Choosing the best lotion for diabetics’ feet is crucial for preventing complications, and the ideal products prioritize intense hydration, gentle formulations, and ingredients that support the skin’s natural barrier. Look for lotions specifically designed for diabetic foot care, often containing humectants like urea or hyaluronic acid, and emollients such as ceramides, while avoiding fragrances, dyes, and harsh chemicals. This guide will help you understand what makes a lotion effective and how to incorporate it into your daily routine.
Why Specialized Foot Care is Essential for Diabetics

Taking proactive care of your feet is incredibly important when you have diabetes, and it goes far beyond just comfort. Your feet are particularly vulnerable to a range of complications that can arise from the condition, making daily, specialized attention absolutely non-negotiable for long-term health and well-being.
* Preventing Complications: Diabetes, especially if blood sugar levels are not consistently well-managed, can lead to two primary issues that significantly impact foot health: neuropathy and poor circulation. Diabetic neuropathy, or nerve damage, can cause a loss of sensation in your feet, meaning you might not feel cuts, blisters, burns, or even pressure from ill-fitting shoes. A minor injury can easily go unnoticed and worsen without you realizing it. Simultaneously, poor circulation means that blood flow to your feet is reduced, hindering the body’s ability to heal wounds and fight off infections. This dangerous combination makes feet highly susceptible to dryness, cracks, and slow-healing wounds. What might be a minor scrape for someone without diabetes could quickly escalate into a severe infection or ulcer for a diabetic individual, potentially leading to more serious interventions like amputation if not promptly addressed. Regular moisturizing helps create a resilient skin barrier, acting as a vital defense against these potential complications.
* Maintaining Skin Integrity: Your skin acts as your body’s primary protective barrier against the outside world. For people with diabetes, this barrier can become compromised. High blood sugar levels can reduce the skin’s natural moisture, leading to persistent dryness, flakiness, and a loss of elasticity. This dry skin is more prone to cracking and fissures, especially in areas of high pressure like the heels and balls of the feet. These cracks are not just uncomfortable; they create tiny entry points for bacteria, significantly increasing the risk of infection. Regular application of a specialized diabetic lotion helps to restore and maintain the skin’s natural moisture balance and strengthen its protective barrier. By keeping the skin supple and intact, you drastically reduce the likelihood of cracks forming and provide a robust shield against harmful pathogens.
* Early Detection: The simple, consistent act of applying lotion to your feet every day encourages a crucial routine: daily foot inspection. Because neuropathy can mask pain and discomfort, it’s vital to visually and physically check your feet for any changes. While applying lotion, you’re more likely to notice subtle signs that might otherwise go unnoticed. This includes checking for new cuts, scrapes, blisters, redness, swelling, unusual warmth, ingrown toenails, changes in skin color, or any unusual growths. Spotting these minor issues early, before they have a chance to develop into serious problems, is incredibly powerful. Early detection means you can address concerns promptly, whether it’s a simple bandage, a change in footwear, or a visit to your doctor or podiatrist, thereby preventing minor irritations from escalating into major health crises.
