The best meal plan for diabetics is a personalized, balanced approach prioritizing whole foods, controlled carbohydrate intake, and consistent meal times to effectively manage blood sugar. This approach helps stabilize glucose levels, prevent complications, and improve overall well-being. This guide will outline the core principles to help you build your ideal diabetic meal plan.
Understanding Core Diabetic Nutrition Principles

Navigating diabetes means understanding how food impacts your body. It’s not about deprivation, but rather making informed choices that support stable blood sugar and overall health. Let’s dive into some fundamental concepts that will empower you.
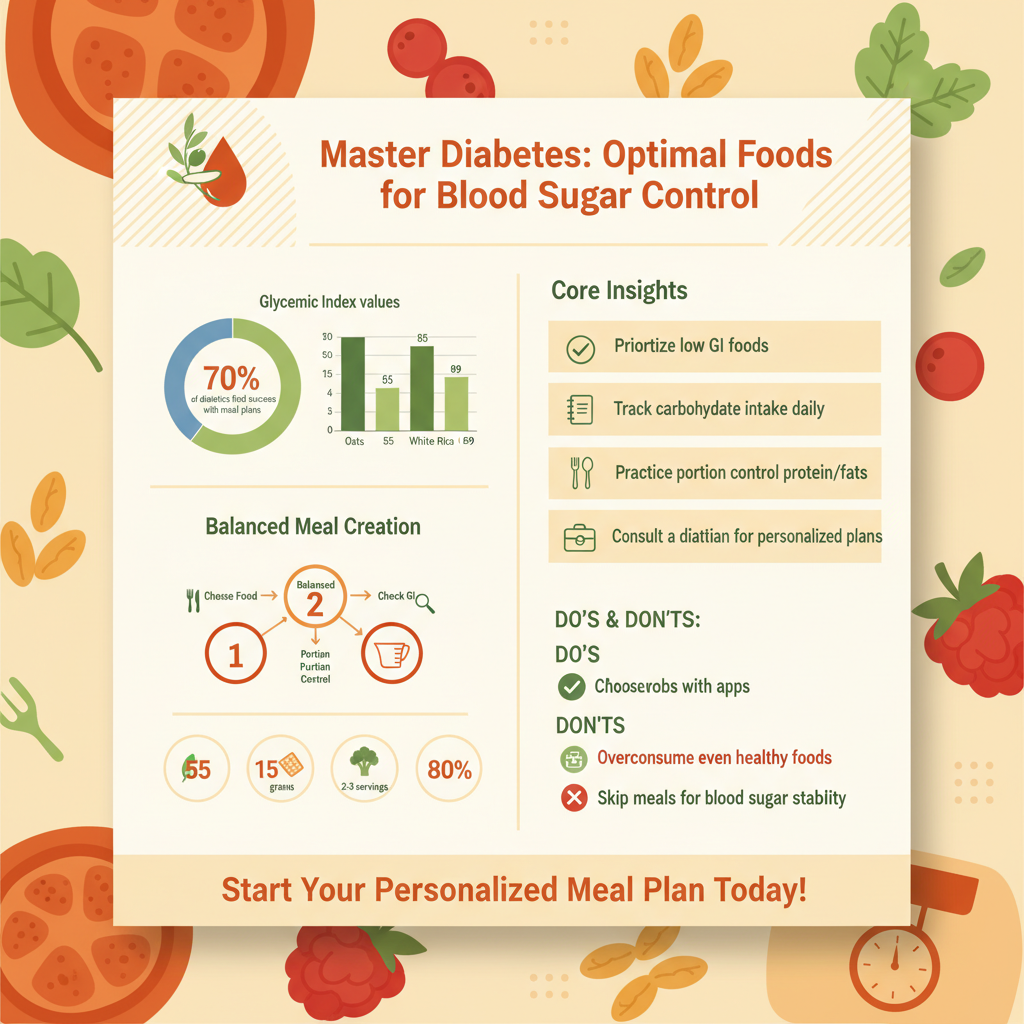
* Glycemic Index (GI) and Load (GL): The Glycemic Index (GI) is a system that ranks carbohydrate-containing foods by how much they raise blood sugar levels after eating. Foods with a high GI are quickly digested and absorbed, causing a rapid rise in blood sugar, while low GI foods are digested more slowly, leading to a gentler and more sustained rise. Glycemic Load (GL) takes this a step further by considering both the GI of a food and the amount of carbohydrates in a typical serving. Choosing lower GI foods like most non-starchy vegetables, legumes, and certain whole grains can help prevent sharp blood sugar spikes. However, it’s also important to consider the total meal composition; pairing a higher GI food with protein or healthy fats can help mitigate its impact. Understanding GI and GL helps you make smarter choices about the *type* of carbohydrates you consume.
