When it comes to the “best” medicine for type 2 diabetes, there’s no single perfect pill; instead, effective management always involves a personalized strategy, combining lifestyle changes with pharmacological interventions tailored to individual needs. The most commonly prescribed and highly effective medications often include metformin, SGLT2 inhibitors, GLP-1 receptor agonists, and sometimes insulin, each working through distinct mechanisms to control blood sugar, mitigate complications, and significantly improve long-term health outcomes. Navigating the various treatment options for type 2 diabetes can indeed be complex, but understanding the primary medications available is a crucial step towards taking charge of your health.
Metformin: The First-Line Treatment

Metformin stands as the long-standing cornerstone of type 2 diabetes treatment, often being the very first medication prescribed by healthcare providers. Its enduring popularity is due to its robust effectiveness in lowering blood sugar, its affordability, and a generally favorable safety profile that has been extensively studied over decades. The medication primarily works by decreasing the amount of glucose (sugar) produced by the liver, which is a major contributor to high fasting blood sugar levels in people with type 2 diabetes. Additionally, metformin plays a vital role in improving insulin sensitivity in the body’s tissues, allowing cells to utilize insulin more effectively to absorb glucose from the bloodstream.
While highly effective, it’s common for individuals starting metformin to experience some gastrointestinal issues such as nausea, diarrhea, or stomach upset. The good news is that these side effects are often temporary and tend to improve over time as your body adjusts to the medication. To minimize discomfort, doctors often recommend starting with a low dose and gradually increasing it, or prescribing extended-release formulations of metformin, which can be gentler on the digestive system. Taking metformin with meals can also significantly help in alleviating these common side effects, making the treatment more manageable.
SGLT2 Inhibitors: Kidney and Cardiovascular Benefits
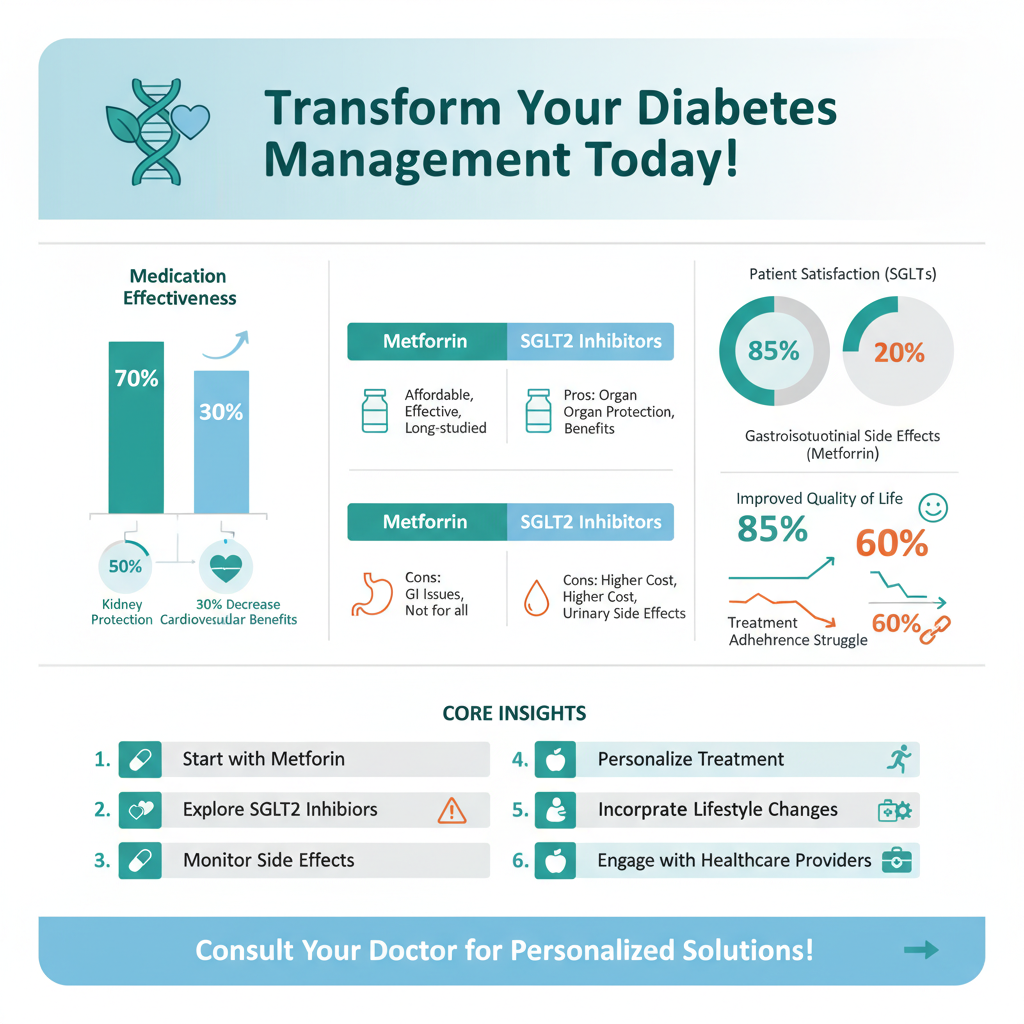

SGLT2 inhibitors represent a relatively newer and incredibly exciting class of drugs that have revolutionized type 2 diabetes management due to their unique mechanism of action and impressive broader health benefits. Medications like empagliflozin (Jardiance), dapagliflozin (Farxiga), and canagliflozin (Invokana) work by targeting the kidneys, specifically inhibiting a protein called SGLT2. This inhibition leads to the kidneys removing more glucose from the body and expelling it through urine, thereby lowering blood sugar levels independently of insulin.
