For most people with Type 2 diabetes, Metformin is considered the best first-line medicine due to its effectiveness, safety profile, and low cost. However, for Type 1 diabetes, insulin is the necessary treatment, and for patients seeking weight management alongside blood sugar control, newer GLP-1 agonists like Semaglutide are often the top choice. This guide breaks down the most effective medications available today to help you understand your options before consulting your doctor.
Navigating a diabetes diagnosis can feel like learning a new language. With so many commercials, news headlines, and medical opinions floating around, it is easy to feel overwhelmed. Are injectables better than pills? Is insulin always the last resort? The truth is, the landscape of diabetes management has changed drastically in the last decade. We have moved from simply trying to lower blood sugar numbers to a more holistic approach that protects your heart, kidneys, and waistline. Whether you are newly diagnosed or looking to switch up your current regimen, understanding the “why” and “how” behind these medications empowers you to have better conversations with your healthcare team.
Metformin: The Gold Standard for Type 2

If you have recently been diagnosed with Type 2 diabetes, chances are high that the first prescription you received was for Metformin. It has held the title of “first-line therapy” for decades, and for very good reason. Unlike some other medications that force your body to squeeze out more insulin, Metformin works a bit more subtly and smartly. Its primary job is to lower the amount of glucose (sugar) your liver produces. At the same time, it increases your muscle sensitivity to insulin, meaning your body can use the insulin it already has much more effectively.
The benefits of Metformin go beyond just blood sugar control. First and foremost, it is incredibly affordable. In a world where medication costs are skyrocketing, Metformin remains accessible to almost everyone. Secondly, it has a very high safety profile regarding hypoglycemia. Because it doesn’t stimulate the pancreas to produce more insulin, it rarely causes your blood sugar to drop dangerously low—a common fear for many patients. There is also some evidence suggesting it may have anti-aging and anti-cancer properties, though research is still ongoing in those areas.