* Carbohydrate Counting: Carbohydrate counting is a cornerstone strategy for managing blood sugar, especially for individuals using insulin. It involves tracking the amount of carbohydrates in meals and snacks to match it with insulin doses or simply to stay within a target range recommended by your healthcare team. This method provides flexibility in food choices while maintaining control. You can count carbs by reading food labels, using apps, or referring to nutrition databases. While it might seem daunting at first, with practice, it becomes an incredibly effective tool for predicting and managing blood sugar responses, helping you achieve more consistent glucose levels and improving your overall diabetes control. A Registered Dietitian can help you determine your individual carbohydrate targets.
* Portion Control: Even healthy foods can impact blood sugar and weight if consumed in excess. Portion control is about understanding appropriate serving sizes to manage your total calorie and carbohydrate intake effectively. It’s a crucial strategy not just for blood sugar management, but also for maintaining a healthy weight, which is vital for preventing and managing diabetes complications. Learning to eye-ball appropriate portions or using measuring cups and scales initially can be incredibly helpful. Paying attention to serving sizes listed on food labels is also key. Over time, you’ll develop a better sense of what a healthy portion looks like for different food groups, empowering you to enjoy a wider variety of foods responsibly.
Foods to Prioritize for Blood Sugar Stability

Filling your plate with nutrient-dense foods is key to managing blood sugar and feeling great. These food groups are your allies in creating a balanced and satisfying meal plan.
* Non-Starchy Vegetables: These are your best friends in a diabetic meal plan! Non-starchy vegetables are packed with vitamins, minerals, and fiber, yet they’re very low in carbohydrates and calories, meaning they have minimal impact on blood sugar. Think vibrant leafy greens like spinach, kale, and collards; cruciferous veggies like broccoli, cauliflower, and Brussels sprouts; and colorful options such as bell peppers, asparagus, green beans, mushrooms, and zucchini. Aim to fill at least half of your plate with these powerhouses at every meal. They add volume and nutrients without contributing to blood sugar spikes, helping you feel full and satisfied. Enjoy them steamed, roasted, grilled, or raw in salads.
* Lean Proteins: Protein is essential for building and repairing tissues, supporting muscle health, and promoting satiety, which means you feel fuller for longer. Critically for diabetics, protein has very little direct impact on blood sugar levels. Incorporating lean protein sources into every meal helps slow down the absorption of carbohydrates, further contributing to stable blood sugar. Excellent choices include skinless chicken and turkey, various types of fish (like salmon, cod, tuna, and tilapia), eggs, tofu, tempeh, beans, lentils, and Greek yogurt. Prioritizing lean options helps you get the protein you need without excessive saturated fat.
* Healthy Fats: While calorie-dense, healthy fats are crucial for heart health, satiety, and the absorption of fat-soluble vitamins. They also play a role in slowing down digestion, which can help keep blood sugar levels steady after a meal. Focus on unsaturated fats found in sources like avocados, nuts (almonds, walnuts, pecans), seeds (chia, flax, pumpkin), and olive oil. Fatty fish like salmon and mackerel are also excellent sources of omega-3 fatty acids, which are beneficial for heart health. Remember to consume healthy fats in moderation, as they are high in calories, but don’t shy away from including them in your diet for their significant benefits.
