Managing gestational diabetes effectively relies heavily on making smart food choices to keep blood sugar levels stable, which is crucial for both maternal and fetal health. The best foods to focus on include complex carbohydrates, lean proteins, healthy fats, and an abundance of non-starchy vegetables, as these help slow glucose absorption, provide sustained energy, and deliver vital nutrients without causing spikes in blood sugar. By understanding how different foods impact your blood sugar, you can make informed decisions that support a healthy pregnancy and minimize complications.
Understanding Your Gestational Diabetes Diet

Gestational diabetes (GD) is a unique condition that arises during pregnancy when your body struggles to produce or effectively use enough insulin. Insulin is a vital hormone responsible for converting glucose (sugar) from the food you eat into energy for your cells. During pregnancy, hormonal changes can make your cells more resistant to insulin, meaning your pancreas has to work extra hard to keep up. If it can’t produce enough additional insulin, blood sugar levels rise, leading to GD. This condition typically appears in the second or third trimester and usually resolves after birth, but it’s critical to manage it carefully for the health of both you and your baby.
The cornerstone of managing gestational diabetes is dietary management. While some women may eventually need medication or insulin, a well-planned diet is often the first and most effective line of defense against high blood glucose levels. This dietary approach isn’t about deprivation; rather, it’s about making smart, informed food choices that support your body’s unique needs during pregnancy.
The primary goal of your gestational diabetes diet is twofold: first, to prevent sudden and significant spikes in blood sugar, which can be harmful to both mother and baby. Uncontrolled high blood sugar can increase risks such as pre-eclampsia, preterm birth, and a larger-than-average baby (macrosomia), which can complicate delivery. Second, your diet must ensure optimal nutrition, providing all the essential vitamins, minerals, and energy necessary for your baby’s healthy growth and development, as well as maintaining your own well-being throughout pregnancy. It’s a delicate balance, but one that is entirely achievable with the right knowledge and guidance.
Smart Carbohydrate Choices for Stable Energy
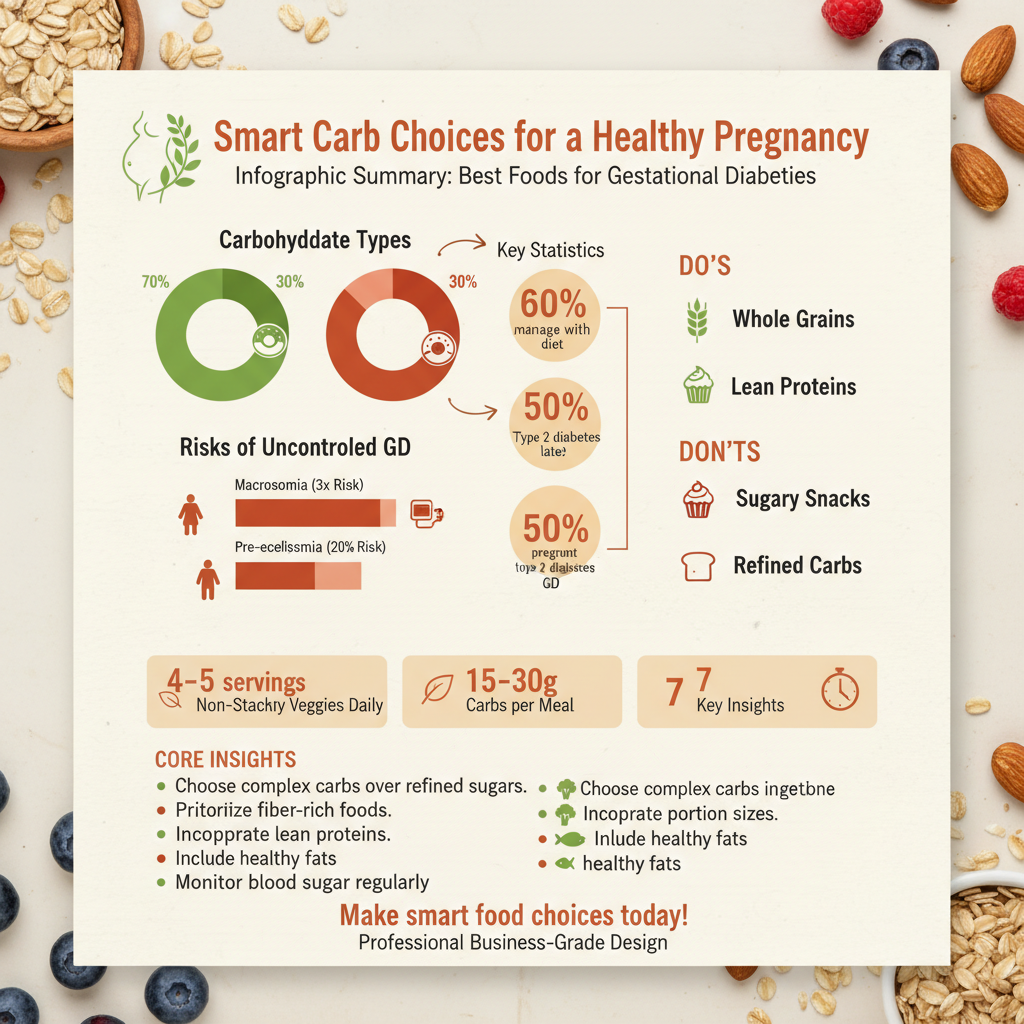

Carbohydrates are an essential part of your diet, providing the primary source of energy for both you and your growing baby. However, for those with gestational diabetes, the type and portion size of carbohydrates are paramount. Instead of simple, refined carbs that cause rapid blood sugar spikes, you’ll want to prioritize complex carbohydrates that are rich in fiber. Fiber plays a crucial role by slowing down the digestion and absorption of glucose into your bloodstream, leading to a more gradual and stable rise in blood sugar.
