Finding the “best” workout for diabetics isn’t about a single exercise, but rather a strategic combination of aerobic activity, strength training, and flexibility, all tailored to your individual health needs and cleared by your doctor. The most effective approach integrates exercises that improve insulin sensitivity, manage blood sugar, and support cardiovascular health, making consistent movement the real winner in your diabetes management journey.
Why Exercise is Essential for Diabetes Management

Living with diabetes means actively managing your health, and exercise is one of the most powerful tools in your arsenal. It’s not just about looking good; it’s about feeling great, improving your body’s vital functions, and significantly reducing the risks associated with diabetes. Let’s explore the core benefits that make physical activity non-negotiable for those managing blood sugar.
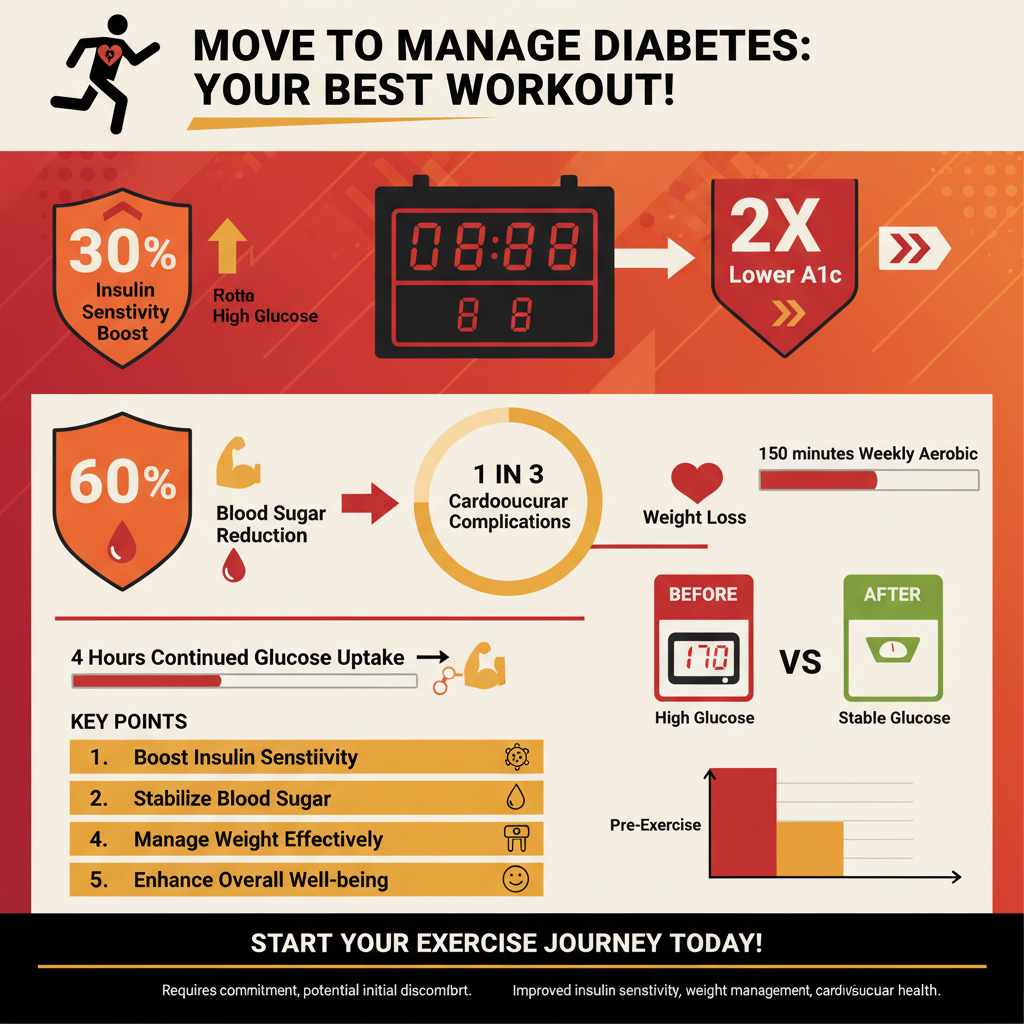
– Blood Sugar Regulation: Regular physical activity helps lower blood glucose levels by increasing insulin sensitivity and allowing cells to take up more glucose. When you move, your muscles use glucose for energy. This process is incredibly efficient: during exercise, your cells can absorb glucose even without insulin, or with less insulin, through a pathway called non-insulin-mediated glucose uptake. After your workout, your muscles continue to take up glucose to replenish glycogen stores, keeping your blood sugar lower for hours. This consistent lowering effect helps stabilize your glucose levels throughout the day and contributes to a better long-term A1c.
