The “best” type 2 diabetes medication is not a universal choice, but rather a highly individualized decision made in consultation with your healthcare provider. While Metformin is often the first-line therapy for many, newer drug classes like GLP-1 receptor agonists and SGLT2 inhibitors offer significant additional benefits, including cardiovascular and kidney protection, for a growing number of patients. This guide provides an overview of the most common and effective medication categories to help you understand the options available for managing type 2 diabetes effectively, empowering you to have a more informed conversation with your doctor about what’s right for you.
Understanding Individualized Treatment Approaches

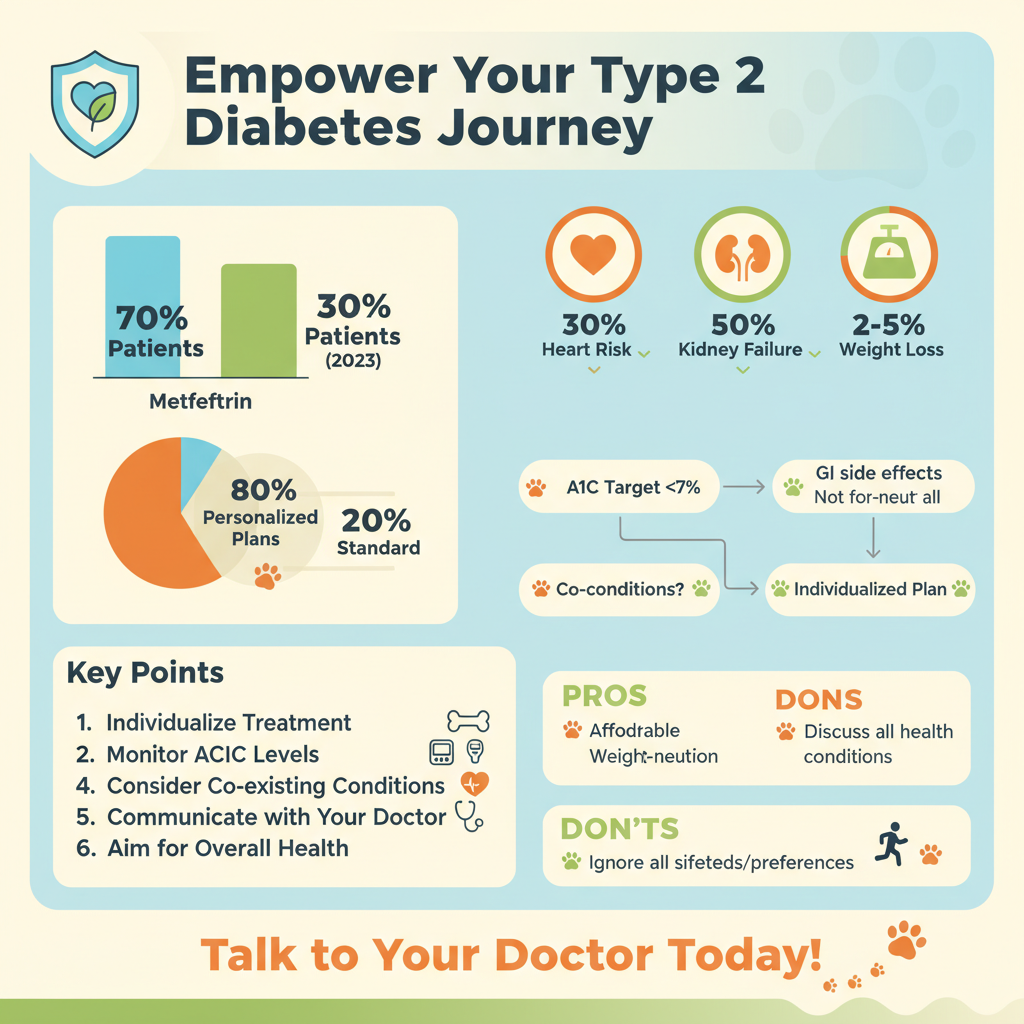
When it comes to managing type 2 diabetes, there’s no one-size-fits-all solution, and that’s perfectly okay! Your body, your lifestyle, and your health history are unique, which means your treatment plan should be too. The “best” medication for you will depend on several important factors that your healthcare provider carefully considers.
Firstly, your current A1C levels play a crucial role. This blood test reflects your average blood sugar over the past two to three months, giving a clear picture of how well your diabetes is currently controlled. Beyond that, any existing health conditions, such as heart disease, kidney disease, or even high blood pressure, will heavily influence medication choices. For example, some newer medications offer remarkable benefits specifically for heart and kidney health, making them a top choice for individuals with these co-existing conditions. Your weight is another key factor; some medications are known to help with weight loss, while others can cause weight gain. Of course, we can’t forget about potential side effects and how they might impact your daily life – finding a balance between effectiveness and tolerability is essential.