Excellent sources of complex carbohydrates include whole grains like oats (especially steel-cut or rolled oats), quinoa, brown rice, barley, farro, and 100% whole-wheat bread or pasta. These options not only help regulate blood sugar but also provide sustained energy, keeping you feeling fuller longer and supporting healthy digestion. For instance, a bowl of oatmeal for breakfast can provide a steady energy release that white toast simply cannot.
Legumes are another fantastic choice, offering a powerful combination of carbohydrates, protein, and dietary fiber. Lentils, chickpeas, black beans, kidney beans, and cannellini beans are incredibly versatile and can be added to soups, salads, stews, or even mashed into dips like hummus. Their unique nutrient profile makes them a slow-digesting food that helps prevent post-meal blood sugar surges while delivering essential nutrients like folate and iron.
Crucially, even with smart carbohydrate choices, portion sizes matter immensely. It’s easy to overconsume even healthy carbs, which can still lead to elevated blood sugar. Learning to identify appropriate serving sizes for various carbohydrate-rich foods is vital. Your healthcare provider or a registered dietitian can help you understand carbohydrate counting and how to integrate it into your meal planning, ensuring you get the energy you need without overwhelming your system.
Lean Proteins: Essential for Growth and Blood Sugar Control

Incorporating lean protein sources into every meal and snack is a cornerstone of managing gestational diabetes. Protein plays a significant role in stabilizing blood sugar levels because it doesn’t directly raise blood glucose in the same way carbohydrates do. Instead, protein helps slow down the digestion of carbohydrates eaten alongside it, leading to a more gradual release of sugar into your bloodstream. Beyond blood sugar control, protein is absolutely vital for your baby’s rapid growth and development, forming the building blocks for cells, tissues, and organs. It also helps you feel more satisfied after meals, which can prevent overeating and reduce cravings.
Excellent options for lean protein include skinless poultry like chicken and turkey breast, which are low in saturated fat and high in protein. Fish is another superb choice, especially fatty fish like salmon, mackerel, and sardines, which are packed with omega-3 fatty acids. These healthy fats are crucial for your baby’s brain and eye development, and the protein content helps manage your blood sugar. Always choose low-mercury fish options during pregnancy and aim for 2-3 servings per week.
Eggs are a complete protein source, meaning they contain all nine essential amino acids. They are incredibly versatile and make for a quick and easy meal or snack, whether scrambled, hard-boiled, or incorporated into an omelet with plenty of vegetables. For plant-based protein options, tofu, tempeh, and edamame are excellent choices that provide substantial protein without animal fats.
When it comes to dairy, opt for low-fat or fat-free versions of products like Greek yogurt, cottage cheese, and milk. Plain Greek yogurt, in particular, is a powerhouse of protein and probiotics, but it’s essential to carefully check labels for added sugars, as many flavored yogurts can be surprisingly high in carbs. By making smart protein choices, you’ll support both your blood sugar stability and your baby’s healthy development.