– Improved Insulin Sensitivity: Exercise makes your body’s cells more responsive to insulin, which is crucial for both Type 1 and Type 2 diabetes management. For individuals with Type 2 diabetes, where insulin resistance is a major factor, increased sensitivity means your body can use the insulin it produces more effectively, requiring less of it to manage blood sugar. If you have Type 1 diabetes, enhanced insulin sensitivity means you might need less exogenous insulin, making blood sugar management potentially easier and more predictable. This cellular-level improvement is a game-changer, helping your body utilize glucose efficiently and reducing the overall burden on your insulin-producing cells.
– Weight Management and Cardiovascular Health: Regular exercise supports healthy weight, reduces blood pressure, improves cholesterol levels, and strengthens the heart, mitigating common diabetes complications. Many individuals with Type 2 diabetes also manage their weight, and exercise burns calories, helping to create a deficit necessary for weight loss or maintenance. Beyond the scales, physical activity significantly reduces visceral fat (fat around your organs), which is particularly harmful and linked to insulin resistance. Furthermore, it strengthens your heart muscle, improves circulation, and helps lower “bad” LDL cholesterol while raising “good” HDL cholesterol. These cardiovascular benefits are vital, as people with diabetes have a higher risk of heart disease, stroke, and other circulatory issues.
Aerobic Exercise: The Foundation for Heart Health

Aerobic exercise, often called cardio, is the cornerstone of any effective fitness plan for individuals with diabetes. It’s about getting your heart pumping and your lungs working, which has profound benefits for blood sugar control and overall health.
– Recommended Activities: Brisk walking, cycling, swimming, dancing, or jogging are excellent choices that get your heart rate up. The beauty of aerobic exercise is its accessibility and variety. Brisk walking is fantastic because it’s low-impact and can be done almost anywhere, making it a great starting point for many. Cycling, whether outdoors or on a stationary bike, provides a great cardio workout while being gentle on joints. Swimming offers a full-body workout with minimal impact, ideal for those with joint pain or neuropathy. Dancing is a fun and expressive way to move, while jogging, for those cleared for higher impact, builds endurance and strengthens bones. The key is finding an activity you enjoy and can stick with!
– Benefits for Diabetics: Aerobic exercise directly lowers blood sugar during and after exercise, improves cardiovascular fitness, and helps with weight control. As you engage in aerobic activity, your muscles actively consume glucose from your bloodstream for energy. This immediate effect helps manage post-meal spikes and can lead to lower overall glucose levels. Over time, consistent cardio improves your heart’s efficiency, strengthening your cardiovascular system and reducing your risk for heart disease, a major concern for individuals with diabetes. It also contributes significantly to calorie expenditure, aiding in weight management and reducing the health risks associated with excess body fat.
– Frequency and Duration: Aim for at least 150 minutes of moderate-intensity aerobic activity per week, spread across most days. Moderate intensity means you’re working hard enough to raise your heart rate and break a sweat, but you can still carry on a conversation (the “talk test”). You don’t have to do it all at once! Breaking your activity into shorter, more manageable chunks, like three 10-minute walks per day, can be just as effective. Consistency is more important than sporadic bursts of intense activity. Gradually increase your duration or intensity as your fitness improves to keep challenging your body and reaping the benefits.
Strength Training: Building Muscle for Better Metabolism

While cardio gets a lot of attention, strength training is equally vital for diabetes management. Building muscle isn’t just for bodybuilders; it’s a powerful way to improve your body’s ability to handle glucose and boost your metabolism.
– Types of Resistance: Include bodyweight exercises, resistance bands, or free weights to build muscle mass. There’s a strength training option for everyone, regardless of fitness level or access to equipment. Bodyweight exercises like squats, lunges, push-ups (even on your knees or against a wall), and planks are excellent for building foundational strength using just your own body. Resistance bands offer portable and versatile options for targeting various muscle groups, from bicep curls to glute bridges. Free weights (dumbbells, barbells) and weight machines found in gyms provide opportunities for progressive overload, allowing you to gradually increase the challenge as you get stronger. The goal is to challenge your muscles, not necessarily to lift extremely heavy weights.
