When it comes to the “best” diet for type 2 diabetes, the optimal approach isn’t a single restrictive plan, but rather a sustainable, whole-foods-focused eating pattern. This involves prioritizing non-starchy vegetables, lean proteins, healthy fats, and carefully managed complex carbohydrates, alongside consistent eating habits, to effectively manage blood sugar levels, support weight management, and reduce the risk of complications. Adopting this holistic approach empowers you to take control of your health, feel energized, and significantly improve your quality of life while navigating type 2 diabetes.
The Foundation: Core Principles of a Type 2 Diabetes Diet

Building a successful eating plan for type 2 diabetes starts with understanding some fundamental principles. These aren’t just rules; they’re guidelines designed to support your body’s natural functions and promote stable blood sugar.
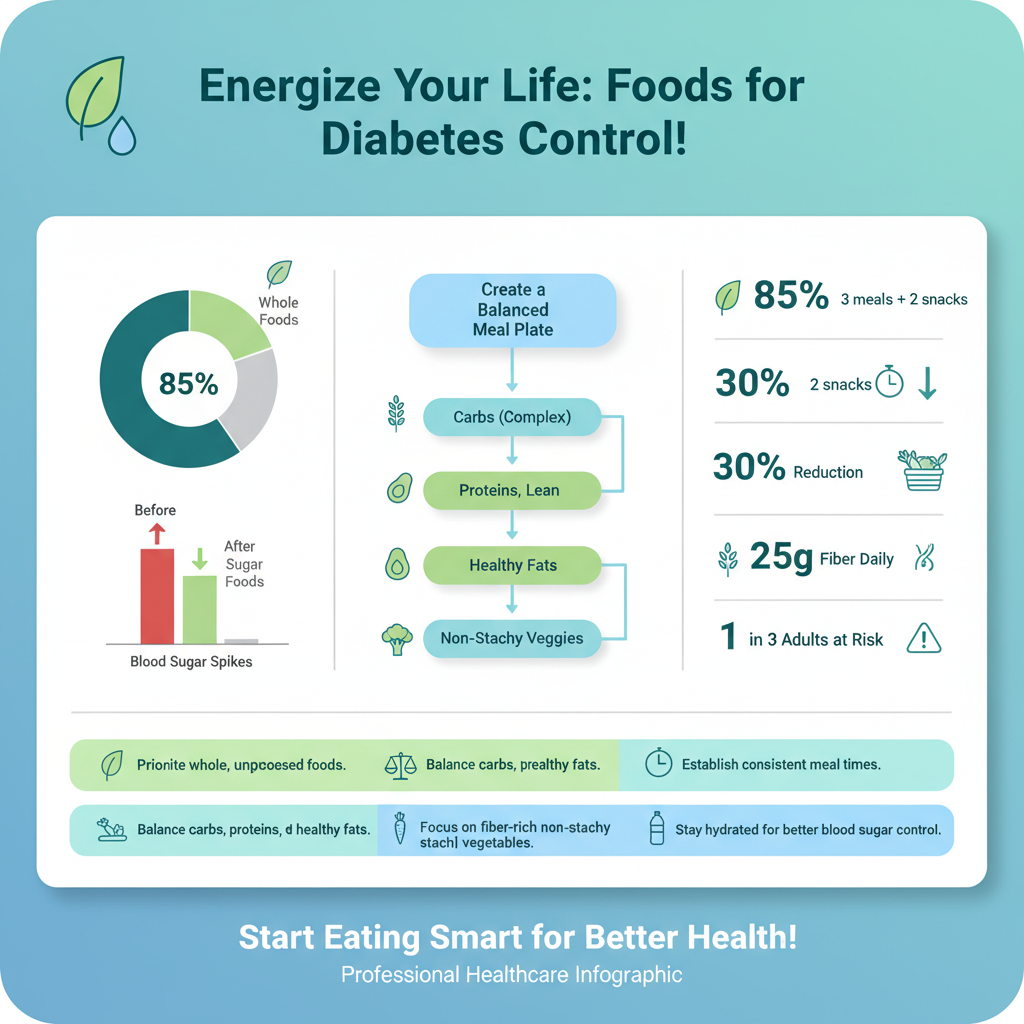
* Focus on Whole, Unprocessed Foods: Think of food as it comes from nature. Prioritizing foods in their most natural state means choosing fresh vegetables, fruits, whole grains, and lean proteins over highly processed options. Why is this so crucial? Whole foods retain their natural fiber, vitamins, and minerals, which are often stripped away during processing. They also tend to have fewer hidden sugars, unhealthy fats, and artificial additives that can wreak havoc on blood sugar levels and overall health. For example, opting for a baked sweet potato instead of processed potato chips, or a piece of grilled chicken instead of a pre-made frozen meal, makes a huge difference. These choices provide sustained energy and better nutritional value, helping you feel fuller for longer and avoid those dreaded energy crashes.
