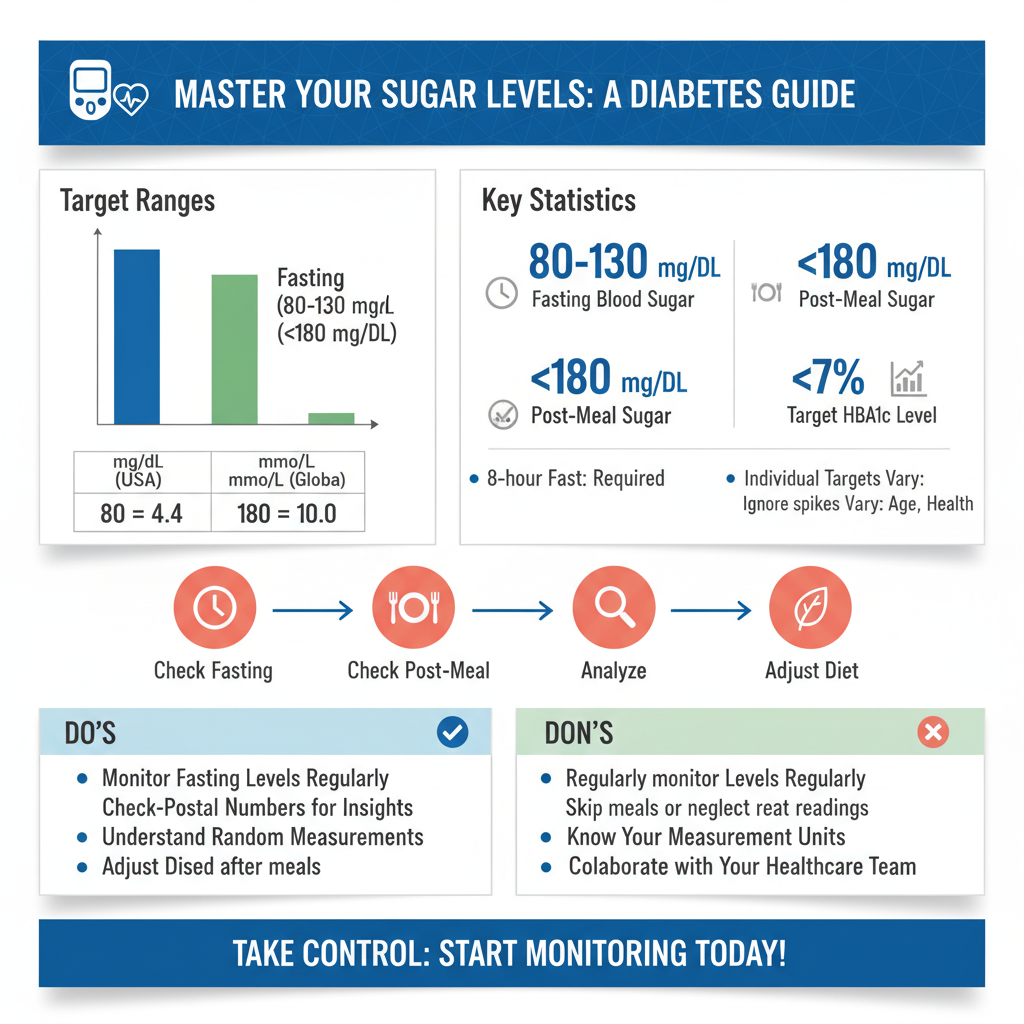
For most adults with diabetes, the best sugar levels typically aim for a fasting blood sugar between 80-130 mg/dL (4.4-7.2 mmol/L), and less than 180 mg/dL (10.0 mmol/L) two hours after starting a meal. Additionally, a target HbA1c below 7% (53 mmol/mol) is generally recommended. Achieving and maintaining these target ranges is crucial for managing diabetes and preventing complications, though individual targets may vary based on age, duration of diabetes, and other health conditions. Understanding these numbers and how to influence them is a cornerstone of living well with diabetes, empowering you to make informed daily choices that support your long-term health.
Understanding Blood Sugar Measurements

Navigating the world of diabetes management often starts with understanding your blood sugar numbers. It’s like having a dashboard for your body, giving you immediate feedback on how your choices affect your health.
