The best times to check blood sugar for type 2 diabetes are typically first thing in the morning (fasting), just before meals, and one to two hours after eating. Testing at these specific intervals provides a complete picture of how your body manages glucose throughout the day, though your healthcare provider will ultimately determine your specific schedule based on your medications and treatment goals. Effective diabetes management relies heavily on data; without frequent monitoring at strategic times, both the patient and the medical provider are essentially operating in the dark. By adhering to a structured testing schedule, you transform a daily chore into a powerful analytical tool that informs dietary choices, medication adjustments, and long-term health strategies.
First Thing in the Morning (Fasting)

Testing your blood sugar immediately upon waking is arguably the most critical data point of the day. This measurement, known as the fasting plasma glucose test, checks your baseline glucose level after an 8-hour sleep period without food. It provides a clear indication of how your body maintains homeostasis when no external fuel sources are being introduced. For many with type 2 diabetes, the target fasting range is typically between 80 and 130 mg/dL, though individual targets may vary based on age and duration of the condition.
This morning check is particularly vital for identifying distinct physiological phenomena that affect glucose regulation. Specifically, it helps identify if you are experiencing the “dawn phenomenon”—a natural rise in blood sugar caused by the release of hormones like cortisol and growth hormone in the early morning hours. Alternatively, high morning numbers could indicate the Somogyi effect, where blood sugar drops too low during the night, triggering a rebound spike. By consistently recording your fasting numbers, you provide your healthcare team with the evidence needed to distinguish between these conditions, allowing them to adjust evening medication dosages or recommend bedtime snack alterations to stabilize overnight levels.
Before Meals and Snacks
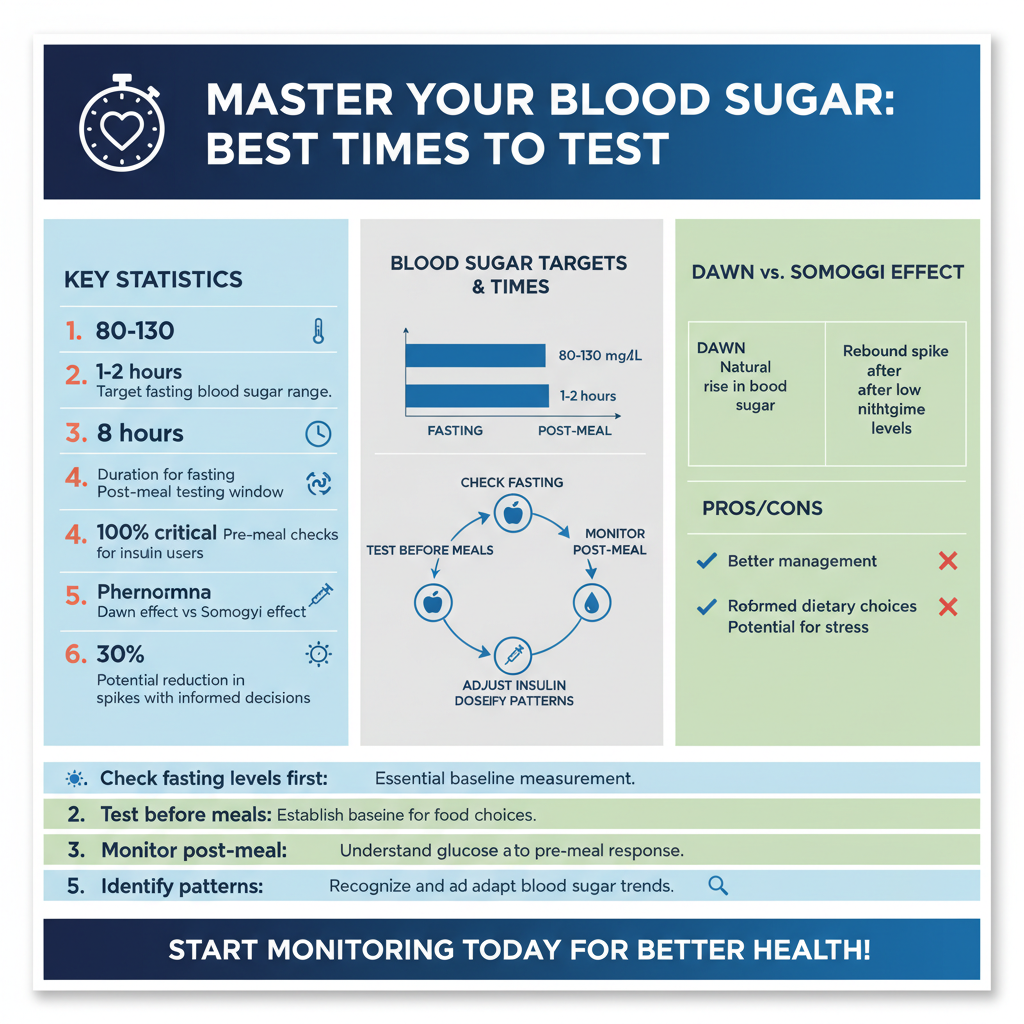

Checking your glucose levels before eating establishes a baseline number before you introduce new carbohydrates into your system. This “pre-prandial” reading serves as a navigational tool, allowing you to make informed decisions about the meal you are about to consume. If your pre-meal blood sugar is already elevated—perhaps due to stress or a lack of activity earlier in the day—you might choose to reduce your carbohydrate intake for that specific meal or opt for foods with a lower glycemic index to prevent a dangerous spike.