Healthy Fats for Satiety and Fetal Development
While fat often gets a bad rap, healthy fats are absolutely essential during pregnancy, particularly when managing gestational diabetes. They don’t significantly impact blood sugar levels, making them a safe and beneficial addition to your diet. More importantly, healthy fats promote satiety, helping you feel fuller for longer after meals and reducing the likelihood of snacking on less healthy, high-carb options. Beyond helping you feel satisfied, these fats are crucial for your baby’s developing brain and nerve function, aiding in the absorption of fat-soluble vitamins (A, D, E, K), which are vital for overall health.
Focus on including sources of monounsaturated and polyunsaturated fats, which are known for their health benefits. Avocados are a fantastic example, rich in monounsaturated fats, fiber, and potassium. They can be enjoyed sliced on whole-grain toast, added to salads, or mashed into guacamole.
Nuts and seeds are another excellent source of healthy fats, fiber, and various micronutrients. Almonds, walnuts, pecans, and cashews offer different nutritional profiles; for instance, walnuts are particularly rich in omega-3s. Seeds like chia seeds, flaxseeds, and pumpkin seeds are also powerhouses of nutrients, fiber, and healthy fats. Just remember to be mindful of portion sizes with nuts and seeds, as they are calorie-dense. A small handful typically suffices for a snack.
Olive oil is a staple in healthy cooking, providing beneficial monounsaturated fats. Use it for sautéing vegetables, dressing salads, or as a dip for whole-grain bread. Other healthy cooking oils include avocado oil and canola oil (though choose expeller-pressed varieties where possible).
On the flip side, it’s crucial to avoid trans fats, which are often found in highly processed foods, fried items, and some baked goods. These fats offer no nutritional benefit and can be detrimental to heart health. You should also limit saturated fats, typically found in high quantities in red meat, butter, and full-fat dairy, as excessive intake can negatively impact overall health during pregnancy and beyond. Prioritizing healthy fats ensures both your and your baby’s well-being without causing blood sugar spikes.
Non-Starchy Vegetables & Low-Glycemic Fruits
Non-starchy vegetables and low-glycemic fruits are your allies in managing gestational diabetes, offering a wealth of nutrients, fiber, and flavor with minimal impact on blood sugar. When planning your meals, aim to fill at least half your plate with non-starchy vegetables. These nutrient-dense powerhouses are incredibly low in carbohydrates, calories, and sugar, yet packed with essential vitamins, minerals, antioxidants, and dietary fiber.
Excellent non-starchy options include leafy greens like spinach, kale, collard greens, and romaine lettuce. Other fantastic choices are broccoli, cauliflower, bell peppers (all colors!), zucchini, cucumber, asparagus, green beans, mushrooms, and onions. These vegetables can be enjoyed in generous portions, whether steamed, roasted, grilled, or added raw to salads. They help you feel full and satisfied without contributing excessive carbohydrate load, making them perfect for boosting your nutrient intake and managing blood sugar.
When it comes to fruit, the key is moderation and choosing low-glycemic options. Low-glycemic fruits are those that cause a slower and more gradual rise in blood sugar compared to high-glycemic fruits. Berries (strawberries, blueberries, raspberries, blackberries) are excellent choices due to their high fiber content and antioxidant levels. Apples, pears, cherries, and grapefruit are also good low-glycemic options. Always be mindful of portion sizes; a small apple or a cup of berries is generally considered a suitable serving. Eating fruit whole rather than drinking juice is also preferred, as the fiber in whole fruit helps slow sugar absorption.
These fruits and vegetables provide essential vitamins (like Vitamin C and K), minerals (like potassium and magnesium), and a significant amount of dietary fiber. Fiber is particularly beneficial as it aids digestion, helps prevent constipation (a common pregnancy complaint), and further supports stable blood sugar levels by slowing carbohydrate absorption. Incorporating a colorful variety of these foods ensures you’re getting a broad spectrum of nutrients for a healthy pregnancy.
Practical Meal Planning & Eating Strategies
Beyond choosing the right foods, how you eat them is equally important for effective gestational diabetes management. Strategic meal planning and eating habits can significantly impact your blood sugar stability and overall well-being throughout your pregnancy.
A highly effective strategy is to aim for smaller, more frequent meals and snacks throughout the day. Instead of three large meals that can overwhelm your system with a sudden influx of glucose, try to consume three modest meals and two to three planned snacks. This approach keeps your digestive system working steadily, preventing significant dips and spikes in blood sugar. For example, you might have breakfast, a mid-morning snack, lunch, an afternoon snack, dinner, and potentially a small bedtime snack. This consistent fueling helps maintain stable energy levels and can curb intense hunger that might lead to poor food choices.
