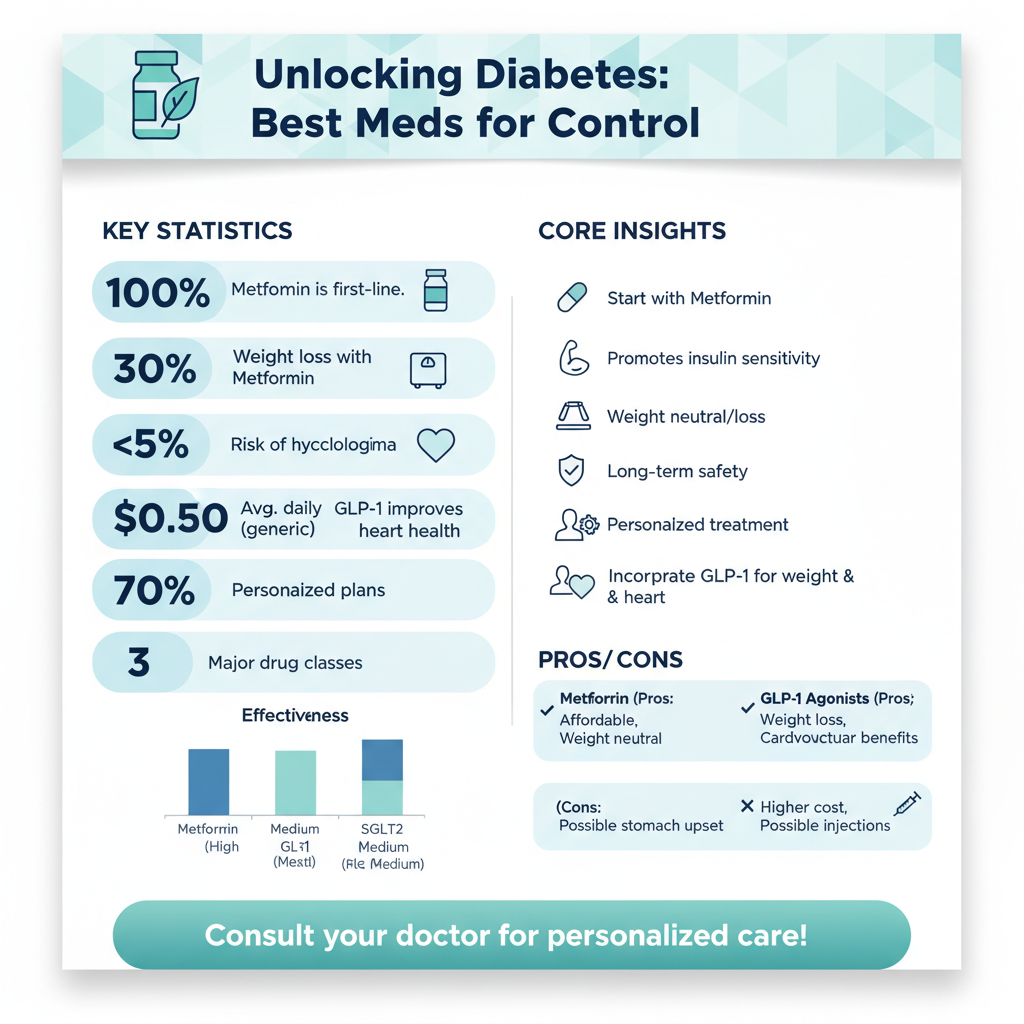
While there is no single “best” medicine for everyone, Metformin is universally recognized by medical guidelines as the first-line treatment for Type 2 diabetes due to its safety, effectiveness, and affordability. However, newer drug classes like GLP-1 receptor agonists (such as Ozempic) and SGLT2 inhibitors (such as Jardiance) are becoming increasingly popular “best” options for patients who also need support with weight loss or cardiovascular health. Ultimately, the right medication depends on your specific blood sugar targets, medical history, and lifestyle. Navigating a diabetes diagnosis can feel overwhelming, especially when you are faced with a pharmacy aisle full of options or a doctor listing off complex drug names. The landscape of diabetes management has changed dramatically in the last decade, moving away from a “one-size-fits-all” approach to highly personalized treatment plans. Let’s dive into the details to help you understand what might work best for your unique body.