For patients utilizing insulin therapy, this testing window is non-negotiable. It helps you calculate insulin doses precisely, ensuring that the amount of insulin administered matches both the current blood sugar level and the anticipated carbohydrate intake. Even for those managing diabetes solely through oral medications or lifestyle changes, pre-meal testing reinforces the connection between behavior and biology. It encourages a moment of pause and assessment, shifting the patient from passive consumption to active management. Consistently high pre-meal numbers may suggest that the previous meal was too heavy in carbohydrates or that basal insulin or long-acting medications need adjustment.
One to Two Hours After Meals

While pre-meal numbers set the stage, testing one to two hours after the first bite of food measures how well your body handled the carbohydrates consumed during the meal. This is known as postprandial glucose testing. For most adults with diabetes, the American Diabetes Association recommends a target of less than 180 mg/dL at this interval. This specific timeframe captures the peak glucose concentration, offering insight into your body’s immediate insulin response (or lack thereof).
This testing time is the most effective method for identifying specific trigger foods that cause sharp spikes in your blood sugar levels. For example, you may discover that your body processes a sweet potato reasonably well, resulting in a modest rise, whereas white pasta causes a rapid and sustained spike. These insights allow for “precision nutrition.” Rather than following a generic diet plan, you can curate a menu based on your unique metabolic responses. If you consistently notice spikes two hours after eating despite healthy food choices, it may signal to your physician that your rapid-acting insulin or mealtime oral medications are insufficient to cope with your dietary intake.
Before Bedtime
Testing before sleep ensures your glucose levels are stable enough to sleep safely through the night without dropping too low. Nocturnal hypoglycemia (low blood sugar while sleeping) is a significant concern, particularly for those taking insulin or sulfonylureas. A bedtime check provides peace of mind; if levels are trending low (e.g., below 100 mg/dL for some patients), a small snack containing protein and complex carbohydrates can be consumed to sustain glucose levels until morning.
Furthermore, this data point provides context for your morning fasting numbers. It helps manage overnight highs if your morning fasting numbers are consistently elevated. If you go to bed with a normal blood sugar level but wake up high, the issue lies in the body’s overnight regulation (such as the dawn phenomenon discussed earlier). However, if you go to bed with high blood sugar, the morning high is simply a continuation of unresolved hyperglycemia from the evening. Understanding this distinction is crucial for your medical team to prescribe the correct intervention, such as changing the timing of evening medication or adjusting dinner composition.
During Exercise and Physical Activity
Physical activity acts as a potent insulin sensitizer, meaning it helps your muscles use glucose more effectively. However, the relationship between exercise and blood sugar is complex. Testing before working out prevents hypoglycemia during physical exertion. If your starting blood sugar is too low (typically below 100 mg/dL), engaging in cardio could lead to a rapid drop, causing dizziness, fainting, or more severe complications. Conversely, if blood sugar is excessively high (above 250 mg/dL) and ketones are present, exercise can be dangerous and potentially induce ketoacidosis.