It’s also important to remember that treatment goals extend far beyond just lowering blood sugar. While achieving target glucose levels is fundamental, modern diabetes management aims to prevent serious complications like heart attacks, strokes, kidney failure, and nerve damage, ultimately working towards improving your overall quality of life. This holistic approach means that medication choices are often strategic, selected not just for their sugar-lowering power, but for their broader protective benefits. That’s why open communication with your doctor is absolutely crucial. Don’t hesitate to share your concerns, your lifestyle, and your preferences. Together, you can determine the most suitable regimen for your unique needs, ensuring your plan is not only effective but also sustainable and aligns with your personal health journey.
Metformin: The Foundation of Type 2 Diabetes Management

For many people starting their journey with type 2 diabetes management, Metformin is a familiar name, and for good reason! It’s often the very first medication prescribed and is considered a cornerstone of treatment worldwide. Think of Metformin as a diligent assistant helping your body work more efficiently. It primarily works in two key ways: first, it reduces the amount of glucose (sugar) your liver produces, especially overnight, which is often a significant contributor to high blood sugar in type 2 diabetes. Second, it improves your body’s sensitivity to insulin in muscle cells, meaning your body can use its own insulin more effectively to take glucose out of your bloodstream and into your cells for energy.
The benefits of Metformin are extensive and well-established. It’s highly effective at reducing A1C levels, helping you get closer to your target blood sugar goals. A huge plus is its low risk of hypoglycemia (low blood sugar), especially when used as a standalone therapy, which can be a significant concern with some other diabetes medications. Many individuals also appreciate its potential for modest weight loss or, at the very least, its weight-neutral effect, which can be a welcome bonus for those also focusing on weight management.
Like any medication, Metformin does come with potential side effects, though they are generally mild and manageable. The most common issues are primarily gastrointestinal, such as nausea, diarrhea, stomach upset, or gas. These symptoms often improve over time as your body adjusts, and your doctor might suggest starting with a low dose and gradually increasing it. Additionally, extended-release (ER) formulations of Metformin are available, which can significantly reduce these digestive side effects by releasing the medication more slowly throughout the day. It’s a classic for a reason, providing a solid, reliable foundation for most type 2 diabetes treatment plans.
GLP-1 Receptor Agonists: Weight Loss and Cardiovascular Benefits

Stepping into the world of newer, innovative diabetes medications, we encounter GLP-1 receptor agonists – a class that has truly revolutionized type 2 diabetes care. These medications are fascinating because they mimic the action of a natural hormone called glucagon-like peptide-1 (GLP-1), which your body usually releases after you eat. When you take a GLP-1 receptor agonist, it stimulates your pancreas to release insulin only when blood sugar levels are high, which significantly lowers the risk of hypoglycemia. But their magic doesn’t stop there! They also slow down the rate at which food leaves your stomach (gastric emptying), helping you feel fuller for longer, and reduce appetite, often leading to a natural decrease in food intake.
What makes GLP-1 receptor agonists truly stand out are their significant additional benefits beyond just blood sugar control. They are renowned for their impressive ability to promote weight loss, often a major challenge for individuals with type 2 diabetes. For many patients, losing even a modest amount of weight can have profound positive impacts on overall health. Even more crucially, a growing body of research has shown that this class of medications offers proven cardiovascular benefits, significantly reducing the risk of major adverse cardiovascular events like heart attack and stroke in many patients with established cardiovascular disease or those at high risk.
This class includes popular medications like semaglutide (available as an injectable, Ozempic, or an oral tablet, Rybelsus), liraglutide (Victoza), and dulaglutide (Trulicity). While most are administered as once-daily or once-weekly injections (often with very fine needles that are easy to use), the availability of an oral option has been a game-changer for some. Common side effects can include nausea, vomiting, or diarrhea, particularly when starting treatment or increasing the dose, but these often subside over time. For many, the profound benefits for blood sugar, weight, and heart health make GLP-1 receptor agonists an incredibly valuable addition to their diabetes management plan.
SGLT2 Inhibitors: Heart, Kidney, and Blood Sugar Protection
Another groundbreaking class of medications that has transformed type 2 diabetes management is SGLT2 inhibitors. These medications work in a uniquely clever way to help your body manage blood sugar. Instead of focusing on insulin production or sensitivity, SGLT2 inhibitors primarily act on your kidneys. Normally, your kidneys reabsorb most of the glucose that filters through them back into your bloodstream. SGLT2 inhibitors, however, block a protein in the kidneys called SGLT2, which is responsible for this reabsorption. By blocking it, these medications cause your kidneys to remove more glucose from your body through your urine, effectively “peeing out” excess sugar and lowering your blood sugar levels.