– Metabolic Advantages: Increased muscle mass improves the body’s ability to store and use glucose, leading to better long-term blood sugar control and insulin sensitivity. Muscle tissue is metabolically active, meaning it uses more energy even at rest compared to fat tissue. More importantly for diabetes, muscles are the primary storage site for glycogen (the stored form of glucose). When you have more muscle mass, you have a larger “storage tank” for glucose. This means your body can clear glucose from your bloodstream more effectively, reducing circulating blood sugar levels and improving your overall insulin response. This metabolic boost can significantly impact your A1c over time.
– Program Structure: Incorporate 2-3 sessions per week, targeting major muscle groups with 8-12 repetitions per set. To maximize benefits, structure your workouts to hit all major muscle groups: chest, back, shoulders, arms, legs, and core. For each exercise, aim for 2-3 sets of 8-12 repetitions, where the last few reps feel challenging but you can maintain good form. Always include a warm-up before lifting and a cool-down with stretching afterward. Proper form is crucial to prevent injury and ensure you’re effectively targeting the desired muscles. If you’re new to strength training, consider working with a certified personal trainer to learn the correct techniques.
Flexibility and Balance: Preventing Injury and Enhancing Mobility
While aerobic and strength training often take center stage, incorporating flexibility and balance exercises is like adding the finishing touches to a masterpiece. These practices are essential for preventing injuries, enhancing your ability to move comfortably, and improving your overall quality of life.
– Key Practices: Gentle stretching, yoga, Tai Chi, or Pilates can significantly improve your range of motion and stability. Stretching, whether static (holding a stretch) or dynamic (moving through a range of motion), helps lengthen muscles and improve joint flexibility. Yoga combines physical postures, breathing techniques, and meditation, offering a holistic approach to flexibility, strength, and mental well-being. Tai Chi, often described as “meditation in motion,” consists of slow, flowing movements that enhance balance, coordination, and mindfulness. Pilates focuses on core strength, flexibility, and controlled movements, leading to improved posture and body awareness. Each of these practices offers unique benefits and can be adapted to various fitness levels.
– Injury Prevention: Enhances joint flexibility, reducing the risk of strains and falls, which can be particularly important for individuals with diabetes-related neuropathy. Diabetes can sometimes lead to neuropathy, which is nerve damage that can affect sensation in the feet and legs, impacting balance and increasing the risk of falls. Flexibility exercises keep your joints lubricated and your muscles pliable, making you less prone to muscle strains or sprains during daily activities or other workouts. Balance exercises actively train your proprioception (your body’s sense of position in space), which is crucial for preventing stumbles and falls. Maintaining good mobility also means you can perform everyday tasks more easily and safely.
– Overall Well-being: Flexibility and balance training contributes to better posture, reduced muscle soreness, and can also help manage stress. Beyond the physical benefits, these practices have a calming effect. The mindful movements of yoga or Tai Chi, coupled with controlled breathing, can significantly reduce stress levels, which is important as chronic stress can negatively impact blood sugar control. Improved flexibility can alleviate common aches and pains, such as back stiffness, and contribute to better posture, which affects everything from breathing to confidence. By reducing muscle soreness, you’ll feel more comfortable and be more likely to stick with your overall exercise routine.
Important Considerations and Safety Tips
Embarking on or adjusting an exercise routine when you have diabetes comes with specific considerations. Prioritizing safety and working closely with your healthcare team will ensure your fitness journey is both effective and healthy.
– Consult Your Doctor: Always get medical clearance before starting or significantly changing an exercise routine, especially if you have complications. This is perhaps the most crucial step. Your doctor can assess your current health status, discuss any diabetes-related complications (like neuropathy, retinopathy, kidney disease, or heart conditions), and help you create a personalized exercise plan that’s safe and appropriate. They can advise on specific exercises to avoid or modifications to make, ensuring your routine supports your health rather than putting you at risk.
– Monitor Blood Sugar: Check your blood glucose before and after exercise, and be prepared with a quick source of glucose if needed. Exercise can significantly affect blood sugar levels, sometimes causing them to drop too low (hypoglycemia) or, less commonly, rise too high (hyperglycemia). Monitoring allows you to understand how different activities impact your body. If your blood sugar is below 100 mg/dL before exercise, a small snack might be needed. Always carry a fast-acting source of glucose, like glucose tablets, juice, or hard candy, to treat potential lows. If your blood sugar is very high (e.g., above 250 mg/dL with ketones, or above 300 mg/dL without ketones), your doctor might advise against exercising until levels are safer.