Key Ingredients to Look For in Diabetic Lotions
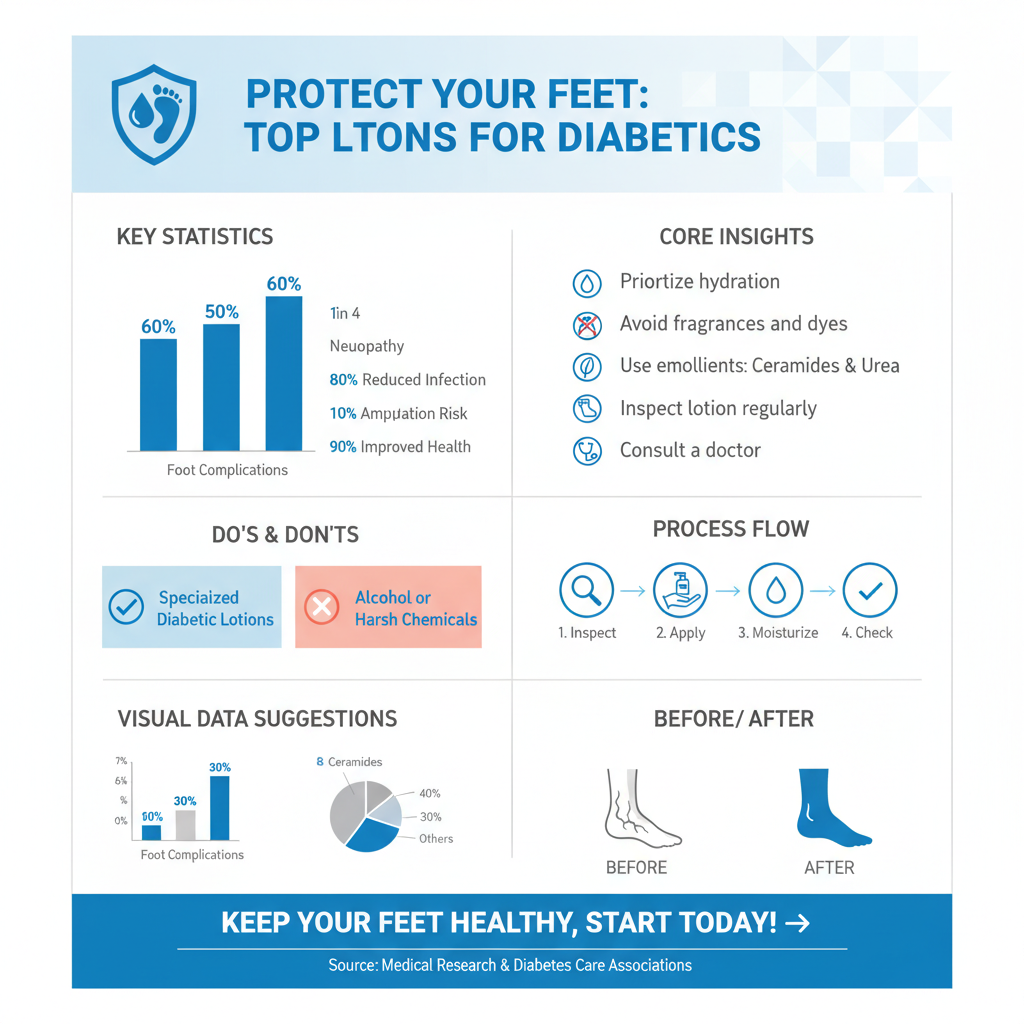

When selecting a lotion for diabetic foot care, the ingredient list is your best friend. Look for formulations packed with components specifically chosen for their hydrating, barrier-supporting, and gentle properties. These ingredients work synergistically to provide the specialized care your feet need.
* Hydrating Humectants: These powerhouse ingredients are essential because they attract and bind water to the outermost layer of your skin, providing deep and lasting hydration.
* Urea: Often considered a gold standard in diabetic foot care, urea is a naturally occurring compound in healthy skin that is both a powerful humectant and a mild keratolytic. This means it not only draws moisture into the skin but also gently breaks down and softens thick, rough, or callused skin. Look for concentrations typically between 5-10% for daily moisturizing, as higher concentrations (15-40%) are usually reserved for more targeted exfoliation under a doctor’s guidance.
* Hyaluronic Acid: Known for its incredible ability to hold up to 1,000 times its weight in water, hyaluronic acid is a super hydrator. It helps to plump the skin, improve elasticity, and reduce the appearance of dryness and fine lines, leaving feet feeling soft and smooth.
* Lactic Acid: Another alpha-hydroxy acid (AHA) that acts as both a humectant and a gentle exfoliant. In lower concentrations, lactic acid helps hydrate dry skin and improve its texture, making it softer and more pliable without being overly harsh.
Other beneficial humectants include glycerin and sodium PCA, which also help draw moisture into the skin.
* Skin Barrier Support: A healthy skin barrier is crucial for locking in moisture and protecting against external irritants and bacteria. These ingredients help repair and strengthen that barrier.
* Ceramides: These are natural lipids (fats) that are a fundamental component of the skin barrier. Think of your skin cells as bricks and ceramides as the mortar that holds them together. Replenishing ceramides helps to repair a compromised barrier, reducing transepidermal water loss (TEWL) and making the skin more resilient against dryness and environmental stressors.
* Petrolatum (Petroleum Jelly): A highly effective occlusive agent, petrolatum forms a protective, non-breathable layer on the skin’s surface. This barrier physically prevents moisture from evaporating, sealing in hydration and protecting the skin from external irritants.
* Dimethicone: A silicone-based polymer, dimethicone also acts as an occlusive, but it’s often preferred for its lighter, non-greasy feel. It forms a breathable protective barrier that helps to smooth the skin’s surface and prevent moisture loss, without feeling heavy or sticky.
These emollients work to “fill in the gaps” in a dry, damaged skin barrier, making it stronger and more effective at retaining moisture.
* Gentle and Non-Irritating: Given the sensitive and often compromised nature of diabetic skin, minimizing potential irritants is paramount.