* Key Blood Sugar Types: When you check your blood sugar, you’re usually looking at one of a few key measurements, each telling you something a little different about your body’s glucose management.
* Fasting Blood Sugar: This is your glucose level after not eating or drinking anything (except water) for at least 8 hours. It’s typically checked first thing in the morning before breakfast. This measurement is super important because it shows how well your body manages glucose when it’s not processing food. A consistently high fasting sugar can indicate that your body isn’t producing enough insulin or isn’t using it effectively overnight.
* Post-meal Blood Sugar (Postprandial): This measures your blood sugar levels after eating. It’s commonly checked one or two hours after the start of a meal. These readings are invaluable for understanding how specific foods, portion sizes, and carbohydrate counts impact your glucose levels. They help you pinpoint which meals might be causing spikes and guide your dietary adjustments.
* Random Blood Sugar: As the name suggests, this is a blood sugar measurement taken at any time, regardless of when you last ate. While not as specific for pattern analysis as fasting or post-meal readings, a random blood sugar check can still be useful, especially if you’re experiencing symptoms of high or low blood sugar, providing an immediate snapshot of your current glucose status.
* Units of Measure: It can sometimes feel like a puzzle with different countries using different units, but don’t worry, it’s easy to get the hang of it!
* In the United States and a few other countries, blood sugar is measured in milligrams per deciliter (mg/dL).
* In many other parts of the world, including Canada, the UK, Europe, and Australia, it’s measured in millimoles per liter (mmol/L).
While the numbers look different, they represent the same thing. Your healthcare team will always communicate your targets in the unit common to your region, so you’ll quickly become familiar with what feels right for you.
* HbA1c: A Long-Term View: Think of your daily blood sugar checks as snapshots, while your HbA1c (often just called A1c) is like a video reel of your glucose management over time. This crucial test provides an average blood sugar level over the past 2-3 months. How? It measures the percentage of your red blood cells that have sugar coating them. Since red blood cells live for about 2-3 months, this test offers a broader picture of how well your diabetes is being controlled consistently, beyond just your daily fluctuations. It’s an excellent indicator of your overall risk for diabetes-related complications.
Ideal Target Ranges: What to Aim For

Having specific targets gives you a clear roadmap for managing your diabetes effectively. These ranges are generally recommended for most adults, but remember, your personal targets might be slightly different – always a good chat to have with your doctor!
* Pre-meal (Fasting) Targets: For most adults with diabetes, the goal is often between 80-130 mg/dL (4.4-7.2 mmol/L). Achieving this range for your fasting blood sugar is a fantastic sign that your body is managing glucose well overnight and between meals. It indicates that your medication (if you take it), lifestyle choices, and overall health are working in harmony to prevent excessive glucose buildup. Consistently hitting this target can significantly reduce your risk of long-term complications.
* Post-meal Targets: Generally, blood sugar should be less than 180 mg/dL (10.0 mmol/L) one to two hours after starting a meal. This target is vital because it reflects how your body handles the carbohydrates and sugars you consume. If your post-meal numbers are consistently higher than this, it might suggest that your meal choices, portion sizes, or medication dosages need adjustment. Keeping these spikes in check is crucial for protecting your blood vessels and organs over time. Regularly monitoring your post-meal numbers can help you identify trigger foods and refine your eating habits for better control.
* Bedtime Targets: Aiming for 100-140 mg/dL (5.6-7.8 mmol/L) before bed can help prevent overnight lows (hypoglycemia) or highs (hyperglycemia). Going to bed with very low blood sugar can lead to disruptive and potentially dangerous nighttime lows, while going to bed too high can mean you wake up with elevated sugars and might feel tired or unwell. A stable bedtime glucose level helps ensure a safer and more restful night, contributing to better overall well-being and more manageable morning readings. This target is particularly important for individuals on insulin or certain oral medications that carry a risk of hypoglycemia.
The Importance of HbA1c for Long-Term Control

While daily finger pricks give you immediate feedback, the HbA1c test offers a powerful perspective on your diabetes management over the long haul. It’s a key indicator that truly reflects your commitment and the effectiveness of your treatment plan.
