For individuals managing diabetes, certain vitamins and minerals are often highlighted for their potential role in supporting overall health, blood sugar regulation, and preventing complications. Key among these often include Vitamin D for its role in insulin sensitivity, Vitamin B12 to address potential deficiencies from medication, and Magnesium and Chromium for their involvement in glucose metabolism. However, it’s crucial to remember that supplements should always complement, not replace, medical treatment and dietary management, and you should always consult your healthcare provider before starting any new regimen.
Why Vitamins Matter for Diabetics

Living with diabetes is a journey that often requires careful attention to many aspects of your health, and nutrition is certainly at the top of that list. While a balanced diet is fundamental, individuals with diabetes may sometimes find themselves facing unique nutritional challenges or increased needs. This isn’t just about what you eat; it can also be influenced by the condition itself, the medications you take, and even specific dietary recommendations.
Firstly, diabetes can directly impact how your body absorbs and utilizes certain nutrients. For instance, high blood sugar levels can lead to increased urination, which in turn can cause some water-soluble vitamins and minerals to be flushed out of the body more quickly, potentially leading to deficiencies over time. The condition also places increased oxidative stress on the body, meaning there’s a higher demand for antioxidants and nutrients that help repair cellular damage.
Secondly, a major factor for many managing type 2 diabetes is medication. Metformin, a widely prescribed drug, is incredibly effective at helping regulate blood sugar, but it’s also known to interfere with the absorption of Vitamin B12. This isn’t a reason to stop taking your medication, but it is a strong reason to be aware of potential side effects and discuss monitoring and supplementation with your doctor.
Lastly, while dietary restrictions are often necessary to manage blood sugar, sometimes these can inadvertently limit the intake of certain micronutrients if not carefully planned. For example, if you’re reducing your intake of certain food groups, you need to ensure you’re getting essential vitamins and minerals from other sources.
This is where specific vitamins and minerals can play a supportive role. They can help bridge nutritional gaps, enhance the body’s natural processes for blood sugar control, support nerve function (which is often compromised in diabetes), bolster cardiovascular health, and reduce the risk of common diabetes-related complications like neuropathy or kidney issues. It’s vital to view these supplements as a supportive tool within a comprehensive diabetes management plan, working hand-in-hand with a healthy diet, regular exercise, and prescribed medications, not as a replacement for any of them. Think of them as helping your body run a little smoother, but your healthcare team provides the engine and the roadmap!