* Whole Grains: Unlike refined grains, whole grains contain all parts of the grain kernel – the bran, germ, and endosperm – providing valuable fiber, vitamins, and minerals. This fiber helps slow down the absorption of glucose into the bloodstream, leading to a more gradual rise in blood sugar compared to refined grains. While still carbohydrate-containing and needing moderation, whole grains are a much healthier choice. Opt for options like oats (steel-cut or rolled), quinoa, brown rice, whole-wheat bread and pasta, barley, and farro. Pay attention to portion sizes and consider them as your “complex carbohydrate” portion of a balanced meal, typically occupying about a quarter of your plate.
Foods to Limit or Avoid for Optimal Health

To maintain stable blood sugar and promote long-term health, it’s equally important to be mindful of foods that can negatively impact your glucose levels and overall well-being.
* Added Sugars and Sweetened Beverages: This category is arguably one of the biggest culprits for blood sugar spikes and should be heavily limited or avoided. Added sugars, found in sodas, fruit juices (even 100% juice can be problematic due to concentrated sugar without fiber), sweet tea, energy drinks, candies, pastries, cookies, and many processed desserts, directly and rapidly elevate blood sugar levels. They offer little to no nutritional value, contributing “empty calories” that can lead to weight gain and make diabetes management extremely challenging. Opt for water, unsweetened tea, or naturally flavored water with lemon or cucumber instead. When craving something sweet, choose whole fruit in moderation.
* Refined Carbohydrates: Refined carbohydrates have been stripped of their fiber, vitamins, and minerals during processing. This means they are quickly broken down into glucose in your body, causing rapid and often significant blood sugar spikes, similar to added sugars. Common examples include white bread, white rice, white pasta, sugary breakfast cereals, crackers, and many processed snack foods. These foods offer minimal nutritional benefit and can make blood sugar control a constant battle. Swapping them for their whole-grain counterparts, even in moderation, is a much healthier strategy for sustained energy and better glucose management.
* Unhealthy Fats: While healthy fats are beneficial, certain fats can negatively impact your heart health, which is a significant concern for people with diabetes who already face an increased risk of cardiovascular disease. Saturated fats, found in high amounts in fatty cuts of red meat, full-fat dairy products, butter, and some processed snacks, can raise LDL (“bad”) cholesterol. Trans fats, often found in fried foods, fast food, margarines, and many commercially baked goods and processed snacks, are even worse, raising LDL cholesterol while lowering HDL (“good”) cholesterol. Always check food labels for “partially hydrogenated oil” – a clear sign of trans fats. Limiting these unhealthy fats protects your heart and supports overall metabolic health.
Building Your Plate: Practical Meal Strategies
Once you know which foods to prioritize and which to limit, the next step is to put it all together into practical, balanced meals. These strategies make meal planning easy and effective.
* The Plate Method: This is a super simple yet incredibly effective visual tool for building balanced meals without complex calculations. Imagine your plate divided into three sections:
* Half of your plate: Fill this with non-starchy vegetables (e.g., a large salad, steamed broccoli, roasted bell peppers). This ensures a good fiber intake and minimal carbohydrate impact.
* One-quarter of your plate: Dedicate this section to lean protein (e.g., grilled chicken breast, baked fish, a serving of lentils). This provides satiety and helps stabilize blood sugar.
* One-quarter of your plate: This is for your complex carbohydrates (e.g., a small serving of brown rice, quinoa, whole-wheat pasta, or a sweet potato). This portion ensures you get necessary energy while managing carb intake.
This method takes the guesswork out of portioning and helps create satisfying, blood-sugar-friendly meals every time.