– Hydration and Foot Care: Drink plenty of water and wear appropriate, comfortable footwear to prevent blisters and foot injuries. Staying well-hydrated is essential for everyone, but particularly important for those with diabetes, as dehydration can affect blood sugar levels and overall performance. When it comes to your feet, neuropathy can reduce sensation, making you less aware of cuts, blisters, or sores. Wear well-fitting, supportive shoes and moisture-wicking socks to prevent friction and keep your feet dry. Always inspect your feet daily after exercise for any signs of irritation or injury.
– Listen to Your Body: Pay attention to how you feel; avoid overexertion and know the signs of hypoglycemia or hyperglycemia. Don’t push yourself too hard, especially when starting out. Fatigue, dizziness, excessive sweating, shakiness, or confusion during exercise could be signs of hypoglycemia and require immediate attention. Conversely, increased thirst, frequent urination, or unusual fatigue could indicate hyperglycemia. If you experience chest pain, shortness of breath, or severe pain, stop exercising immediately and seek medical attention. Gradually increase your intensity and duration, allowing your body time to adapt and get stronger.
The “best” workout for diabetics is ultimately a balanced, consistent, and personalized routine combining aerobic and strength training, with flexibility woven in. Starting small, gradually increasing intensity, and most importantly, consulting with your healthcare provider are crucial steps to creating a safe and effective exercise plan. Embrace movement as a powerful tool in managing your diabetes and improving your overall quality of life—your body will thank you for the energy, stability, and control you gain!
Frequently Asked Questions
What types of exercise are best for managing diabetes?
Focus on a combination of aerobic exercise and strength training for the most effective **diabetes management**. Aerobic activities like brisk walking, cycling, swimming, or dancing improve insulin sensitivity and lower blood sugar, while strength training (using weights, resistance bands, or bodyweight) builds muscle mass, which helps glucose uptake and boosts metabolism. Flexibility exercises, such as stretching or yoga, also complement these by improving range of motion and reducing injury risk.
How does regular exercise specifically help in controlling blood sugar levels?
Regular physical activity profoundly benefits blood sugar control by increasing insulin sensitivity, meaning your cells can more effectively use insulin to take up glucose from the bloodstream. Exercise also directly helps muscles absorb glucose for energy during and after a workout, even without insulin, which naturally lowers blood sugar. Over time, consistent exercise can lead to better A1C levels, reduced insulin resistance, and improved overall glycemic control for individuals with diabetes.
Are there any exercises diabetics should avoid, or specific precautions to take?
Diabetics should generally avoid exercises with a high risk of injury, especially if they have neuropathy or retinopathy, such as contact sports or heavy lifting that strains the eyes. It’s crucial to consult your doctor before starting any new **diabetic workout plan**, particularly if you have complications like nerve damage, heart conditions, or foot ulcers. Always wear appropriate footwear, monitor your blood sugar before and after exercise, and stay hydrated to prevent hypoglycemia or hyperglycemia.
How often and how intensely should a diabetic exercise to see benefits?
For optimal **diabetes management**, aim for at least 150 minutes of moderate-intensity aerobic activity spread throughout the week, such as 30 minutes on most days. Additionally, incorporate strength training exercises for all major muscle groups 2-3 times per week, with at least one day of rest between sessions. Consistency is key; even short bursts of activity can contribute to better blood sugar control and overall health for individuals with diabetes.
Which is more important for diabetics: aerobic exercise or strength training?
Both aerobic exercise and strength training are crucial and complement each other for effective **diabetes management**, so neither is inherently “more important.” Aerobic activities are excellent for immediate blood sugar lowering and cardiovascular health, while strength training builds muscle mass, which improves long-term insulin sensitivity and basal metabolism. A balanced **workout routine for diabetics** should ideally integrate both, providing comprehensive benefits for blood glucose control, weight management, and overall well-being.
References
- Get Active! | Exercise & Diabetes | ADA
- https://www.cdc.gov/diabetes/managing/healthy-living/physical-activity.html
- Healthy Living with Diabetes – NIDDK
- https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetes-and-exercise/art-20045615
- https://www.health.harvard.edu/staying-healthy/exercising-with-diabetes
- https://my.clevelandclinic.org/health/articles/17395-exercising-with-diabetes-how-to-do-it-safely
- https://en.wikipedia.org/wiki/Exercise_and_diabetes_mellitus