* Balance Macronutrients: At each meal, aim for a balanced intake of carbohydrates, proteins, and healthy fats. This trio works together beautifully to help stabilize blood sugar and maintain satiety, which is that satisfying feeling of fullness. Carbohydrates are your body’s primary energy source, but the *type* and *amount* matter. Pairing complex carbohydrates with protein and healthy fats slows down glucose absorption into the bloodstream, preventing rapid spikes. Protein is vital for muscle repair and keeps you feeling full, while healthy fats contribute to satiety, hormone production, and nutrient absorption. A balanced meal might look like grilled salmon (protein and healthy fats) with a generous serving of steamed broccoli (fiber-rich non-starchy vegetable) and a small portion of quinoa (complex carbohydrate).
* Emphasize Consistent Eating Times: Our bodies thrive on routine, and your blood sugar levels are no exception! Eating regular meals and snacks at consistent times throughout the day can significantly help regulate blood sugar levels. When you go too long without eating, your blood sugar can drop, leading to intense hunger and potentially overeating later. Conversely, erratic eating can make it harder for your body to manage glucose effectively, leading to extreme highs and lows. Aim for three balanced meals and perhaps 1-2 healthy snacks, spread evenly throughout your waking hours. This steady intake helps your body process glucose more efficiently, supports a healthy metabolism, and can even make it easier to stick to your dietary goals by preventing excessive hunger.
Foods to Prioritize for Blood Sugar Control

Now that we understand the core principles, let’s dive into the delicious foods that should be the stars of your plate! These choices are packed with nutrients and work hard to keep your blood sugar steady.
* Abundant Non-Starchy Vegetables and Fruits: These are your best friends in managing type 2 diabetes! Load up on leafy greens (spinach, kale, lettuce), cruciferous vegetables (broccoli, cauliflower, Brussels sprouts), bell peppers, cucumbers, mushrooms, and asparagus. They are incredibly rich in fiber, vitamins, and minerals, yet have minimal impact on blood sugar levels due to their low carbohydrate content. Fruits, especially berries (strawberries, blueberries, raspberries), apples, pears, and citrus fruits (oranges, grapefruit), are also fantastic choices in moderation. They offer natural sweetness, antioxidants, and fiber. Try adding a handful of spinach to your morning eggs, snacking on an apple with a tablespoon of almond butter, or filling half your dinner plate with roasted broccoli and bell peppers.
* Lean Proteins and Healthy Fats: Including sufficient lean proteins and healthy fats is key for satiety, muscle maintenance, and slowing down carbohydrate absorption. Excellent sources of lean protein include fish (especially fatty fish like salmon, mackerel, and tuna, which are also rich in omega-3s), skinless chicken breast, turkey, beans, lentils, and tofu. For healthy fats, reach for nuts (almonds, walnuts), seeds (chia seeds, flax seeds, pumpkin seeds), avocados, and olive oil. These healthy fats are crucial for heart health, which is particularly important for individuals with diabetes. A handful of almonds as a snack, avocado slices added to your salad, or cooking with olive oil instead of butter are simple ways to incorporate these beneficial foods.