* Always opt for formulas that are fragrance-free and dye-free. Fragrances, even “natural” ones, are common culprits for skin irritation and allergic reactions, which can be particularly problematic for fragile diabetic skin. Dyes serve no therapeutic purpose and can also cause sensitivities.
* Look for products labeled as hypoallergenic, which indicates they are formulated to minimize the risk of allergic reactions.
* Many reputable brands will also clearly state that their products are dermatologist-tested or podiatrist-recommended, offering an extra layer of assurance regarding their safety and efficacy for sensitive skin.
Ingredients to Avoid for Diabetic Foot Health

Just as important as knowing what to look for, is knowing what to steer clear of. Certain ingredients can irritate, dry out, or even damage the already vulnerable skin of diabetic feet, counteracting your best efforts at proper care.
* Harsh Fragrances and Dyes: These are top offenders when it comes to skin irritation and allergic reactions, especially for sensitive or compromised skin. Fragrances, whether natural or synthetic, can trigger contact dermatitis, leading to redness, itching, burning, and even rashes. For diabetic skin, which is already prone to dryness and slow healing, any form of irritation can compromise the skin barrier further, creating opportunities for infection or making existing issues worse. Dyes, added purely for aesthetic appeal, offer no benefit and can also be common allergens. It’s always best to choose lotions explicitly labeled “fragrance-free” and “dye-free” to minimize these risks.
* Alcohol-Based Products: When we talk about alcohol to avoid in lotions, we’re primarily referring to simple, drying alcohols like ethanol, isopropyl alcohol (rubbing alcohol), alcohol denat., or SD alcohol. These types of alcohol act as solvents and can strip the skin of its natural oils and protective lipids, leading to excessive dryness, irritation, and disruption of the skin’s vital barrier function. While they might feel like they’re drying quickly, they actually dehydrate the skin, which is the opposite of what diabetic feet need. This can exacerbate existing dryness and make the skin more prone to cracking and vulnerability. Note that “fatty alcohols” like cetyl alcohol or stearyl alcohol are different; these are emollients that actually help moisturize and condition the skin. Always check the ingredient list carefully for the drying forms of alcohol.
* Intense Exfoliants (without doctor’s advice): While gentle exfoliants like low concentrations of urea or lactic acid can be beneficial for softening rough skin, strong, aggressive exfoliants should be avoided unless specifically recommended and supervised by a podiatrist or doctor. This includes harsh physical scrubs with abrasive particles, or chemical exfoliants with high concentrations of alpha-hydroxy acids (AHAs), beta-hydroxy acids (BHAs), or retinoids. Fragile diabetic skin can be easily damaged by intense exfoliation, leading to micro-tears, raw spots, or even open wounds. Given the impaired healing capacity and increased infection risk associated with diabetes, any break in the skin barrier is a serious concern. If you have significant calluses or very thick skin, consult your healthcare provider for safe and appropriate removal methods, which may include professional debridement or specific topical treatments.
Top Characteristics of Effective Diabetic Foot Lotions
Beyond the ingredient list, the overall formulation and characteristics of a lotion play a significant role in its effectiveness and, perhaps more importantly, its consistent use. The best lotions for diabetic feet are designed with both efficacy and user experience in mind.
* Fast-Absorbing and Non-Greasy: This characteristic might seem like a matter of preference, but for daily diabetic foot care, it’s incredibly practical and safety-oriented. A fast-absorbing, non-greasy formula ensures that the lotion penetrates the skin quickly without leaving a heavy, sticky, or slippery residue. This encourages consistent daily application because it’s convenient and comfortable – you don’t have to wait a long time before putting on socks or shoes. More importantly, a greasy residue on the soles of your feet can be a significant safety hazard, increasing the risk of slips and falls, which can lead to injuries that are particularly problematic for individuals with diabetes. A lotion that feels light and clean on the skin makes the daily moisturizing routine much more pleasant and sustainable.
* Long-Lasting Hydration: Diabetic feet often suffer from chronic dryness, meaning that a quick burst of moisture isn’t enough. An effective lotion must provide sustained hydration throughout the day to truly prevent the skin from drying out, cracking, and becoming vulnerable. Look for products that boast “24-hour hydration” or “long-lasting moisture.” These formulations typically combine humectants (to draw in moisture) with emollients and occlusives (to seal it in and prevent evaporation), creating a protective barrier that continues to work for many hours. Consistent, long-lasting moisture keeps the skin pliable, healthy, and resilient, reducing the need for multiple applications throughout the day and ensuring continuous protection against dryness.
