the best medicine for type 2 diabetes by considering a patient’s individual factors, including their A1c level, co-existing conditions (like heart or kidney disease), weight, potential medication side effects, and cost. The ideal treatment plan is highly personalized, often involving a combination of different drug classes to achieve optimal blood sugar control and protect against complications. This tailored approach ensures the most effective and safest type 2 diabetes medications are used.
What are common side effects patients should be aware of when starting new type 2 diabetes medications?
Common side effects vary among type 2 diabetes medications, but patients should be aware of potential issues such as gastrointestinal upset (nausea, diarrhea, stomach pain) frequently associated with metformin and GLP-1 receptor agonists. There’s also a risk of hypoglycemia (low blood sugar), especially with insulin or sulfonylureas, which can cause dizziness, sweating, and confusion. It’s crucial for patients to discuss all possible side effects with their healthcare provider and understand how to manage them to ensure safe and effective use of their type 2 diabetes medicines.
References
- https://diabetes.org/healthy-living/medication-treatments/type-2-diabetes-medication
- https://www.niddk.nih.gov/health-information/diabetes/overview/type-2-diabetes/treatment
- Type 2 diabetes – Diagnosis and treatment – Mayo Clinic
- https://www.cdc.gov/diabetes/basics/type2.html
- https://en.wikipedia.org/wiki/Type_2_diabetes_management
- https://www.health.harvard.edu/blog/new-drugs-for-type-2-diabetes-202303032900
- Treatment for type 2 diabetes – NHS