But the story of SGLT2 inhibitors is much more exciting than just blood sugar reduction. This class of drugs provides robust protection against some of the most serious complications associated with type 2 diabetes. They have been shown to significantly reduce the risk of hospitalization for heart failure, a condition where the heart struggles to pump blood effectively, and they also improve kidney outcomes, slowing the progression of chronic kidney disease in many patients. This “dual protection” for both the heart and kidneys makes them an invaluable treatment option, especially for individuals with existing cardiovascular disease, heart failure, or kidney disease, or those at high risk. As an added benefit, because they help the body excrete sugar and some extra fluid, SGLT2 inhibitors can also contribute to modest weight loss.
Well-known examples in this class include empagliflozin (Jardiance), dapagliflozin (Farxiga), and canagliflozin (Invokana). These are typically taken orally once a day. Common side effects can include an increased risk of urinary tract infections (UTIs) and genital yeast infections, as more sugar in the urine can create a more hospitable environment for bacteria and fungi. Staying well-hydrated is always a good idea, and discussing any symptoms promptly with your doctor is key. Despite these potential side effects, the powerful cardiovascular and renal protective effects, combined with effective blood sugar control, make SGLT2 inhibitors a truly remarkable option for many managing type 2 diabetes.
Other Oral Medications: Complementary and Alternative Options
While Metformin, GLP-1 receptor agonists, and SGLT2 inhibitors often take center stage in modern type 2 diabetes management, several other oral medication classes play vital roles, either as complementary therapies or as alternative options depending on individual needs and circumstances. Each class works differently to help you achieve your blood sugar goals.
* DPP-4 Inhibitors (e.g., Januvia, Tradjenta): These medications work by increasing the levels of natural hormones called “incretins” (like GLP-1) in your body. Incretins help stimulate the pancreas to produce more insulin when blood sugar is high and also reduce the amount of glucose produced by the liver. The key difference from GLP-1 receptor agonists is that DPP-4 inhibitors prevent the breakdown of your *body’s own* incretins, rather than directly mimicking them. They are generally very well-tolerated, have a low risk of hypoglycemia, and are weight-neutral, meaning they typically don’t cause weight gain or loss. They’re often a good choice for those who need moderate A1C reduction and want a medication with minimal side effects.
* Sulfonylureas (e.g., Glipizide, Glyburide): These are older, more traditional medications that have been used for decades. They work by stimulating the beta cells in your pancreas to produce and release more insulin, regardless of your current blood sugar level. They are quite effective at lowering A1C and are generally very affordable. However, because they continuously prompt insulin release, they carry a higher risk of hypoglycemia (low blood sugar) compared to many newer drugs. They can also lead to weight gain, which might be a concern for some individuals. Despite these drawbacks, their effectiveness and cost-efficiency mean they still have a place in certain treatment plans, especially when financial considerations are paramount.
* Thiazolidinediones (TZDs) (e.g., Pioglitazone): TZDs primarily improve insulin sensitivity in the body’s cells, particularly in muscle and fat tissue. This means your body can use the insulin it produces more effectively, allowing glucose to move from your bloodstream into your cells. They offer durable A1C reduction and have been shown to have some beneficial effects on cardiovascular health for certain patients. However, TZDs can cause fluid retention, which may lead to weight gain and can be a concern for individuals with heart failure. They also carry a small risk of bone fractures and a historical association with bladder cancer (though the risk is very low). Your doctor will carefully weigh these factors when considering a TZD for your treatment plan.
Understanding these various options helps illustrate the breadth of tools available to manage type 2 diabetes, each with its own profile of benefits and considerations.
When Insulin Therapy Becomes Necessary
For many individuals with type 2 diabetes, oral medications and injectables like GLP-1 agonists are highly effective in managing blood sugar levels for years. However, sometimes, despite optimizing other therapies, the body’s natural insulin production significantly declines, or insulin resistance becomes too great for other medications to overcome. In these situations, insulin therapy becomes a necessary and incredibly powerful tool to achieve target blood glucose levels. It’s also often initiated at diagnosis if A1C levels are extremely high, indicating that the pancreas is already under significant strain.
Insulin therapy directly replaces the insulin your body isn’t producing or using effectively. It’s essentially giving your body back the crucial hormone it needs to move glucose from your bloodstream into your cells for energy, providing robust and often rapid blood sugar control. Many people initially feel apprehensive about starting insulin, often associating it with “failing” to manage their diabetes or believing it means their condition is much worse. It’s important to understand that this is a common misconception. Starting insulin simply means you’re giving your body the support it needs to stay healthy and prevent complications, and it’s a natural progression for many living with type 2 diabetes.