* Fiber-Rich Complex Carbohydrates in Measured Portions: Not all carbohydrates are created equal! Unlike refined carbohydrates, fiber-rich complex carbohydrates provide a slow, steady release of glucose into your bloodstream, thanks to their high fiber content. This helps prevent rapid blood sugar spikes. Prioritize whole grains like oats, quinoa, brown rice, barley, and 100% whole-wheat bread or pasta. Sweet potatoes and legumes (like black beans, chickpeas, and kidney beans) are also fantastic complex carb choices. The key here, however, is measured portions. Even healthy carbs can raise blood sugar if consumed in excess. A good rule of thumb is to aim for a serving size equivalent to about a cupped hand. For example, a small bowl of oatmeal for breakfast, or a half-cup of brown rice with your dinner.
Foods to Limit and Avoid

While focusing on what to eat is empowering, it’s equally important to understand what foods can hinder your blood sugar management and overall health. Making informed choices to limit or avoid certain items can have a profound impact.
* Sugary Drinks, Refined Grains, and Processed Snacks: These are often the biggest culprits when it comes to blood sugar spikes and poor health outcomes. Sugary drinks like sodas, fruit juices (even 100% fruit juice can be high in natural sugars without the fiber of whole fruit), sweetened teas, and sports drinks flood your system with sugar very quickly, leading to rapid and dangerous blood glucose elevations. Refined grains, such as white bread, white rice, many breakfast cereals, and pastries, are stripped of their fiber and nutrients, acting much like sugar in your body. Processed snacks like cookies, chips, and candies are not only high in sugar and refined carbs but also often contain unhealthy fats and sodium. Cutting these out is one of the most effective steps you can take for better blood sugar control and weight management.
* Trans Fats and Excessive Saturated Fats: These types of fats are detrimental to heart health, which is a significant concern for people with type 2 diabetes, as they have an increased risk of cardiovascular disease. Trans fats, often found in fried foods, many baked goods (like commercial cakes, cookies, and pies), and some margarines, raise “bad” LDL cholesterol and lower “good” HDL cholesterol. Excessive saturated fats, common in fatty cuts of red meat, full-fat dairy products, and processed meats, can also contribute to unhealthy cholesterol levels. While some saturated fat is okay in moderation, making leaner protein choices and opting for healthy cooking oils like olive or avocado oil can make a big difference for your heart.
* High-Sodium Foods and Excessive Alcohol: Reducing your intake of high-sodium foods is vital for managing blood pressure, which, like heart disease, is a common co-existing condition with diabetes. Many processed meats (like deli meats, bacon, sausage), canned soups, frozen dinners, and convenience foods are packed with hidden sodium. Always check nutrition labels! As for alcohol, excessive consumption can interfere with blood sugar levels, potentially causing dangerous lows (especially if you’re on certain medications) or highs. It can also impact liver function and contribute to weight gain. If you choose to drink, do so in moderation, always with food, and discuss safe limits with your healthcare provider.
Practical Meal Planning & Portion Control
Knowledge is power, but applying that knowledge practically is where the magic happens! Meal planning and mastering portion control are essential skills for managing type 2 diabetes effectively.
* Understand Appropriate Portion Sizes: This is perhaps one of the most critical skills to develop. Even healthy foods can impact blood sugar if consumed in excessive amounts, particularly carbohydrates. Learning to accurately gauge servings of carbohydrates, proteins, and fats prevents overeating and helps maintain blood sugar stability. You don’t need to carry a measuring cup everywhere, but understanding typical serving sizes is key. For example, a portion of protein (like chicken or fish) is about the size of your palm, a serving of cooked carbohydrates (like rice or pasta) is about the size of a cupped hand, and a serving of healthy fat (like nuts or avocado) is roughly the size of your thumb. Using smaller plates can also trick your brain into feeling more satisfied with appropriate portions.
* Read Nutrition Labels Carefully: Nutrition labels are your secret weapon for making informed food choices. Don’t just glance at them; truly understand what you’re looking at. Pay close attention to the serving size and servings per container – these are often smaller than you might assume! Then, check the total carbohydrates, added sugars, fiber content, and types of fats (prioritizing unsaturated fats over saturated and trans fats). A higher fiber content in carbohydrates is generally better as it slows glucose absorption. Be mindful of “sugar-free” claims, as these products can still contain carbohydrates or sugar alcohols that affect blood sugar. Empower yourself by becoming a label-reading expert!