Another crucial strategy is to combine carbohydrates with protein and healthy fats at every meal and snack. This synergy is powerful: protein and fat slow down the digestion and absorption of carbohydrates, blunting the blood sugar response. For instance, instead of just eating an apple (a carbohydrate), pair it with a tablespoon of peanut butter (protein and healthy fat) or a handful of almonds. If you’re having whole-grain toast, top it with avocado and a hard-boiled egg. This combination helps to create a more balanced meal that provides sustained energy and avoids rapid blood sugar spikes.
Finally, regularly monitoring your blood glucose levels, as advised by your healthcare provider, is perhaps the most critical practical strategy. Blood glucose monitoring isn’t just about identifying highs; it’s a powerful tool for learning. Each reading provides immediate feedback on how your body responds to different foods, portion sizes, and meal combinations. This personalized data empowers you to make adjustments to your diet and fine-tune your meal plan. Work closely with your doctor or a registered dietitian to interpret your readings and make informed decisions that support optimal blood sugar control.
Effectively managing gestational diabetes through diet involves a conscious effort to select nutrient-dense foods that support stable blood sugar levels. By prioritizing complex carbohydrates, lean proteins, healthy fats, and a wealth of non-starchy vegetables and fruits, you can nourish yourself and your baby while minimizing health risks associated with GD. Remember that healthy eating for gestational diabetes is a powerful tool for a healthy pregnancy. Always consult with your doctor or a registered dietitian to develop a personalized meal plan tailored to your specific needs, and diligently monitor your blood sugar for the best possible outcome during your pregnancy. Your commitment to a healthy diet is a profound step towards safeguarding both your health and the well-being of your little one.
Frequently Asked Questions
What are the best carbohydrate choices for managing gestational diabetes effectively?
For effective gestational diabetes management, focus on complex carbohydrates rich in fiber, such as whole grains (like oats, quinoa, and brown rice), whole-wheat bread, and starchy vegetables like sweet potatoes (in moderation). These choices digest slower, leading to a more gradual rise in blood sugar compared to refined carbohydrates. Prioritizing these “good carbs” helps maintain stable glucose levels while providing essential energy for pregnancy.
How do lean proteins and healthy fats help stabilize blood sugar for gestational diabetes?
Lean proteins and healthy fats are crucial for stabilizing blood sugar in gestational diabetes because they slow down the digestion and absorption of carbohydrates, preventing rapid glucose spikes. Incorporating sources like chicken, fish, eggs, beans, nuts, seeds, and avocados in your meals and snacks can also enhance satiety, helping you feel fuller longer and manage portion sizes. This balanced approach to “gestational diabetes foods” supports both maternal and fetal health.
Which fruits and vegetables are most beneficial for a gestational diabetes diet?
For a gestational diabetes diet, prioritize non-starchy vegetables like leafy greens (spinach, kale), broccoli, bell peppers, and green beans, as they are low in carbohydrates and high in essential nutrients. When it comes to fruits, opt for options rich in fiber and lower in sugar, such as berries, apples, pears, and grapefruit, always mindful of portion control. These choices provide vital vitamins and minerals without significantly impacting blood glucose levels.
What are some practical snack ideas for women managing gestational diabetes between meals?
Practical snack ideas for gestational diabetes typically combine a lean protein or healthy fat with a small portion of complex carbohydrate to prevent blood sugar spikes. Consider options like Greek yogurt with a few berries, a handful of almonds with an apple slice, hard-boiled eggs, or cottage cheese with vegetable sticks. These balanced “gestational diabetes snacks” can help maintain stable glucose levels and curb hunger between main meals.
Why is portion control and consistent meal timing so important when eating with gestational diabetes?
Portion control and consistent meal timing are paramount for managing gestational diabetes because they directly impact your body’s ability to process glucose. Eating appropriate portion sizes prevents an overload of carbohydrates that can cause blood sugar levels to spike, while regular, evenly spaced meals and snacks (e.g., every 2-3 hours) help keep your glucose stable throughout the day. This strategic approach ensures your body can efficiently manage the “foods for gestational diabetes” you consume.
References
- https://www.mayoclinic.org/diseases-conditions/gestational-diabetes/in-depth/gestational-diabetes-diet/art-20047094
- https://diabetes.org/healthy-living/pregnancy/gestational-diabetes-nutrition-tips
- https://www.cdc.gov/diabetes/basics/gestational.html
- https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/gestational/eating-diet-nutrition
- https://my.clevelandclinic.org/health/articles/23307-gestational-diabetes-diet
- https://www.ucsfhealth.org/conditions/gestational-diabetes/diet
- Gestational diabetes