* Average Over Time: As we discussed, your HbA1c isn’t just a single snapshot; it reflects your average blood glucose over a couple of months. This makes it incredibly valuable for assessing how well your diabetes is managed consistently. It gives both you and your healthcare team a comprehensive overview, highlighting trends and the overall success of your strategies (or areas that need improvement). For example, if your daily readings are often within target, but your A1c is high, it might suggest unnoticed spikes at other times, or perhaps you’re only checking at convenient times.
* General Target: For most adults with diabetes, a target HbA1c of less than 7% (53 mmol/mol) is often recommended. Achieving and maintaining an A1c below this threshold is strongly associated with a reduced risk of developing or worsening long-term diabetes complications, such as heart disease, kidney disease, nerve damage (neuropathy), and eye problems (retinopathy). It’s a powerful goal that motivates many to stay on track with their treatment. Think of it as your long-term health report card.
* Individualized Goals: While <7% is a general guideline, it’s crucial to understand that your HbA1c target might be different. Your doctor will consider various factors like your age, how long you've had diabetes, the presence of other health conditions (like heart disease or kidney issues), your risk of severe hypoglycemia, and your overall health and life expectancy. For example, older adults or those with a history of severe lows might have a slightly higher, more relaxed A1c target (e.g., <8%) to prioritize safety and quality of life. Conversely, some individuals with newly diagnosed diabetes and no significant complications might aim for an even tighter control, closer to non-diabetic levels, if it can be achieved safely. Always discuss your specific A1c goal with your healthcare provider.
Key Factors Influencing Your Blood Sugar
Your blood sugar levels are dynamic and influenced by a multitude of factors throughout your day. Understanding these can help you better anticipate fluctuations and make proactive adjustments.
* Dietary Choices: This is perhaps the most immediate and impactful factor. What and when you eat plays a huge role in your blood glucose.
* Carbohydrate Intake: Carbohydrates are the primary nutrient that breaks down into glucose. The amount of carbs you eat directly affects how high your blood sugar will rise. Learning to count carbohydrates and understand portion sizes is a game-changer for many.
* Types of Food: Not all carbs are created equal! Simple carbohydrates (like sugary drinks, white bread, candy) cause faster and higher blood sugar spikes compared to complex carbohydrates (like whole grains, vegetables, legumes), which digest more slowly. Fiber-rich foods also help slow down sugar absorption.
* Meal Timing: Eating consistently timed meals can help keep your blood sugar more stable. Skipping meals or eating very large meals can lead to erratic readings.
* Physical Activity: Exercise is a powerful tool for managing diabetes, but its impact can vary.
* Lowering Blood Sugar: Regular physical activity generally lowers blood sugar by increasing insulin sensitivity and allowing your muscles to use glucose for energy, even without insulin. Aerobic exercises like walking, swimming, or cycling are particularly effective.
* Intense or Prolonged Activity: Sometimes, very intense exercise can temporarily *raise* blood sugar due to the release of stress hormones. Prolonged activity, especially without adequate carbohydrate intake, can lead to delayed hypoglycemia hours later. It’s crucial to monitor your blood sugar before, during, and after exercise, and discuss necessary adjustments to your food or medication with your doctor.
* Medications and Other Factors: Beyond diet and exercise, several other elements can significantly affect your glucose levels.
* Insulin and Oral Diabetes Medications: These are designed specifically to help lower blood sugar. Taking them as prescribed is paramount. Missing a dose or taking an incorrect dose can lead to high or low readings.
* Stress: Emotional or physical stress (like from an illness, surgery, or even just a tough day at work) triggers the release of hormones that can raise blood sugar.
* Illness: When you’re sick, your body releases hormones to fight infection, which can cause your blood sugar to rise, even if you’re not eating much. This is why “sick day rules” are important for diabetes management.
* Sleep Quality: Poor sleep can impact insulin sensitivity and stress hormones, potentially leading to higher blood sugar levels. Aim for consistent, quality sleep.
* Hormonal Changes: Women might notice fluctuations during their menstrual cycle or menopause.