Metformin: The Gold Standard First-Line Therapy

If you have recently been diagnosed with Type 2 diabetes, chances are high that the first prescription handed to you was for Metformin. For decades, this medication has held the title of the “gold standard” in diabetes care, and for good reason. It is widely considered the foundation upon which other treatments are built.
So, why is Metformin almost always the first choice? The answer lies in its unique ability to tackle the root causes of high blood sugar without aggressive side effects. Metformin works primarily by targeting the liver. In people with Type 2 diabetes, the liver often produces too much glucose, even when the body doesn’t need it. Metformin tells the liver to slow down this production. Simultaneously, it works in the background to improve your insulin sensitivity. This means it helps your muscle cells absorb sugar from your bloodstream more effectively, allowing your body to use its own natural insulin better.
The benefits of Metformin extend beyond just lowering A1C levels. One of its biggest advantages is its safety profile regarding weight. Unlike some older diabetes medications that could cause weight gain, Metformin is considered “weight neutral,” and some patients even experience modest weight loss while taking it. Additionally, because it doesn’t stimulate the pancreas to pump out more insulin, it carries a very low risk of causing hypoglycemia (dangerously low blood sugar).
Finally, we cannot overlook the practical benefits. Metformin has been around for a long time, which means it has a long-term safety record that doctors trust. It is also available as a generic drug, making it incredibly affordable—often costing just pennies a day. While some people experience stomach upset when starting the drug, extended-release versions have made it much easier for patients to tolerate this essential medication.
GLP-1 Receptor Agonists for Weight Management

In recent years, a new class of drugs has taken the medical world—and the media—by storm. GLP-1 receptor agonists, which include brand names like Ozempic (semaglutide), Wegovy, and Mounjaro (tirzepatide), have revolutionized how we treat Type 2 diabetes, particularly for those struggling with obesity.
These medications are usually injectable (though oral versions like Rybelsus exist) and work by mimicking the action of a natural hormone called glucagon-like peptide-1. When you eat, your gut releases this hormone to signal your pancreas to release insulin. However, in people with Type 2 diabetes, this signal is often weak. GLP-1 medications amplify this signal, ensuring your body produces the right amount of insulin in response to a meal.
But what makes GLP-1s a “best” option for so many patients today is their dual benefit. Beyond blood sugar control, these drugs are powerful tools for weight management. They work on the brain’s appetite centers to reduce hunger and cravings, and they slow down gastric emptying, meaning food stays in your stomach longer, making you feel fuller faster.
For patients carrying excess weight, this is a game-changer. Losing 5% to 15% (or more) of body weight can significantly improve insulin sensitivity, sometimes allowing patients to reduce other medications. If your primary goal involves both lowering your A1C and significant weight loss, your doctor might suggest a GLP-1 receptor agonist earlier in your treatment plan, potentially in combination with Metformin.
SGLT2 Inhibitors for Heart and Kidney Protection

Another major breakthrough in diabetes care comes in the form of SGLT2 inhibitors. You may recognize these by brand names such as Jardiance (empagliflozin) and Farxiga (dapagliflozin). These medications represent a completely different approach to managing blood sugar—one that focuses on the kidneys rather than the pancreas or liver.
Normally, your kidneys act as a filter, reabsorbing glucose back into the bloodstream so it isn’t lost. SGLT2 inhibitors block this reabsorption process. Essentially, they open a “release valve,” allowing your body to expel excess sugar through your urine. This mechanism helps lower blood sugar levels effectively without relying on insulin.