* Consistent Meal Timing: Eating meals and snacks at regular intervals throughout the day is crucial for maintaining stable blood sugar levels. Skipping meals or eating at erratic times can lead to significant fluctuations – either dangerous drops (hypoglycemia) or sharp spikes (hyperglycemia) as your body tries to compensate. Consistency helps your body process food and utilize insulin more efficiently, making it easier to manage your glucose. Aim for meals roughly every 4-5 hours, with healthy snacks in between if needed, especially if you’re on certain medications. Establishing a routine helps your body anticipate food intake and regulate blood sugar more smoothly.
* Mindful Eating: Beyond what you eat, *how* you eat plays a significant role in blood sugar management and overall well-being. Mindful eating involves paying full attention to your food, recognizing hunger and fullness cues, and savoring the experience. This means eating slowly, chewing thoroughly, putting down your fork between bites, and minimizing distractions like screens. Practicing mindful eating can help you feel more satisfied with smaller portions, prevent overeating, and better connect with your body’s signals. It also reduces stress, which can indirectly impact blood sugar. By truly enjoying your meals, you can improve digestion, satisfaction, and your relationship with food.
Effective Meal Planning and Preparation Tips
Success with a diabetic meal plan often comes down to preparation. These tips will help you stay on track, even on busy days.
* Weekly Meal Prep: Taking some time each week to plan and prepare your meals in advance can be a game-changer for diabetes management. Batch cooking ensures you have healthy, portion-controlled options readily available, reducing the temptation for quick, unhealthy choices when hunger strikes. You can cook a large batch of lean protein (like chicken or turkey), chop vegetables for salads or stir-fries, cook a pot of quinoa or brown rice, or even assemble complete meals in containers. This strategy saves time during the busy week, reduces stress, and makes sticking to your meal plan much easier and more consistent.
* Reading Food Labels: Becoming a savvy label reader is an empowering skill for anyone managing diabetes. Food labels provide vital nutritional information that helps you make informed choices. Pay close attention to:
* Serving Size: All other information is based on this; make sure to adjust if you eat more or less.
* Total Carbohydrates: This is key for carb counting.
* Fiber: Higher fiber content is generally better, as it slows sugar absorption.
* Added Sugars: Aim for as little as possible.
* Saturated and Trans Fats: Limit these for heart health.
Understanding these numbers allows you to choose products that align with your dietary goals and avoid hidden sugars or unhealthy ingredients.
* Smart Snacking: Snacks can be a valuable tool in a diabetic meal plan, helping to prevent extreme hunger between meals and stabilize blood sugar. However, choosing the *right* snacks is crucial. Opt for healthy, portion-controlled options that combine protein, fiber, or healthy fats to promote satiety and provide a sustained release of energy. Great ideas include a handful of unsalted nuts, a piece of fruit with a small spoonful of peanut butter, Greek yogurt with a few berries, vegetable sticks with hummus, or a hard-boiled egg. Avoid processed snacks high in sugar, unhealthy fats, and refined carbs, as they will quickly spike your blood sugar and leave you feeling hungry again soon after.
The Role of Professional Guidance and Support
While these principles provide an excellent foundation, individual needs vary greatly. Professional guidance is invaluable for tailoring a plan that truly works for you.
* Consult a Registered Dietitian (RD/RDN): This is perhaps the most critical step you can take. A Registered Dietitian (RD or RDN) specializes in medical nutrition therapy and can create a personalized meal plan tailored precisely to your specific needs, preferences, lifestyle, and medical conditions. They can help you set realistic carbohydrate targets, teach you advanced carb counting techniques, navigate food labels, address any food allergies or intolerances, and provide ongoing support and adjustments. Their expertise is invaluable in developing a sustainable and effective eating strategy that goes beyond general recommendations and focuses on *your* unique path to better health.
* Regular Doctor Check-ups: Your doctor is a central figure in your diabetes management team. Regular check-ups are essential for monitoring your blood sugar levels (including A1C), blood pressure, cholesterol, and kidney function. Your doctor can adjust your medications as needed, discuss any symptoms or concerns you have, and help you understand the broader implications of your diet on your overall health. Maintaining open communication with your healthcare provider ensures that your meal plan and lifestyle choices are always in sync with your medical treatment, working together to prevent complications and improve your long-term health outcomes.