Modern insulin regimens are incredibly flexible and designed to integrate seamlessly into your life. Options range from once-daily basal insulin, which provides a steady background level of insulin throughout the day, to multiple daily injections (MDI) that combine basal insulin with bolus (mealtime) insulin to cover carbohydrates you eat. For some, advanced options like insulin pump therapy offer continuous insulin delivery and precise dose adjustments. Your healthcare team will work closely with you to determine the type of insulin, the regimen, and the delivery method that best suits your lifestyle, blood sugar patterns, and specific needs, making sure you feel confident and comfortable every step of the way. Insulin is a life-changing therapy that, when used correctly, can significantly improve your health and quality of life.
Navigating the landscape of type 2 diabetes medications can seem complex, but understanding the diverse categories and their unique benefits is key. Remember, there isn’t a single “best” medication, but rather an optimal treatment plan tailored specifically for you. The most important step is to have an open and detailed discussion with your healthcare provider to explore which medications align best with your health goals, lifestyle, and medical history to achieve the most effective diabetes management. By working together with your care team, you can confidently choose the path that leads to better blood sugar control, improved overall health, and a higher quality of life.
Frequently Asked Questions
What are the main types of medications used to manage type 2 diabetes, and how do they work?
Type 2 diabetes medications fall into several categories, each targeting different aspects of blood sugar regulation. Common classes include biguanides (like metformin) which reduce glucose production in the liver, sulfonylureas and meglitinides that stimulate insulin release, and DPP-4 inhibitors which enhance the body’s natural insulin response. SGLT2 inhibitors help kidneys remove more glucose, while GLP-1 receptor agonists slow digestion and increase insulin secretion, offering diverse pathways to achieve optimal glycemic control.
How do doctors determine the best type 2 diabetes medication for an individual patient?
Selecting the best type 2 diabetes medication is a personalized process based on several factors, including the patient’s A1C level, duration of diabetes, other health conditions (like heart disease or kidney issues), potential side effects, and cost. Doctors also consider if a medication offers additional benefits beyond blood sugar control, such as weight loss or cardiovascular protection. The goal is to create a tailored treatment plan that effectively manages blood sugar while minimizing risks and improving overall quality of life.
Why is Metformin often the first-line treatment recommendation for most people with type 2 diabetes?
Metformin is widely recommended as the initial medication for most individuals with type 2 diabetes due to its proven efficacy, favorable safety profile, and affordability. It primarily works by reducing glucose production in the liver and improving insulin sensitivity in muscle cells, helping to lower blood sugar levels without causing weight gain or significant risk of hypoglycemia. Its long-standing track record and cardioprotective benefits in some studies make it a foundational choice in type 2 diabetes management.
Which type 2 diabetes medications offer additional benefits like weight loss or cardiovascular protection?
Several newer type 2 diabetes medications offer significant benefits beyond just blood sugar reduction. GLP-1 receptor agonists (e.g., Ozempic, Trulicity) are known for promoting weight loss and have shown robust cardiovascular benefits, reducing the risk of heart attack, stroke, and cardiovascular death. SGLT2 inhibitors (e.g., Farxiga, Jardiance) also contribute to weight loss and have demonstrated strong protective effects for both the heart and kidneys, making them excellent choices for patients with existing cardiovascular disease or kidney issues.
Are there newer injectable non-insulin medications for type 2 diabetes, and what are their advantages?
Yes, newer injectable non-insulin medications, primarily GLP-1 receptor agonists, have revolutionized type 2 diabetes management. These medications are administered once daily or weekly and work by mimicking a natural hormone that helps regulate blood sugar. Their key advantages include potent A1C reduction, significant weight loss potential, and proven benefits for cardiovascular health, often reducing the risk of major adverse cardiac events. They also generally carry a low risk of hypoglycemia when not used with insulin or sulfonylureas.
References
- https://diabetes.org/health-wellness/medication
- https://www.niddk.nih.gov/health-information/diabetes/overview/medications-treatments
- https://www.cdc.gov/diabetes/managing/medications.html
- Type 2 diabetes – Diagnosis and treatment – Mayo Clinic
- https://en.wikipedia.org/wiki/Type_2_diabetes_medication
- https://medlineplus.gov/type2diabetes.html
- https://my.clevelandclinic.org/health/diseases/4162-type-2-diabetes/management-and-treatment
- https://www.aafp.org/pubs/afp/issues/2019/0715/p99.html