However, the “best” aspect of SGLT2 inhibitors isn’t just about glucose; it’s about organ protection. Large-scale clinical trials have shown that these drugs offer profound benefits for the heart and kidneys. For patients with Type 2 diabetes who also have established cardiovascular disease, heart failure, or chronic kidney disease (CKD), SGLT2 inhibitors are often the top choice.
They help reduce blood pressure and reduce the strain on the heart, leading to fewer hospitalizations for heart failure. Furthermore, they slow the progression of kidney damage, which is a common long-term complication of diabetes. If your medical history includes heart concerns or if you want to be proactive about kidney health, this class of medication serves double duty: managing your diabetes while acting as a shield for your vital organs.
DPP-4 Inhibitors and Sulfonylureas
While Metformin, GLP-1s, and SGLT2s often steal the spotlight, there are other oral medications that play a vital role in diabetes management, specifically DPP-4 inhibitors and Sulfonylureas.
DPP-4 Inhibitors: Medications like Januvia (sitagliptin) are often prescribed for patients who need help lowering blood sugar but cannot tolerate Metformin or need a gentle add-on therapy. They work by blocking the enzyme that breaks down incretin hormones, thereby helping the body produce insulin when it’s needed. They are generally weight-neutral and have very few side effects, making them a “friendly” option for elderly patients or those with sensitive stomachs. While they aren’t as powerful as GLP-1s for weight loss, they are an excellent, low-hassle maintenance medication.
Sulfonylureas: This class includes drugs like glipizide and glyburide. These are some of the oldest diabetes medications available and work by directly stimulating the pancreas to squeeze out more insulin. The primary advantage here is cost-effectiveness; like Metformin, they are very affordable. They are also quite potent at lowering high blood sugar quickly. However, they come with a caveat: because they force insulin release regardless of glucose levels, they carry a higher risk of hypoglycemia (low blood sugar) and can sometimes cause mild weight gain. They remain a valid option for many, especially when cost is a major factor, but require careful monitoring of meal timing to avoid blood sugar dips.
When Insulin Therapy Is Necessary
There is a common misconception that starting insulin means you have “failed” at managing your diabetes. We need to clear that up right now: needing insulin is not a failure; it is simply a reflection of the biology of diabetes. Type 2 diabetes is a progressive condition. Over time, the beta cells in the pancreas that produce insulin can become exhausted and less efficient. For some people, oral medications and lifestyle changes eventually aren’t enough to keep blood sugar in a safe range.
When A1C levels remain high despite using multiple other medications, insulin becomes the “best” and safest medicine because it is the most natural way to replace what your body is missing. Doctors usually start with basal insulin (long-acting), which provides a steady background level of insulin to keep blood sugar stable overnight and between meals. If more control is needed, mealtime insulin (rapid-acting) may be added.
Modern insulin pens are discreet, the needles are ultra-thin and virtually painless, and the dosing can be highly customized. Insulin therapy provides the ultimate control over blood sugar, preventing the dangerous long-term complications associated with hyperglycemia. Embracing insulin when necessary is a powerful step toward protecting your long-term health.
How to Choose the Best Medicine for You
With so many options on the table, how do you and your doctor decide which path to take? This decision requires a personalized approach that looks at the whole person, not just the blood sugar numbers.
Here are the critical factors you should discuss during your next appointment:
* Comorbidities: Do you have high blood pressure, heart disease, or kidney issues? If so, SGLT2 inhibitors or GLP-1s might be prioritized over other options.
* Weight Goals: Is weight loss a primary objective? If yes, a GLP-1 receptor agonist is likely the most effective tool.
* Side Effects: How sensitive is your stomach? If you have a history of GI issues, your doctor may start with extended-release Metformin or DPP-4 inhibitors rather than GLP-1s.