* Dermatologist Recommended: When a lotion is recommended or endorsed by dermatologists or podiatrists, it offers an extra layer of assurance regarding its safety and effectiveness. These professionals are experts in skin health and foot care, respectively, and their recommendations are typically based on rigorous testing, clinical studies, and a deep understanding of what works best for sensitive and compromised skin. Products bearing such endorsements are usually formulated with high standards, free from common irritants, and designed to address specific skin concerns effectively. Seeing this recommendation on a product label indicates that the lotion has been vetted by medical professionals who understand the unique needs of diabetic foot health, making it a reliable choice for your daily routine.
Proper Application Techniques for Maximum Benefit
Applying lotion might seem straightforward, but for diabetic feet, following specific techniques can significantly enhance the product’s effectiveness and help prevent potential problems. It’s not just about what you use, but how you use it!
* Clean and Dry Feet: This is perhaps the most crucial step before applying any foot lotion. Always start with feet that are thoroughly clean and completely dry. Washing your feet daily (using lukewarm water and a mild soap) removes dirt, sweat, and bacteria, allowing the lotion to absorb more effectively and without trapping impurities. Drying your feet completely, however, is even more critical, especially between the toes. Gently pat your feet dry with a soft towel, rather than rubbing vigorously, which can irritate sensitive skin. Any residual moisture, particularly in the warm, dark environment between your toes, can create an ideal breeding ground for fungal infections like athlete’s foot. Ensure every crevice is dry before moving on to the next step. Applying lotion immediately after a bath or shower, once your feet are dry, is often ideal because your skin is slightly softened and more receptive to moisture.
* Focus on Dry Areas: Once your feet are clean and dry, concentrate the lotion application on the areas most prone to dryness and pressure. These typically include the heels, soles, and the tops of your feet. These regions bear the brunt of daily activity and are often thicker and drier than other skin areas. Use a generous amount of lotion and gently massage it into the skin until it’s absorbed. Massaging not only helps the product penetrate but also can stimulate blood circulation, which is beneficial for diabetic foot health. Pay extra attention to rough patches and calluses (but remember, heavy calluses should be managed by a podiatrist, not just lotion). Ensure full coverage of these vulnerable areas to provide maximum hydration and protection.
* Avoid Between Toes: This instruction is so important it deserves its own specific mention. While you want to hydrate the rest of your foot, *never* apply lotion between your toes. As mentioned earlier, the spaces between your toes are naturally warm and prone to retaining moisture. Introducing lotion here further increases the humidity, creating a perfect, dark, and damp environment for fungal infections to thrive. Fungal infections can lead to itching, redness, cracking, and peeling, which, for a diabetic individual, can easily become entry points for bacterial infections and lead to more serious complications. Always ensure this area remains dry and free of lotion to protect against fungal growth and maintain optimal foot health.
When to Seek Professional Medical Advice
While a good daily foot care routine with the right lotion is fundamental for managing diabetic foot health, there are critical times when you must elevate your concerns to a healthcare professional. Ignoring these signs can have severe consequences for individuals with diabetes.
* Persistent Dryness or Cracking: If, despite consistent daily use of a specialized diabetic lotion and following proper application techniques, you find that your feet remain persistently dry, flaky, or continue to develop cracks, it’s time to consult your doctor or podiatrist. This could indicate that the lotion you’re using isn’t strong enough, or more importantly, it could be a sign of an underlying issue that needs medical attention. Sometimes, what looks like persistent dryness might actually be a subtle fungal infection or another dermatological condition requiring prescription-strength treatment. A professional can assess the situation, recommend a more potent treatment, or investigate any deeper causes contributing to your skin’s condition, ensuring you get the right care.
* Signs of Infection: Any indication of an infection on your feet requires immediate medical attention. Do not wait to see if it improves on its own. For individuals with diabetes, infections can escalate rapidly and lead to very serious complications due to impaired immune response and circulation.
* Redness or Swelling: If an area of your foot becomes unusually red, inflamed, or swollen, especially if it’s new or worsening.
* Warmth: If a particular area of your foot feels noticeably warmer to the touch than the surrounding skin.
* Pain: If you experience new or increased pain, throbbing, or tenderness, particularly around a wound or blister, even if your neuropathy usually masks pain.
* Pus or Discharge: Any fluid, pus, or foul odor emanating from a cut, blister, or crack is a definitive sign of infection.
* Red Streaks: Red streaks spreading from a wound up your leg can indicate a spreading infection (cellulitis) and is a medical emergency.
* Fever or Chills: Systemic symptoms like fever or chills accompanying a foot issue mean the infection is affecting your whole body.
Prompt medical intervention is crucial to prevent the infection from spreading, potentially leading to ulcers, osteomyelitis (bone infection), or, in severe cases, amputation.