Vitamin D: Supporting Insulin Sensitivity
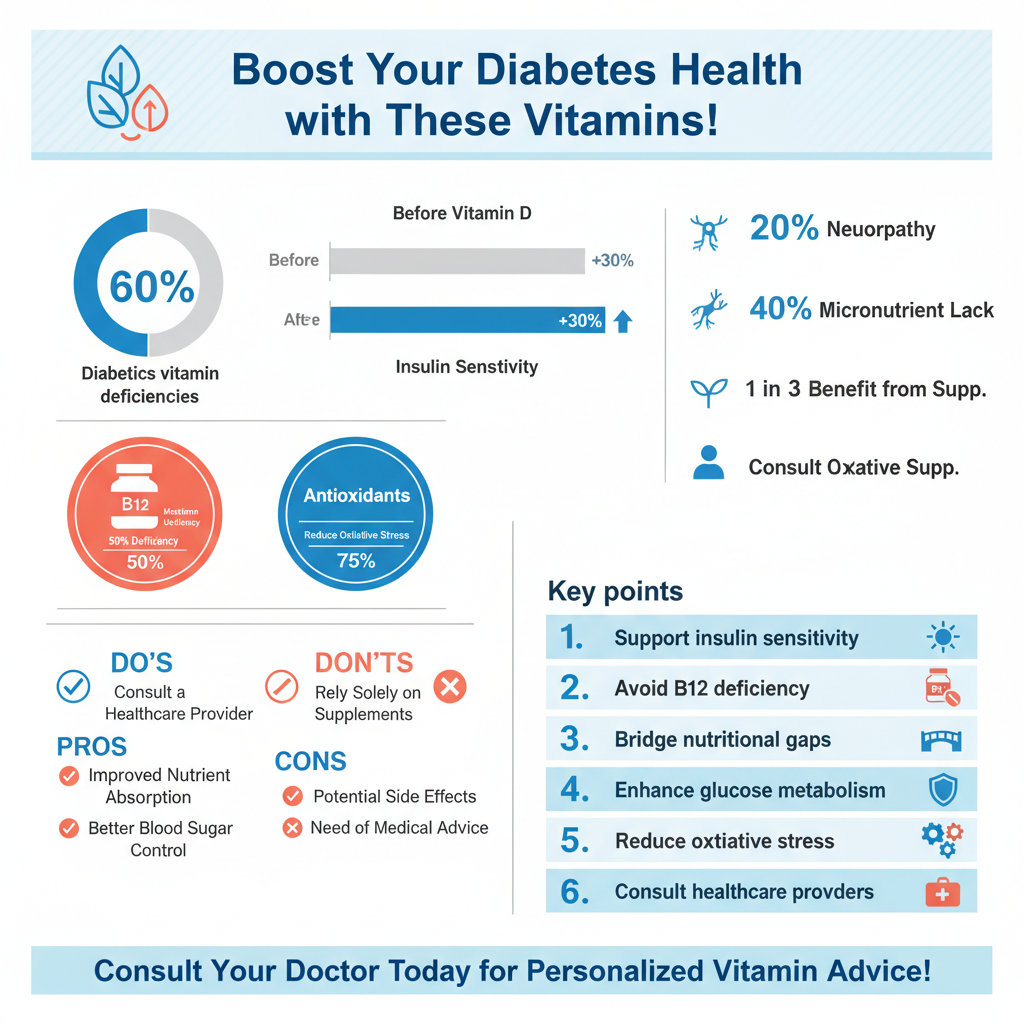

Often referred to as the “sunshine vitamin,” Vitamin D is far more than just essential for bone health; it’s a powerful hormone-like substance that plays a surprisingly significant role in metabolic health, especially for those with diabetes. Research consistently shows that a large percentage of individuals with both type 1 and type 2 diabetes are deficient in Vitamin D. This isn’t just a coincidence; there’s a strong biological connection.
Vitamin D receptors are found throughout the body, including in the beta cells of the pancreas, which are responsible for producing insulin. Adequate Vitamin D levels are believed to influence both insulin production and insulin sensitivity. When your body is more sensitive to insulin, it means your cells can more effectively take up glucose from your bloodstream, leading to better blood sugar control. Some studies even suggest that sufficient Vitamin D levels might help reduce the risk of developing type 2 diabetes in the first place, and in those already diagnosed, it may improve glycemic control and potentially lower the risk of complications such as kidney disease or nerve damage.
So, how do you get enough Vitamin D? Your primary source is typically sun exposure, as your skin produces Vitamin D when exposed to UV-B rays. However, factors like skin tone, geographical location, time of year, and sunscreen use can limit this. Dietary sources include fatty fish like salmon, mackerel, and tuna, as well as fortified foods such such as milk, cereals, and some yogurts. Given the widespread prevalence of deficiency, especially among diabetics, supplementation is often recommended. However, Vitamin D is a fat-soluble vitamin, meaning it can accumulate in your body, so it’s essential to have your levels checked by your doctor before starting supplementation and to take the dose they recommend. They’ll help you find the right balance to support your health safely.
Vitamin B12: Protecting Nerve Health

When we talk about diabetes management, the conversation often circles back to specific medications that have revolutionized treatment. Metformin is a fantastic example, helping millions manage their blood sugar effectively. However, like many powerful medicines, it comes with potential side effects, and one that’s particularly relevant for diabetics is its impact on Vitamin B12 absorption.