* Hypoglycemia Risk: If your job involves driving or heavy machinery, or if you live alone, avoiding low blood sugar is crucial. You might avoid Sulfonylureas in favor of drugs that don’t cause lows.
* Needle Phobia: Are you comfortable with injections? While the needles for GLP-1s and insulin are tiny, some patients prefer to stick strictly to oral pills.
* Cost and Insurance: This is a major practical factor. Newer drugs like Ozempic or Jardiance can be expensive without good insurance coverage. Metformin and Sulfonylureas are generally the most budget-friendly.
Finding the best medicine for diabetes type 2 is a collaborative process that often starts with Metformin but may evolve to include combination therapies like GLP-1s or SGLT2 inhibitors for added health protection. Because diabetes is a progressive condition, your medication needs may change over time to keep your blood sugar in a healthy range. Schedule an appointment with your endocrinologist or primary care physician to review your current A1C levels and determine if your current treatment plan is the most effective option for your long-term health.
Frequently Asked Questions
What is considered the first-line best medicine for diabetes type 2?
Metformin is widely recognized by medical guidelines and healthcare providers as the first-line treatment and best starting medicine for type 2 diabetes due to its high safety profile, affordability, and effectiveness. It works by reducing the amount of sugar your liver releases and improving how your body responds to insulin, often without causing weight gain or hypoglycemia (low blood sugar). Most doctors prescribe Metformin alongside lifestyle changes like diet and exercise before adding other medications.
Which diabetes type 2 medications are best for promoting weight loss?
GLP-1 receptor agonists (such as semaglutide) and dual GIP/GLP-1 agonists (such as tirzepatide) are currently considered the most effective diabetes medications for patients seeking significant weight loss. These injectable treatments lower blood sugar while simultaneously slowing digestion and signaling fullness to the brain, which helps reduce calorie intake. Because obesity is a major risk factor for diabetes complications, these medications address both glucose control and weight management simultaneously.
What are the best diabetes medications for protecting heart and kidney health?
SGLT2 inhibitors and GLP-1 receptor agonists are the top choices for patients who have existing heart disease, heart failure, or chronic kidney disease (CKD). Clinical studies have shown that SGLT2 inhibitors (which help kidneys remove sugar through urine) significantly reduce the risk of heart failure hospitalization and slow kidney disease progression. Major health organizations now recommend prioritizing these specific drug classes for high-risk patients regardless of their current A1C levels.
What are the safest oral diabetes medicines with the fewest side effects?
While individual reactions vary, DPP-4 inhibitors (such as Sitagliptin) are often cited as some of the best-tolerated oral medications because they are “weight neutral” and rarely cause low blood sugar or gastrointestinal distress. Unlike Metformin, which can cause stomach upset, or sulfonylureas, which carry a risk of hypoglycemia, DPP-4 inhibitors provide a gentler option for moderate blood sugar control. They are frequently used when patients cannot tolerate the side effects of stronger diabetes treatments.
How do doctors determine the best medicine combination for high A1C levels?
When A1C levels are significantly high (often above 9% or 10%), doctors may prescribe combination therapy immediately rather than starting with a single drug to bring glucose levels down quickly and safely. This approach often involves pairing Metformin with a basal insulin or a high-efficacy agent like a GLP-1 agonist to attack high blood sugar from multiple angles. The “best” combination is highly personalized based on the patient’s risk of hypoglycemia, insurance coverage, and willingness to use injectable medications.
References
- Insulin, Medicines, & Other Diabetes Treatments – NIDDK
- Type 2 diabetes – Diagnosis and treatment – Mayo Clinic
- https://www.nhs.uk/conditions/type-2-diabetes/medicine/
- https://my.clevelandclinic.org/health/treatments/13901-diabetes-medicines
- https://diabetes.org/health-wellness/medication
- Type 2 diabetes: Which medication is best for me? – Harvard Health
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes/medicines-for-diabetes
- https://www.cdc.gov/diabetes/managing/manage-blood-sugar.html