* Other Medications: Some non-diabetes medications (like steroids) can also impact blood sugar. Always discuss all your medications with your doctor.
Effective Blood Sugar Monitoring Strategies
Monitoring your blood sugar isn’t just about getting a number; it’s about gathering information to make better decisions. The more insights you have, the better equipped you are to manage your diabetes proactively.
* Regular Glucometer Use: Your traditional finger-prick glucometer is your direct access to real-time blood sugar levels. Learning *when* and *how often* to check is key to identifying patterns.
* When to Check: Common times include first thing in the morning (fasting), before meals, one or two hours after starting a meal, before and after exercise, before bed, and if you suspect a low or high. Your doctor will provide a personalized testing schedule based on your type of diabetes, medications, and overall control.
* How to Use the Data: Each reading is a piece of a puzzle. A high post-meal reading might suggest a need to adjust your carbohydrate intake for that meal, while a consistent low before lunch could indicate too much morning medication. Regular checks empower you to react appropriately and learn how your body responds.
* Continuous Glucose Monitors (CGMs): For many, CGMs have revolutionized blood sugar management. These small, wearable devices automatically measure glucose levels every few minutes, providing real-time data without constant finger pricks (though some still require calibration with a finger prick).
* Real-time Data and Trend Analysis: CGMs show you not just your current glucose level, but also the direction it’s heading (up, down, or stable) and how fast. This trend information is incredibly powerful. You can see how a specific food impacts your glucose over several hours, or how exercise affects it.
* Alerts and Alarms: Many CGMs offer customizable alerts for high or low blood sugar, allowing you to take action before levels become dangerous.
* Comprehensive View: CGMs provide a fuller picture of your glucose fluctuations throughout the day and night, including periods you wouldn’t typically measure with a traditional meter. This can help identify previously unnoticed highs or lows. Discuss with your healthcare team if a CGM might be a good option for you.
* Logging and Pattern Recognition: Simply taking readings isn’t enough; you need to make sense of them!
* Keep a Detailed Log: Whether it’s a paper journal, a smartphone app, or a feature built into your glucometer/CGM, consistently log your readings. But don’t stop there! Also note down:
* Food Intake: What you ate, how much, and the approximate carbohydrate count.
* Physical Activity: Type, duration, and intensity of exercise.
* Medications: Doses and times.
* Other Factors: Stress levels, illness, unusual events.
* Pinpoint Influences: Over time, reviewing your log will help you identify clear patterns. You might notice that certain foods always cause a spike, or that your morning walks consistently lower your fasting sugar. This data is your personal “diabetes detective kit,” helping you and your healthcare team make informed adjustments to your diet, exercise, and medication plan.
When to Consult Your Healthcare Team
Your diabetes journey is a partnership between you and your healthcare team. Knowing when to reach out is just as important as knowing your numbers. They are your expert guides in navigating the complexities of diabetes management.
* Persistent High or Low Readings: If you frequently experience hyperglycemia (blood sugar consistently above your target range) or hypoglycemia (blood sugar consistently below your target range), it’s a clear signal to seek medical advice.
* High Blood Sugar (Hyperglycemia): Persistent highs can indicate that your current treatment plan isn’t quite right, or that other factors (like stress or illness) are having a significant impact. Ignoring them increases your risk of complications.
* Low Blood Sugar (Hypoglycemia): Frequent or severe lows can be dangerous and disruptive. They might suggest your medication dose is too high, or that your meal or activity plan needs adjustment. Don’t hesitate to contact your doctor if you’re struggling with lows.
* Medication or Lifestyle Adjustments: Your doctor, alongside a registered dietitian or certified diabetes educator, is your best resource for fine-tuning your treatment.
* Changing Needs: Your body’s needs change over time. What worked last year might not be optimal today. Don’t try to make significant medication changes on your own.
* Diet and Exercise Plan: If you’re struggling to meet your targets despite your best efforts, your healthcare team can help modify your diet plan, introduce new exercise strategies, or explore different medication options. They can also help troubleshoot specific challenges you’re facing.