Metformin works by reducing glucose production by the liver and improving insulin sensitivity, but it can also interfere with calcium absorption in the gut, which is necessary for B12 to be properly absorbed. Over time, this can lead to a significant Vitamin B12 deficiency, especially in individuals taking metformin for extended periods or at higher doses.
Why is B12 so crucial? It’s a powerhouse vitamin involved in several fundamental bodily functions. Primarily, it’s vital for healthy nerve function, playing a key role in the formation of myelin, the protective sheath around nerves. It’s also essential for the production of red blood cells and DNA synthesis. For individuals with diabetes, who are already at a higher risk for nerve damage (diabetic neuropathy), a B12 deficiency can be particularly concerning. Symptoms of B12 deficiency — such as numbness, tingling, weakness, fatigue, memory issues, and balance problems — can mimic or exacerbate the symptoms of diabetic neuropathy, making diagnosis and management more complex.
This makes regular monitoring of B12 levels a critical part of care for anyone with diabetes on metformin. Your doctor can perform a simple blood test to check your levels. If a deficiency is identified, supplementation, often through oral tablets or sometimes even injections in severe cases, becomes incredibly important. Addressing B12 deficiency not only helps protect your nerve health but also supports your overall energy levels and cognitive function, making it a key player in maintaining your quality of life while managing diabetes.
Magnesium and Chromium: Key Metabolic Minerals
Beyond the vitamins, several minerals play unsung yet vital roles in blood sugar regulation. Magnesium and Chromium stand out as two essential micronutrients directly involved in glucose metabolism and insulin signaling, making them particularly important for individuals with diabetes.
Magnesium is a true workhorse in the human body, participating in over 300 enzymatic reactions. Its roles range from nerve and muscle function to protein synthesis and blood pressure regulation. Critically for diabetics, magnesium plays a vital role in glucose control and insulin signaling. It helps insulin receptors on cells function properly, allowing glucose to enter cells more effectively. Think of magnesium as a key helper for insulin, ensuring the “door” to your cells opens smoothly for sugar. Unfortunately, magnesium deficiency is quite common, and even more so in individuals with diabetes. High blood sugar levels can lead to increased magnesium excretion through the kidneys, creating a vicious cycle. Symptoms of magnesium deficiency can include muscle cramps, fatigue, and weakness, which can sometimes be confused with diabetic symptoms. Supplementation, under medical guidance, may help improve insulin sensitivity and contribute to better blood glucose levels, making it a valuable consideration for your diabetes management strategy.
Chromium is another trace mineral that, while needed in very small amounts, has a profound impact on how your body handles sugar. It’s a key component of a molecule called chromodulin, which is believed to enhance the action of insulin. Essentially, chromium acts as an amplifier for insulin, helping it to work more efficiently. This means your body can use blood sugar more effectively, potentially leading to improved glycemic control and lower fasting blood glucose levels. Some studies have also suggested chromium’s potential role in improving cholesterol levels, which is often a secondary concern for those with diabetes. While chromium is found in foods like whole grains, broccoli, and lean meats, absorption can be variable. As with any supplement, especially one impacting blood sugar, discussing chromium supplementation with your doctor is crucial to determine if it’s right for you and what the appropriate dosage should be. Getting these metabolic minerals right can offer significant support to your body’s natural ability to manage glucose.
Other Potentially Beneficial Supplements
While Vitamin D, B12, Magnesium, and Chromium are often top of mind, the world of supplements offers a few other contenders that might provide additional support for individuals managing diabetes. Remember, these are also best discussed with your healthcare provider to ensure they fit safely into your personal health plan.