Beyond their powerful blood sugar-lowering effects, SGLT2 inhibitors have garnered significant attention for their remarkable “organ-protective” properties. Clinical trials have consistently shown that these medications offer substantial benefits in reducing the risk of heart failure hospitalizations, major cardiovascular events like heart attacks and strokes, and slowing the progression of kidney disease. This makes them a particularly strong choice for patients who have existing cardiovascular disease, heart failure, or chronic kidney disease, offering a multi-faceted approach to health management. However, because they cause glucose excretion in urine, potential side effects can include an increased risk of urinary tract infections (UTIs), yeast infections (especially in women), and dehydration. Staying well-hydrated and practicing good hygiene can help mitigate these risks.
GLP-1 Receptor Agonists: Weight Loss and Heart Protection

GLP-1 receptor agonists are another transformative class of medications that have added significant value to the diabetes treatment landscape, available in both injectable (like semaglutide, liraglutide, dulaglutide) and, more recently, oral (oral semaglutide) forms. These medications mimic the action of a natural gut hormone called glucagon-like peptide-1 (GLP-1), which plays a crucial role in glucose metabolism. By stimulating GLP-1 receptors, these drugs promote the pancreas to release more insulin when blood sugar levels are high, slow down gastric emptying (which helps you feel full longer), and reduce the production of glucose by the liver. They also have an appetite-suppressing effect in the brain.
One of the most appealing aspects of GLP-1 receptor agonists for many individuals is their tendency to lead to significant weight loss, a common challenge for people with type 2 diabetes. This weight loss, combined with their impressive ability to lower A1C, makes them a powerful tool for comprehensive diabetes management. Furthermore, like SGLT2 inhibitors, many GLP-1 receptor agonists have demonstrated significant cardiovascular benefits, reducing the risk of major adverse cardiovascular events in patients with established heart disease. Common side effects can include nausea, vomiting, diarrhea, or constipation, especially when treatment is first initiated. These symptoms often subside as the body adjusts, and healthcare providers typically start with a low dose and gradually increase it to improve tolerability.
Insulin Therapy: When It Becomes Necessary
While many people with type 2 diabetes can manage their condition effectively with oral medications and lifestyle changes, insulin therapy becomes a necessary and often life-saving intervention for others. This usually occurs when the pancreas, over time, can no longer produce enough insulin on its own to control blood sugar levels, or when other medications are insufficient to achieve target glucose goals. Insulin is a powerful and essential hormone that allows glucose to enter cells for energy, and supplementing it externally directly addresses the underlying insulin deficiency.
Insulin is available in various forms, each designed to meet different needs. Long-acting (basal) insulin provides a continuous, steady release of insulin throughout the day to cover background glucose needs, much like a healthy pancreas would. Rapid-acting (bolus) insulin, on the other hand, is taken before meals to cover the carbohydrate intake and manage the post-meal rise in blood sugar. Insulin therapy requires careful monitoring of blood glucose levels multiple times a day to ensure effective management and, importantly, to prevent hypoglycemia (dangerously low blood sugar), which is a primary concern. Proper injection technique, whether using pens or syringes, is also vital to ensure the medication is delivered correctly and absorbed efficiently.
Other Important Oral Medications
Beyond the core treatments, several other classes of oral medications offer valuable options for managing type 2 diabetes, often used in combination with first-line therapies or for specific patient profiles.
* Sulfonylureas (e.g., glipizide, glyburide, glimepiride): These older but still widely used medications work by directly stimulating the beta cells in the pancreas to produce and release more insulin. They are known for their ability to quickly and effectively lower blood sugar levels and are generally cost-effective. However, their primary drawbacks include a higher risk of hypoglycemia (low blood sugar), particularly if meals are skipped or delayed, and a potential for weight gain. They may also lose their effectiveness over many years as the pancreas’s ability to produce insulin declines.
* DPP-4 Inhibitors (e.g., sitagliptin, saxagliptin, linagliptin): These medications work by enhancing the body’s natural incretin system. They prevent the breakdown of incretin hormones (like GLP-1) that are naturally released after a meal, leading to increased insulin release from the pancreas when blood glucose levels are high and decreased glucose production by the liver. DPP-4 inhibitors are generally well-tolerated, have a low risk of hypoglycemia when used alone, and are weight-neutral, making them a good option for patients who need additional blood sugar control without the risk of weight gain or severe side effects.