* Plan Meals and Snacks in Advance: Spontaneity can be fun, but when it comes to managing type 2 diabetes, a little planning goes a long way. Prepping meals and having healthy snacks ready can help maintain consistency in your eating schedule, prevent impulsive unhealthy eating choices when hunger strikes, and reduce stress. Dedicate some time each week to plan your meals, create a shopping list, and perhaps do some batch cooking (e.g., cook a large batch of quinoa or chicken breast that can be used for several meals). Keep healthy, pre-portioned snacks like a small handful of nuts, vegetable sticks, or a piece of fruit readily available, so you’re never caught unprepared. This proactive approach saves time, money, and most importantly, supports your health goals.
Beyond Diet: Integrating Lifestyle Factors
While diet is a cornerstone of type 2 diabetes management, it’s just one piece of the puzzle. A truly holistic approach integrates several key lifestyle factors that work synergistically with your eating plan to improve blood sugar control and overall well-being.
* Incorporate Regular Physical Activity: Moving your body is incredibly powerful for diabetes management. Engaging in regular physical activity, which includes both aerobic exercise (like brisk walking, swimming, or cycling) and strength training (using weights or bodyweight exercises), helps improve insulin sensitivity. This means your body’s cells become more responsive to insulin, allowing glucose to enter them more efficiently and lowering blood sugar levels. Exercise also plays a vital role in weight management, stress reduction, and cardiovascular health. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, plus strength training at least twice a week. Even short bursts of activity, like a 10-minute walk after meals, can make a difference!
* Practice Stress Management Techniques: Chronic stress can have a surprisingly significant impact on your blood sugar levels. When you’re stressed, your body releases hormones like cortisol, which can increase glucose production and make your cells more resistant to insulin. This is why incorporating effective stress management techniques into your daily routine is so important. Explore practices like meditation, deep breathing exercises, yoga, spending time in nature, listening to calming music, or engaging in hobbies you enjoy. Finding healthy outlets for stress not only helps regulate your blood sugar but also boosts your mental and emotional well-being, creating a more balanced and resilient you.
* Ensure Adequate Sleep: You might not think of sleep as a diabetes management tool, but it’s crucial! Sufficient quality sleep is fundamental for overall metabolic health. When you don’t get enough sleep, your body’s hormone balance can be thrown off, particularly those that regulate insulin sensitivity, appetite (ghrelin and leptin), and stress hormones. This can lead to increased insulin resistance and higher blood sugar levels the next day, as well as increased cravings for unhealthy foods. Aim for 7-9 hours of consistent, restorative sleep each night. Establish a regular sleep schedule, create a relaxing bedtime routine, and optimize your sleep environment to improve your sleep hygiene.
Partnering with Your Healthcare Team
You don’t have to navigate your type 2 diabetes journey alone. Building a strong support system with your healthcare team is invaluable for personalized guidance and optimal health outcomes.
* Consult a Registered Dietitian: While general guidelines are helpful, every individual’s needs are unique. A Registered Dietitian (RD) is an expert in medical nutrition therapy and can provide personalized meal plans tailored to your specific health needs, preferences, cultural background, and lifestyle. They can educate you on carbohydrate counting, portion control, label reading, and strategies for managing blood sugar spikes. An RD can help you identify trigger foods, overcome dietary challenges, and ensure you’re getting all the necessary nutrients, making your journey much smoother and more effective. Think of them as your personal food coach!
* Monitor Blood Sugar Levels Regularly: Consistent blood sugar monitoring is your direct feedback loop. It helps you understand exactly how different foods, activities, medications, and even stress impact your individual glucose levels. This data is incredibly powerful! By tracking your readings, you and your healthcare team can identify patterns, make timely adjustments to your diet or medication, and gain insight into what works best for *your* body. Whether it’s through finger pricks or a continuous glucose monitor (CGM), regular monitoring empowers you to make informed decisions daily and take proactive steps to maintain healthy ranges.