* Alpha-Lipoic Acid (ALA): This powerful antioxidant is unique because it’s both water and fat-soluble, allowing it to work in various parts of the body. ALA has gained significant attention for its potential benefits in diabetes. It may help improve insulin sensitivity, meaning your cells respond better to insulin, leading to more efficient glucose uptake. Even more excitingly, ALA is often used to help manage the uncomfortable symptoms of diabetic neuropathy, such as burning, tingling, and numbness in the hands and feet. It’s thought to do this by reducing oxidative stress and improving nerve blood flow. There are two forms, R-ALA and S-ALA, with R-ALA generally considered the more bioactive and effective form.
* Coenzyme Q10 (CoQ10): CoQ10 is another potent antioxidant that plays a crucial role in cellular energy production, particularly in the mitochondria (the “powerhouses” of your cells). For individuals with diabetes, who often have an increased risk of cardiovascular complications, CoQ10 may offer significant benefits. It’s known to support heart health, potentially helping to manage blood pressure and cholesterol levels, which are frequently concerns for diabetics. Furthermore, if you’re taking statin medications to manage cholesterol (a common prescription for diabetics), statins can sometimes deplete the body’s natural CoQ10 levels, making supplementation particularly relevant in those cases to help mitigate potential side effects like muscle pain.
* Omega-3 Fatty Acids: Found abundantly in fatty fish like salmon and tuna, as well as in flaxseeds and walnuts, omega-3s (specifically EPA and DHA) are celebrated for their anti-inflammatory properties. Chronic low-grade inflammation is often associated with insulin resistance and diabetes complications. By helping to reduce inflammation, omega-3s may play a role in improving overall metabolic health. Crucially, they are also well-known for their cardiovascular benefits, including helping to lower triglyceride levels, slightly reduce blood pressure, and improve overall heart health – all major concerns for individuals with diabetes. However, caution is advised, especially for those on blood thinners, as high doses of omega-3s can have a blood-thinning effect. Always discuss fish oil or omega-3 supplements with your doctor to ensure they are safe and appropriate for your specific health needs and medications.
Important Considerations and Doctor Consultation
Navigating the world of vitamins and supplements, especially when managing a complex condition like diabetes, requires a thoughtful and informed approach. It’s not just about picking up a bottle off the shelf; it’s about making choices that truly support your health without creating unintended risks. This is why the advice to always consult your healthcare provider or a registered dietitian before starting any new vitamin or supplement regimen isn’t just a suggestion—it’s a critical safety measure.
Here’s why that consultation is non-negotiable:
* Interactions with Diabetes Medications: This is perhaps the most crucial point. Many supplements can interact with your prescribed diabetes medications, potentially altering their effectiveness. For example, certain supplements can lower blood sugar too much when combined with insulin or oral hypoglycemic agents, leading to hypoglycemia (dangerously low blood sugar). Conversely, some supplements might inadvertently raise blood sugar. Other interactions could affect how your body metabolizes medications, making them more or less potent, or even increasing the risk of side effects. Your doctor understands these complex interactions and can advise you safely.
* Individualized Needs and Deficiencies: What works for one person with diabetes might not be right for another. Your healthcare provider can assess your specific nutritional status through blood tests, diet analysis, and a review of your overall health. They can identify actual deficiencies (like low Vitamin D or B12) and recommend targeted supplementation rather than a scattergun approach. A registered dietitian can also provide invaluable guidance on how to optimize your diet to address nutrient gaps first, and then strategically use supplements.
* Dosage Matters – And More Isn’t Always Better: The idea that “if a little is good, a lot must be better” is particularly dangerous when it comes to supplements. Excessive amounts of certain vitamins and minerals can be harmful, leading to toxicity. For example, too much Vitamin D can cause hypercalcemia (high calcium levels), leading to kidney stones and other serious issues. High doses of Vitamin B6 can cause nerve damage, and excessive iron can lead to organ damage. Your doctor can help you determine the correct, safe dosage based on your specific needs and current health status.