Of course, no medication is without its quirks. The most common complaint with Metformin involves the digestive system. Many people experience nausea, bloating, or diarrhea when they first start taking it. The friendly advice here is to start low and go slow. Doctors usually prescribe a low dose to let your body adjust before increasing it. Additionally, asking for the “Extended Release” (ER) version can significantly reduce these tummy troubles. Taking the pill with a large meal also helps cushion the impact, allowing you to reap the benefits without the discomfort.
GLP-1 Agonists (Injectables and Oral)
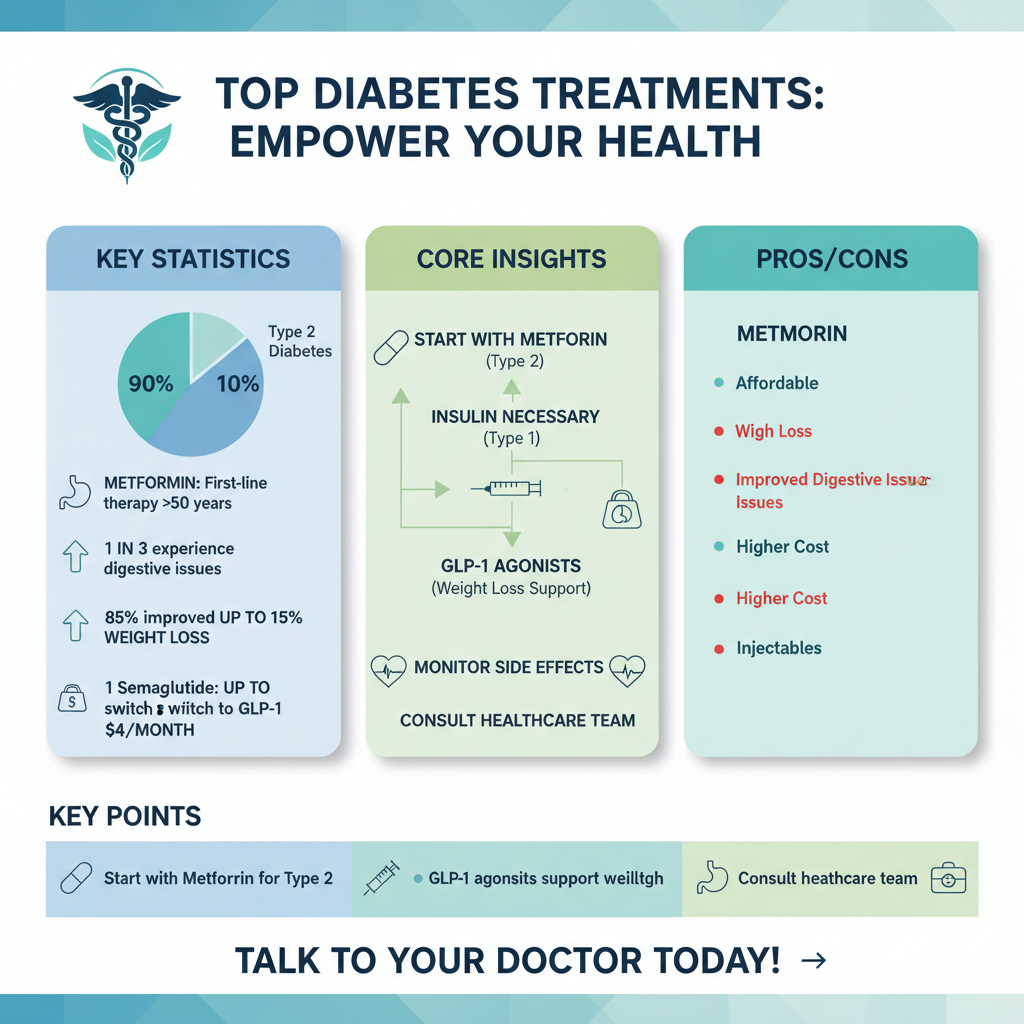

You have probably heard the buzz surrounding drugs like Ozempic, Trulicity, or Rybelsus. These belong to a class of drugs called GLP-1 receptor agonists, and they have truly revolutionized diabetes care. GLP-1 is a hormone naturally found in your intestines. These medications mimic that hormone to tell your pancreas to release insulin when your blood sugar is high. They also stop the liver from making too much sugar and slow down digestion, so you feel full longer.
That last point—feeling full longer—is where the dual benefit comes in. GLP-1 agonists have shown remarkable results in helping patients lose weight. For many people with Type 2 diabetes, weight management is a constant struggle that directly impacts their blood sugar control. By curbing appetite and quieting “food noise,” these drugs help tackle the root cause of insulin resistance for many. Beyond the scale, these medications offer profound cardiovascular protection, reducing the risk of heart attack and stroke in people with established heart disease.
While most of these are weekly injections (which are surprisingly painless thanks to modern pen needles), there are oral options like Rybelsus for those who prefer pills. However, they are potent drugs, and the body takes time to get used to them. The most common side effects are gastrointestinal—nausea and sometimes vomiting. The key to managing this is eating smaller, slower meals and avoiding high-fat foods, which can make the side effects worse. While the adjustment period can be tough for some, the long-term benefits for the heart and waistline often make it a top contender for the “best” medicine title.
SGLT2 Inhibitors: Protecting Heart and Kidneys

If GLP-1s are the stars of weight loss, SGLT2 inhibitors (like Jardiance, Farxiga, and Invokana) are the unsung heroes of heart and kidney protection. These oral medications work on a completely different mechanism than other diabetes drugs. Rather than messing with insulin, they work on the kidneys. Normally, your kidneys filter sugar out of your blood and then reabsorb it back into the body. SGLT2 inhibitors block that reabsorption, allowing your body to expel excess sugar through your urine. Think of it as a safety valve that releases sugar when levels get too high.