* Thiazolidinediones (TZDs) (e.g., pioglitazone, rosiglitazone): TZDs primarily improve insulin sensitivity in muscle, fat, and liver cells, thereby reducing insulin resistance, which is a hallmark of type 2 diabetes. They help the body utilize its own insulin more efficiently, leading to lower blood sugar levels over time. While effective, TZDs can be associated with side effects such as fluid retention, which can exacerbate heart failure in some individuals, and weight gain. They may also carry an increased risk of bone fractures and should be used cautiously, especially in patients with heart conditions.
Choosing the Right Medication: A Personalized Approach
The journey to finding the “best” medicine for type 2 diabetes is profoundly individualized, recognizing that what works wonderfully for one person might not be suitable for another. Your healthcare provider will consider a multitude of factors to craft a treatment plan specifically for you. These crucial considerations include your current A1C levels (a measure of average blood sugar over 2-3 months), the presence of existing cardiovascular disease or kidney disease (which might favor SGLT2 inhibitors or GLP-1 agonists), your body weight and weight management goals, the potential for specific side effects, the cost and insurance coverage of medications, and your personal preferences regarding administration (pills vs. injections) and lifestyle.
Often, effective type 2 diabetes management involves a combination of medications, as different drugs target various aspects of the disease’s pathophysiology. For example, metformin might be combined with an SGLT2 inhibitor to lower liver glucose production and enhance glucose excretion, or with a GLP-1 agonist for added weight loss and cardiovascular protection. This multi-pronged approach ensures comprehensive blood sugar control and addresses broader health risks. Regular, open communication with your healthcare provider is absolutely essential. Your medication regimen is not set in stone; it will likely need to be adjusted and optimized over time as your condition evolves, your health needs change, or as new and improved treatments become available.
Ultimately, managing type 2 diabetes effectively requires a collaborative, ongoing effort between you and your healthcare team, integrating the right medications with consistent lifestyle modifications like a healthy diet and regular physical activity. There is no one-size-fits-all solution, but a personalized approach utilizing the most appropriate medicines can significantly improve your quality of life, prevent long-term complications, and help you live a healthier, more vibrant life. Don’t hesitate to consult with your doctor to discuss which diabetes medications are best suited for your specific health profile, goals, and lifestyle. They are your best resource for navigating these important decisions.
Frequently Asked Questions
What are the most common first-line medications prescribed for newly diagnosed type 2 diabetes?
For most individuals newly diagnosed with type 2 diabetes, metformin is the initial and often preferred medication. It works by reducing glucose production by the liver and improving insulin sensitivity in the body’s cells, effectively lowering blood sugar levels. Alongside metformin, crucial lifestyle changes like diet and exercise are always emphasized as foundational for managing type 2 diabetes.
Which type 2 diabetes medications are known to help with weight loss or avoid weight gain?
Several newer classes of type 2 diabetes medications offer benefits beyond just blood sugar control, including potential weight loss or weight neutrality. GLP-1 receptor agonists (e.g., semaglutide, liraglutide) and SGLT2 inhibitors (e.g., empagliflozin, dapagliflozin) are notable examples. These medications not only lower A1C but can also support weight management, which is a significant advantage for many people living with type 2 diabetes.
How do doctors determine which specific medication is best for an individual with type 2 diabetes?
Doctors personalize type 2 diabetes treatment based on several factors, including the patient’s A1C level, presence of comorbidities like heart disease or kidney issues, potential side effects of medications, and patient preferences. They consider how effectively a medicine lowers blood sugar, its impact on other health conditions, cost, and administration method (pill vs. injection) to develop the most suitable and comprehensive treatment plan.
Why might someone need more than one medication to manage their type 2 diabetes effectively?
Type 2 diabetes is a progressive condition, meaning that over time, the body’s ability to produce or use insulin effectively can worsen, leading to rising blood sugar levels. When a single medication like metformin is no longer sufficient to achieve target A1C levels, doctors will often add a second or even third medication from a different class to target various pathways of glucose regulation. This combination therapy helps to gain better control over blood sugar and prevent complications.
What are some newer classes of medications for type 2 diabetes and what additional benefits do they offer?
Two prominent newer classes of medications for type 2 diabetes are GLP-1 receptor agonists and SGLT2 inhibitors. Beyond their excellent ability to lower blood sugar and A1C, these medications offer significant cardiovascular and renal protective benefits, meaning they can reduce the risk of heart attack, stroke, and kidney disease progression. These additional benefits make them preferred options for many individuals, especially those with pre-existing heart or kidney conditions.
References
- https://diabetes.org/healthy-living/medication-treatments/type-2-diabetes/medications-for-type-2-diabetes
- https://www.niddk.nih.gov/health-information/diabetes/overview/treatment-management/medications
- https://www.cdc.gov/diabetes/managing/medications.html
- https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/in-depth/diabetes-medications/art-20046907
- https://my.clevelandclinic.org/health/diseases/21493-type-2-diabetes/management-and-treatment/medication
- https://en.wikipedia.org/wiki/Type_2_diabetes_treatment