* Quality and Purity of Supplements: The supplement industry is not as tightly regulated as the pharmaceutical industry. This means that the quality, purity, and even the actual content of supplements can vary wildly between brands. Your doctor or dietitian may be able to recommend reputable brands that undergo third-party testing to ensure what’s on the label is actually in the bottle, and that it’s free from harmful contaminants.
Remember, supplements are powerful tools, and like any powerful tool, they need to be used correctly and safely. A personalized approach, developed in close collaboration with your healthcare team, is the best way to ensure that any supplements you take truly support your diabetes management and overall well-being.
Navigating the best vitamins for diabetes involves understanding your unique nutritional needs and potential deficiencies, all while prioritizing medical advice. While key vitamins like D, B12, Magnesium, and Chromium show promise in supporting blood sugar management and preventing complications, they are not a substitute for medication, a healthy diet, and regular exercise. Work closely with your healthcare team to develop a personalized supplement plan that safely supports your overall well-being and helps you effectively manage your diabetes.
Frequently Asked Questions
What are the top recommended vitamins for diabetics to support blood sugar control and overall well-being?
For individuals with diabetes, certain vitamins can be particularly beneficial for blood sugar management and preventing complications. Key recommendations often include Vitamin D, crucial for insulin sensitivity and immune function, and Magnesium, which plays a vital role in glucose metabolism. Additionally, B vitamins, especially B12, are important for nerve health, and Alpha-Lipoic Acid is valued for its antioxidant properties that can help combat oxidative stress.
Why is Vitamin B12 deficiency common in diabetics, especially those on Metformin, and how can it be addressed?
Vitamin B12 deficiency is frequently observed in people with diabetes, particularly among those taking Metformin, as the medication can interfere with its absorption in the gut. B12 is essential for nerve function, red blood cell formation, and DNA synthesis, so a deficiency can exacerbate symptoms like diabetic neuropathy. Regular screening for B12 levels is recommended for Metformin users, and supplementation (oral or injections) can effectively address the deficiency under a doctor’s guidance.
Which vitamins and supplements are often beneficial for managing diabetic neuropathy symptoms?
Managing diabetic neuropathy, a common complication affecting nerve function, can often be supported by specific vitamins and supplements. Alpha-Lipoic Acid is highly regarded for its antioxidant effects that can improve nerve health and reduce pain and numbness. B vitamins, particularly thiamine (B1), B6, and B12, are also crucial for nerve integrity and repair. Some may find relief with Magnesium for muscle and nerve function, but always consult a healthcare professional before starting new supplements.
Can a daily multivitamin be sufficient for diabetics, or should they consider specific individual supplements?
While a daily multivitamin can provide a general nutritional baseline, it may not be sufficient to address the specific deficiencies or therapeutic needs of individuals with diabetes. Diabetic patients often require higher doses of certain nutrients, like Vitamin D or B12, than a standard multivitamin provides, or specific supplements like Alpha-Lipoic Acid for targeted concerns. A personalized approach, guided by blood tests and a healthcare provider, is usually more effective than relying solely on a general multivitamin.
Are there any vitamins or herbal supplements that diabetics should be cautious about or avoid due to potential interactions or risks?
Diabetics should exercise caution with certain vitamins and herbal supplements due to potential interactions with medications or effects on blood sugar levels. High doses of Niacin (Vitamin B3) can sometimes raise blood sugar, while Chromium supplements, although marketed for glucose control, can interact with diabetes medications and should be used cautiously. Herbal remedies claiming to significantly lower blood sugar, such as bitter melon or ginseng, must be used under strict medical supervision to avoid hypoglycemia or adverse interactions with prescribed diabetes medications.
References
- https://www.diabetes.org/healthy-living/medication-treatments/vitamins-supplements
- https://www.mayoclinic.org/diseases-conditions/diabetes/expert-answers/supplements-for-diabetes/faq-20058197
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6480749/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3056801/
- Magnesium | Linus Pauling Institute | Oregon State University
- Vitamin D
- Chromium – Health Professional Fact Sheet
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6950247/