* New Wounds or Sores: Even seemingly minor cuts, blisters, scrapes, or sores on a diabetic foot should be evaluated by a healthcare professional promptly, even if they don’t appear to be infected. Due to neuropathy, you might not feel the severity of the injury, and what seems insignificant can quickly become a serious problem. A small blister could rupture, a minor cut could become infected, or a persistent sore might indicate a developing ulcer. Diabetic foot wounds often heal slowly, and the risk of infection is always high. Your doctor or podiatrist can properly clean and dress the wound, provide guidance on care, and monitor its healing to prevent complications. Early intervention with any new break in the skin is paramount to protecting your foot health.
Maintaining healthy feet is paramount when managing diabetes, and selecting the right lotion is a simple yet powerful step in your daily routine. By prioritizing products with hydrating humectants like urea and hyaluronic acid, barrier-supporting emollients such as ceramides and dimethicone, and always opting for fragrance-free, dye-free formulas, you can significantly reduce the risk of common foot complications like dryness, cracking, and infection. Make daily foot moisturizing a consistent habit, always remembering to apply it to clean, thoroughly dried feet (avoiding between the toes), and incorporating a quick visual inspection. Most importantly, stay vigilant and proactive; if you notice any persistent dryness, new wounds, or signs of infection, do not hesitate to consult your healthcare provider promptly. Your feet carry you through life, so give them the specialized care they deserve!
Frequently Asked Questions
Why is special lotion important for diabetic feet, and how does it differ from regular moisturizers?
Diabetics often experience neuropathy and reduced blood flow, leading to excessively dry, cracked skin on their feet, which significantly increases the risk of infection and complications. Specialized diabetic foot lotions are formulated to provide intensive hydration without irritation, using gentle ingredients that support the skin’s barrier function. Unlike many regular lotions, they typically avoid harsh fragrances, dyes, and alcohols that can further dry or irritate sensitive diabetic skin, making them crucial for maintaining skin integrity and preventing issues.
What key ingredients should I look for in the best lotion for diabetics’ feet?
When choosing a lotion for diabetic feet, prioritize ingredients known for deep hydration and skin barrier support. Look for humectants like urea, lactic acid, or hyaluronic acid, which effectively draw moisture into the skin, and emollients such as ceramides, shea butter, or dimethicone to seal that moisture in. These components are vital for softening dry, cracked skin and preventing further damage, making them essential in an effective diabetic foot lotion. Ensure the product is also fragrance-free and hypoallergenic to minimize irritation.
What ingredients should diabetics *avoid* when selecting a foot lotion or cream?
Diabetics should generally avoid lotions containing harsh ingredients that can irritate or further dry sensitive skin, potentially exacerbating existing conditions. Steer clear of products with strong fragrances, dyes, and high concentrations of alcohol, which can be drying and cause allergic reactions. Additionally, avoid salicylic acid or other strong chemical exfoliants unless specifically recommended by a podiatrist, as these can be too harsh for fragile diabetic skin and potentially lead to open wounds or irritation.
How often should diabetics apply lotion to their feet for optimal care, and what’s the best technique?
For optimal diabetic foot care, lotion should be applied daily, preferably after bathing when the skin is clean and slightly damp, to effectively lock in moisture. Gently massage a generous amount of the best lotion for diabetics feet onto the tops and bottoms of your feet, paying close attention to heels and calloused areas. Crucially, avoid applying lotion *between* your toes, as this can trap moisture and create a warm, moist environment conducive to fungal infections.
Beyond lotion, what are other essential daily practices for comprehensive diabetic foot care?
While using the right lotion is vital, comprehensive diabetic foot care involves several other essential daily practices to maintain foot health and prevent complications. Always inspect your feet daily for cuts, blisters, redness, swelling, or any unusual changes, using a mirror if necessary to check the soles. Wear properly fitting shoes and clean, seamless socks to prevent friction and pressure points, and never walk barefoot, even indoors. Regular check-ups with a podiatrist are also crucial for professional assessment and early detection of potential issues.
References
- https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetic-foot/art-20046161
- https://my.clevelandclinic.org/health/diseases/17691-diabetes-foot-care
- https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/diabetic-foot-care
- https://healthcare.utah.edu/healthfeed/2023/11/diabetic-foot-care-how-to
- https://www.apma.org/patients/foot-health-facts/diabetes/
- Low blood sugar – self-care: MedlinePlus Medical Encyclopedia
- Dermatologist-recommended skin care for people with diabetes
- Diabetes and feet | Foot problems | Diabetes UK