This mechanism does more than just lower A1C; it physically reduces the stress on the cardiovascular system and the kidneys. Today, these drugs are often the preferred choice for diabetic patients who also have heart failure or Chronic Kidney Disease (CKD). Clinical trials have shown that they can significantly slow the progression of kidney disease and reduce hospitalizations for heart failure. For a patient dealing with these specific comorbidities, an SGLT2 inhibitor isn’t just a diabetes drug; it’s a life-preserving therapy.
There are some specific considerations to keep in mind, however. Because the drug pushes sugar into the urine, it creates an environment where bacteria and yeast love to grow. This leads to a slightly higher risk of urinary tract infections (UTIs) and yeast infections (in both men and women). The best way to mitigate this risk is through excellent hygiene and, most importantly, hydration. Since the medication acts somewhat like a diuretic, you will need to drink plenty of water throughout the day to stay hydrated and keep your system flushed.
Insulin Therapy Options
There is a common misconception that starting insulin means you have “failed” at managing your diabetes. We need to erase that stigma. For people with Type 1 diabetes, insulin is a non-negotiable, life-sustaining necessity because their pancreas produces little to no insulin. for those with Type 2, diabetes is a progressive condition. Over years or decades, the pancreas may simply get tired and produce less insulin. In these cases, insulin therapy is the most natural and effective way to replace what the body is missing.
Insulin therapy generally falls into two categories: long-acting (basal) and rapid-acting (bolus). Long-acting insulin, like Lantus or Tresiba, works in the background for 24 hours to keep your baseline sugar steady. Rapid-acting insulin, like Humalog or Novolog, is taken right before meals to handle the spike in sugar from food. Many Type 2 patients find great success just adding a single shot of long-acting insulin to their daily oral regimen, which provides just enough support to bring A1C levels back into range without the complexity of mealtime dosing.
The quality of life for insulin users has improved dramatically thanks to technology. The days of vials and syringes are largely behind us, replaced by discreet, easy-to-use insulin pens. For even more freedom, insulin pumps and “smart pens” can communicate directly with Continuous Glucose Monitors (CGMs), creating a loop that automates much of the decision-making. These advancements make insulin therapy far less intrusive than it used to be, allowing patients to live flexible, active lives while maintaining excellent control.
DPP-4 Inhibitors and Sulfonylureas
While Metformin, GLP-1s, and SGLT2s get the most attention, there are other oral medications that play a vital role in treatment plans. DPP-4 inhibitors (like Januvia or Tradjenta) and Sulfonylureas (like Glipizide or Glimepiride) are often prescribed when Metformin isn’t enough, or if a patient cannot tolerate the side effects of other drugs.
DPP-4 inhibitors are known for being very well-tolerated. They work by helping the body make more insulin only when it is needed and reducing the amount of glucose being produced by the liver when it is not needed. They are “weight neutral,” meaning they won’t cause weight gain, and they rarely cause low blood sugar. They are often a great middle-ground choice for patients who need a little extra help without aggressive side effects.
Sulfonylureas are among the oldest diabetes drugs, and they work by stimulating the pancreas to release more insulin all day long. Their biggest advantage is cost—they are incredibly cheap. However, because they squeeze the pancreas to release insulin regardless of whether you have eaten, they carry a higher risk of hypoglycemia (low blood sugar) and can sometimes cause weight gain. Despite this, for patients on a strict budget, they remain a potent and effective tool when used carefully with regular meals.
Factors in Choosing the Best Medicine
So, with all these options, how do you and your doctor decide which one is the “best” for you? It is rarely a random choice. Doctors look at a variety of factors, starting with your A1C levels. If your numbers are extremely high, they might suggest starting with insulin or a combination of drugs to bring levels down quickly. If your numbers are just slightly above target, lifestyle changes plus Metformin might be the plan.