Checking after exercise helps you understand how different activities impact your glucose sensitivity. While aerobic exercises like walking or jogging typically lower blood sugar, high-intensity interval training or heavy weightlifting can sometimes trigger a temporary stress response that raises blood sugar due to adrenaline release. By monitoring before and after your sessions, you can learn how your body reacts to different modalities. This allows you to plan workout snacks appropriately and time your exercise sessions for when they will be most beneficial for lowering daily glucose averages.
When You Feel Unwell or Stressed
Physiological and psychological stressors act as major disruptors to glucose regulation. Illness, infection, and high stress can cause blood sugar to rise unpredictably. When the body fights an illness, it releases hormones like cortisol and epinephrine to combat the stressor; unfortunately, these hormones also render cells more resistant to insulin. Consequently, a patient with type 2 diabetes may experience stubborn hyperglycemia during a flu or infection, even if they have lost their appetite and are eating very little.
Therefore, more frequent monitoring is required during “sick days” to prevent hyperglycemia or ketoacidosis. Standard protocol often suggests testing every two to four hours when ill. This vigilance allows for the early detection of dangerous trends. If blood sugar levels remain persistently high despite medication, or if you experience symptoms such as extreme thirst, frequent urination, or confusion, immediate medical intervention may be required. Similarly, periods of intense emotional stress or trauma warrant closer monitoring, as stress management techniques may need to be integrated with medical adjustments to restore glycemic control.
Monitoring your blood sugar at these strategic times is the most effective way to manage type 2 diabetes and prevent long-term complications. These numbers are more than just data points; they are a direct communication from your body regarding its metabolic state. Always record your numbers to share with your healthcare team, as these patterns allow them to adjust your medication or lifestyle recommendations for optimal health. By observing the trends across fasting, mealtime, and activity windows, you and your provider can move beyond reactive symptom management toward proactive, precision health optimization.
Frequently Asked Questions
What are the best times of day to check blood sugar for Type 2 diabetes?
The most critical times to check your blood glucose are typically first thing in the morning (fasting), before meals, and two hours after eating. Monitoring at these specific intervals provides a complete picture of your body’s baseline levels and how well it processes carbohydrates throughout the day. Your healthcare provider may also suggest testing before exercise or at bedtime depending on your medication regimen.
How long after eating is the right time to test for post-meal spikes?
Medical experts generally recommend testing your blood sugar exactly two hours after the start of your meal, known as the postprandial reading. Testing at the two-hour mark is crucial because it indicates how well your body handled the meal’s sugar load and whether your glucose levels are returning to a healthy range. If you test too soon, such as 30 minutes after eating, you may see a natural spike that doesn’t accurately reflect your diabetes management.
Why is checking fasting blood sugar in the morning so important?
Testing immediately upon waking gives you a fasting baseline that reveals how your body manages blood sugar after a long period without food. Consistently high morning readings can alert you to the “Dawn Phenomenon”—a natural hormone surge that raises glucose—or indicate that your current evening medication or snack habits need adjustment. This data point is often the primary indicator used to adjust long-acting insulin or oral medications.
Should I check my blood sugar levels before going to sleep?
Checking blood glucose at bedtime is highly advisable, especially if you take insulin or medications that stimulate insulin production, to ensure you are not at risk of nocturnal hypoglycemia (low blood sugar overnight). A bedtime reading also serves as a valuable comparison point for your morning fasting result, helping you understand what happens to your glucose levels while you sleep.
How does exercise affect when I should test my blood sugar?
You should test your blood sugar both before and after physical activity to understand how different workouts impact your levels. For safety, checking before a workout ensures your levels aren’t too low to exercise safely or too high to risk ketoacidosis. Checking afterward helps you identify delayed drops in blood sugar, which can occur several hours after intense physical exertion.
References
- https://www.cdc.gov/diabetes/managing/managing-blood-sugar/bloodglucosemonitoring.html
- Blood sugar testing: Why, when and how – Mayo Clinic
- Diabetes Tests | ADA
- Managing Diabetes – NIDDK
- https://my.clevelandclinic.org/health/treatments/17956-blood-glucose-monitoring
- Blood Glucose Test: MedlinePlus Medical Test
- https://www.nhs.uk/conditions/diabetes/living-with/checking-blood-sugar/
- https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/blood-glucose-monitoring