* Work with Your Doctor for Ongoing Support: Your primary care physician or endocrinologist is the cornerstone of your diabetes management. Regularly discuss your diet, lifestyle habits, medication regimen, and any concerns you have with them. They can monitor your A1C, cholesterol, blood pressure, and kidney function, ensuring that all aspects of your health are being managed effectively and helping to prevent complications. They can also connect you with other specialists, like an ophthalmologist or podiatrist, as needed. Open and honest communication with your doctor ensures you receive the most comprehensive and up-to-date care for your condition.
Adopting the best type 2 diabetes diet is about making informed, sustainable choices that support your health long-term. By focusing on nutrient-dense whole foods, managing carbohydrate intake, limiting harmful ingredients, and incorporating vital lifestyle changes like exercise, stress management, and adequate sleep, you can effectively manage your condition and significantly improve your quality of life. Remember, this journey is best taken with professional guidance; consult your doctor or a registered dietitian to create a personalized eating plan that fits your unique needs and helps you thrive. Your commitment to these principles is an investment in your health and a vibrant future.
Frequently Asked Questions
What is the single “best” type 2 diabetes diet for managing blood sugar effectively?
There isn’t one “best type 2 diabetes diet” that fits everyone, as individual needs vary. However, the most effective approach emphasizes a balanced eating pattern rich in whole, unprocessed foods like vegetables, lean proteins, healthy fats, and complex carbohydrates. The goal is to create a sustainable, personalized diet plan that helps manage blood sugar levels, support a healthy weight, and prevent complications.
How can I effectively control my blood sugar levels through specific dietary choices?
To effectively control blood sugar levels, prioritize foods with a low glycemic index and high fiber content, such as non-starchy vegetables, legumes, and whole grains. Focus on consistent carbohydrate intake throughout the day and pair carbs with protein and healthy fats to slow glucose absorption. Limiting added sugars and refined carbohydrates is crucial for preventing sharp blood sugar spikes.
Which specific foods should be limited or avoided when following a type 2 diabetes diet?
When managing type 2 diabetes through diet, it’s generally recommended to limit or avoid foods high in refined carbohydrates, added sugars, and unhealthy fats. This includes sugary drinks, candies, pastries, white bread, white rice, and highly processed snacks. Reducing saturated and trans fats found in fried foods and some processed meats is also important for heart health.
Why is a focus on whole, unprocessed foods so crucial for a type 2 diabetes diet?
Whole, unprocessed foods are crucial for a type 2 diabetes diet because they are naturally rich in fiber, vitamins, and minerals, which support overall health and improve blood sugar control. Their fiber content helps slow the absorption of sugar into the bloodstream, preventing rapid spikes and promoting stable energy levels. This approach also aids in weight management, a key factor in improving insulin sensitivity.
What are practical strategies for portion control and meal planning to support a type 2 diabetes diet?
Practical strategies for portion control include using smaller plates, measuring food portions, and being mindful of serving sizes, especially for carbohydrate-rich foods. For meal planning, aim for balanced plates that prioritize non-starchy vegetables, include a lean protein source, and incorporate a modest serving of complex carbohydrates. Consistent meal times and planning snacks can also prevent overeating and help maintain stable blood sugar throughout the day.
References
- https://diabetes.org/healthy-living/recipes-nutrition/diabetes-meal-plans-and-a-healthy-diet
- https://www.cdc.gov/diabetes/managing/eat-well.html
- Healthy Living with Diabetes – NIDDK
- Diabetes diet: Create your healthy-eating plan – Mayo Clinic
- https://www.hsph.harvard.edu/nutritionsource/disease-prevention/type-2-diabetes/diet-and-type-2-diabetes/
- https://my.clevelandclinic.org/health/articles/11267-diabetes-diet-what-to-eat-and-what-to-avoid
- https://www.nhs.uk/conditions/type-2-diabetes/eating-well/
- Type 2 diabetes