Your other health conditions play a massive role in this decision. If you have heart disease, a GLP-1 agonist or SGLT2 inhibitor is now the standard of care, regardless of your A1C, because of the heart-protective benefits. If weight loss is a primary goal, the GLP-1 route is favored. Conversely, if cost is a major barrier—which is a very real reality for many—older drugs like Sulfonylureas and Metformin can provide effective control for pennies a day compared to the hundreds of dollars that newer branded drugs might cost without insurance coverage.
Finally, your lifestyle matters. Are you comfortable giving yourself an injection? If you have an unpredictable schedule where you might skip meals, drugs that cause low blood sugar (like Sulfonylureas) might be dangerous. The best medication is the one you will actually take consistently. It is vital to look at medication not as a magic cure, but as a partner to diet and exercise. No drug can completely outwork a poor diet, but the right drug can make your healthy efforts pay off significantly more.
Finding the “best” medicine is a personalized journey that depends entirely on your specific diagnosis, A1C goals, and underlying health conditions. While Metformin remains the standard starting point for Type 2 diabetes, newer classes of drugs offer additional benefits for heart health and weight loss. Always discuss these options with your healthcare provider to create a treatment plan tailored to your body’s needs. By understanding the tools in your toolkit, you can take charge of your health and live a full, vibrant life with diabetes.
Frequently Asked Questions
What is the best first-line medication for Type 2 diabetes?
Most healthcare providers and guidelines recommend Metformin as the first medication for managing Type 2 diabetes because it is effective, affordable, and safe for most people. It works by reducing the amount of sugar your liver releases and improving your body’s sensitivity to insulin. However, doctors may prescribe alternative medicines if a patient has specific kidney issues or experiences severe gastrointestinal side effects.
Which diabetes medications help with weight loss?
GLP-1 receptor agonists, such as semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro), are widely considered the best diabetes medications for promoting weight loss. These injectable drugs mimic hormones that regulate appetite, helping patients feel full longer and reducing overall calorie intake while lowering blood sugar levels. Because of their dual benefits, they are increasingly prescribed for patients battling both obesity and Type 2 diabetes.
Are there diabetes medicines that protect the heart and kidneys?
Yes, two specific classes of drugs—SGLT2 inhibitors (like Jardiance and Farxiga) and GLP-1 receptor agonists—are proven to offer significant protection for the heart and kidneys. SGLT2 inhibitors help the kidneys remove sugar through urine and are highly effective at reducing the risk of heart failure and kidney disease progression. Doctors often prioritize these medications for diabetic patients who have existing cardiovascular conditions or chronic kidney disease.
How do I know if I need insulin or just oral medication?
Doctors typically prescribe oral medications like Metformin first, but insulin may become necessary if pills and lifestyle changes fail to keep your Hemoglobin A1C levels within a healthy target range. Because Type 2 diabetes is a progressive condition, the pancreas may eventually stop producing enough insulin on its own, making insulin therapy the best option for preventing hyperglycemia. Regular blood work and monitoring will help your healthcare provider determine when a transition to insulin is required.
What are the common side effects of popular diabetes medications?
The side effects vary by drug class; for example, Metformin frequently causes digestive issues like nausea or diarrhea, which often improve by taking the pill with food or switching to an extended-release version. GLP-1 agonists may cause nausea and vomiting, while SGLT2 inhibitors can increase the risk of yeast infections and dehydration due to increased urination. It is crucial to discuss these potential reactions with your doctor to find the best medicine that balances blood sugar control with your quality of life.
References
- Insulin, Medicines, & Other Diabetes Treatments – NIDDK
- Type 2 diabetes – Diagnosis and treatment – Mayo Clinic
- Diabetes & Oral Medication: Types & How They Work
- https://www.nhs.uk/conditions/type-2-diabetes/medicine/
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes/diabetes-medicines
- Type 2 diabetes: Which medication is best for me? – Harvard Health
- Diabetes management
- https://diabetes.org/health-wellness/medication