* Diabetes Education Programs: Many hospitals, community centers, and online platforms offer comprehensive diabetes education programs. These programs are designed to provide in-depth knowledge and practical skills for managing diabetes effectively. You can learn about meal planning, blood sugar monitoring, medication management, physical activity, and coping strategies. Participating in such programs can empower you with a deeper understanding of your condition, help you connect with others facing similar challenges, and provide the confidence to make informed decisions about your health. Education is a powerful tool in taking control of your diabetes.
Crafting the best meal plan for diabetics involves a commitment to understanding nutrition, making informed food choices, and consistently applying these principles. By focusing on whole foods, managing carbohydrates, controlling portions, and seeking professional guidance, you can develop an eating strategy that supports stable blood sugar, enhances your health, and improves your quality of life. Start by incorporating these key principles into your daily routine and consult with a dietitian to tailor a plan perfect for you.
Frequently Asked Questions
What are the core principles of an effective meal plan for diabetics?
An effective meal plan for diabetics focuses on consistent carbohydrate intake, portion control, and a balanced distribution of macronutrients to help manage blood sugar levels. Prioritizing whole, unprocessed foods like vegetables, lean proteins, and healthy fats, while limiting added sugars and refined grains, is fundamental for **diabetes management**. The goal is to create sustainable eating habits that support stable glucose and overall well-being.
How can I effectively manage my carbohydrate intake when planning meals?
Effective carbohydrate management involves understanding which foods contain carbs and practicing portion control through methods like carb counting or using the plate method. Focus on complex carbohydrates from whole grains, legumes, and non-starchy vegetables, which have a lower glycemic index and release glucose more slowly. Consulting a registered dietitian can provide personalized guidance on setting appropriate carbohydrate targets for your **diabetic meal plan**.
Which foods should be prioritized, and which should be limited, in a diabetic meal plan?
Prioritize non-starchy vegetables (like leafy greens, broccoli, peppers), lean proteins (chicken, fish, tofu), healthy fats (avocado, nuts, olive oil), and whole grains in your **diabetic meal plan** for optimal nutrition and blood sugar control. Foods to limit include sugary beverages, processed snacks, refined grains (white bread, pasta), and foods high in saturated and trans fats. This focus helps maintain stable glucose and improve heart health.
Why is personalized dietary advice crucial for creating the best diabetic meal plan?
Personalized dietary advice is crucial because each individual’s diabetes is unique, influenced by factors like medication, activity level, other health conditions, and personal preferences. A generic **meal plan for diabetics** may not adequately address specific nutritional needs or cultural eating habits, potentially leading to suboptimal blood sugar control. Working with a doctor or registered dietitian ensures your plan is tailored for maximum effectiveness and sustainability.
What does a balanced plate look like for someone managing diabetes?
A balanced plate for **diabetes management** typically follows the “plate method”: half of your plate should be filled with non-starchy vegetables (e.g., spinach, carrots, bell peppers). One-quarter of the plate should contain lean protein (e.g., grilled chicken, fish, beans), and the remaining quarter should consist of a complex carbohydrate source (e.g., quinoa, brown rice, a small sweet potato). Adding a small serving of healthy fats and a piece of fruit can complete this well-rounded **diabetic meal plan**.
References
- Simple Diabetes Meal Plan: Manage Blood Glucose with the Diabetes Plate
- Healthy Living with Diabetes – NIDDK
- https://www.cdc.gov/diabetes/managing/eat-well.html
- Diabetes diet: Create your healthy-eating plan – Mayo Clinic
- https://www.health.harvard.edu/staying-healthy/the-best-diet-for-type-2-diabetes
- Diabetic Diet | MedlinePlus
- https://www.ucsfhealth.org/education/nutrition-tips-for-diabetes