* Personalized Goal Setting: Regularly reviewing your individual blood sugar targets and management plan with your healthcare provider is essential. Your goals aren’t set in stone. As your health status changes, or as new treatments become available, your targets might need to be re-evaluated. This ongoing dialogue ensures that your diabetes management plan remains aligned with your overall health, lifestyle, and evolving needs, empowering you to live your healthiest life with diabetes.
Maintaining optimal blood sugar levels is a cornerstone of effective diabetes management, significantly reducing the risk of complications and enhancing your overall quality of life. While general targets provide a good starting point and valuable guidance, remember that your personal “best sugar levels” are unique and should always be determined in close consultation with your healthcare provider. Regularly monitor your levels, understand the myriad factors that influence them, and work collaboratively with your medical team to achieve and sustain your individualized goals for a healthier, happier future. Your commitment to understanding and managing your numbers is the most powerful step you can take for your long-term well-being.
Frequently Asked Questions
What are the recommended target blood sugar levels for people with diabetes?
Generally, for most non-pregnant adults with diabetes, a fasting blood sugar level before meals is targeted between 80-130 mg/dL (4.4-7.2 mmol/L). One to two hours after starting a meal, the goal is typically less than 180 mg/dL (10.0 mmol/L). The A1c target, which reflects average blood sugar over 2-3 months, is usually less than 7%, but individual goals may vary based on age, duration of diabetes, and other health conditions. Always consult your healthcare provider to determine your personalized best sugar levels for diabetes management.
Why is it crucial to maintain blood sugar levels within the recommended range?
Keeping blood sugar levels within your personalized target range is vital to prevent both immediate and long-term diabetes complications. Consistently high blood sugar can lead to serious issues like heart disease, kidney damage, nerve damage (neuropathy), and vision loss over time. Conversely, consistently low blood sugar (hypoglycemia) can be immediately dangerous, causing confusion, dizziness, seizures, or even loss of consciousness. Effective management of blood sugar levels significantly improves quality of life and reduces the risk of these severe health problems.
How do diet and exercise impact the best blood sugar levels for diabetes management?
Diet and exercise are cornerstones of achieving and maintaining healthy blood sugar levels. A balanced diet, focusing on whole foods, lean proteins, healthy fats, and complex carbohydrates with controlled portions, helps regulate glucose absorption and prevents sharp spikes. Regular physical activity enhances insulin sensitivity, meaning your body’s cells can more effectively use insulin to take up glucose for energy, thereby lowering blood sugar. Combining consistent healthy eating and regular exercise is key for optimal diabetes control and can significantly improve your best sugar levels.
When should a person with diabetes contact their doctor about their blood sugar levels?
You should contact your doctor if you experience persistent blood sugar readings that are significantly outside your target range, whether consistently too high (hyperglycemia) or too low (hypoglycemia). Urgent medical attention is needed for severe symptoms of hypoglycemia (e.g., confusion, unconsciousness) or hyperglycemia (e.g., extreme thirst, frequent urination, fruity breath, nausea, vomiting, confusion). Any unexplained or frequent fluctuations in your blood sugar, or concerns about your current diabetes medication or management plan, warrant a discussion with your healthcare provider for guidance and potential adjustments.
Are the target blood sugar levels different for various types of diabetes or specific populations (e.g., pregnant women)?
Yes, the “best” blood sugar levels for diabetes can indeed vary significantly depending on the type of diabetes, age, overall health, and specific life circumstances. For instance, target ranges might be tighter for pregnant women with gestational diabetes or pre-existing diabetes to protect both mother and baby. Children and older adults may have different goals to prevent hypoglycemia or manage other health conditions. Your healthcare team will work with you to establish individualized blood sugar goals that are safe and effective for your unique situation, making personalized care crucial for optimal diabetes management.
References
- Diabetes Tests | ADA
- https://www.cdc.gov/diabetes/managing/manage-blood-sugar.html
- https://www.niddk.nih.gov/health-information/diabetes/overview/managing-diabetes/blood-glucose-monitoring-treatment
- Blood sugar testing: Why, when and how – Mayo Clinic
- https://www.nhs.uk/conditions/type-2-diabetes/blood-sugar-levels/
- Blood sugar level
- How to check your blood sugar levels | Diabetes testing | Diabetes UK