Determining the single best diabetic medication depends entirely on your specific diagnosis, though Metformin is widely considered the first-line standard for Type 2 diabetes due to its effectiveness and safety profile. For Type 1 diabetes, insulin is the essential, life-saving medication required for survival. Recently, newer drug classes like GLP-1 agonists (such as Ozempic) and SGLT2 inhibitors have gained popularity for their dual benefits of blood sugar control and cardiovascular protection. Navigating a diagnosis of diabetes can feel overwhelming, but understanding your pharmaceutical toolkit is the first step toward feeling empowered and in control of your health. Let’s explore the options available today so you can have a more informed conversation with your doctor.
Metformin: The First-Line Defense

For the vast majority of people diagnosed with Type 2 diabetes, the journey begins with Metformin. You can think of this medication as the reliable foundation of diabetes management. It has been around for decades, and for good reason: it works well, and it is incredibly safe for most people.
Metformin works primarily by targeting the liver. In a healthy body, the liver releases stored glucose when you haven’t eaten for a while to keep your energy levels stable. However, in Type 2 diabetes, the liver often gets confused and dumps too much sugar into the bloodstream, even when you don’t need it. Metformin gently puts the brakes on this process, lowering the amount of glucose your liver produces. Additionally, it helps your muscle cells become more sensitive to insulin, meaning they can absorb sugar from your blood more effectively.
There are two major reasons why Metformin remains the champion of first-line defense. First is the low risk of hypoglycemia (dangerously low blood sugar). Unlike some older medications that squeeze the pancreas to pump out insulin regardless of your sugar levels, Metformin doesn’t stimulate insulin production directly. This means you aren’t likely to crash or feel shaky and weak from taking it.
The second factor is cost-effectiveness. In a world where medical costs are soaring, Metformin is widely available as a generic drug, often costing just pennies a day. While it is famous for causing some stomach upset when you first start taking it, these side effects usually subside with time or by switching to the extended-release version. For its blend of safety, efficacy, and affordability, it remains the gold standard.
GLP-1 Receptor Agonists
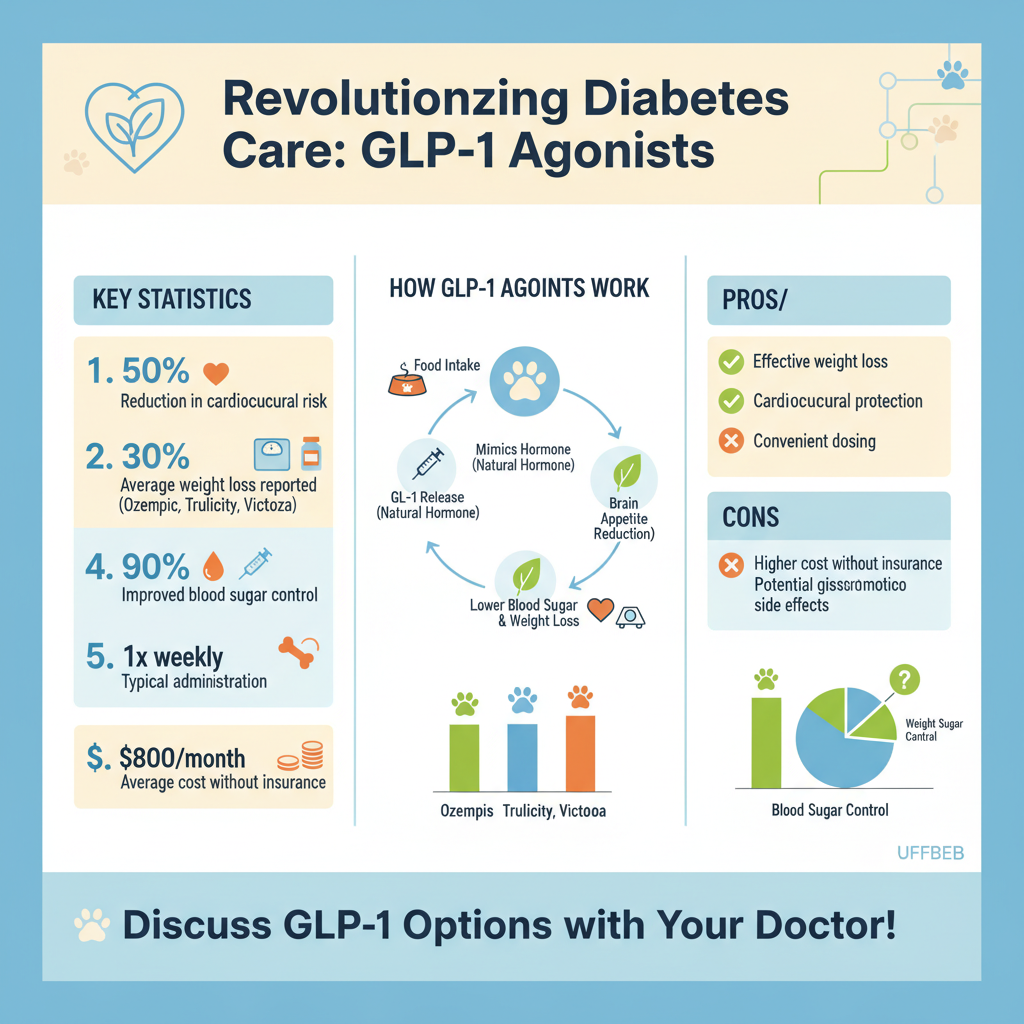

If you have been following health news lately, you have almost certainly heard of GLP-1 receptor agonists. This class of drugs, which includes brand names like Ozempic (semaglutide), Trulicity (dulaglutide), and Victoza (liraglutide), has revolutionized diabetes care. These are typically injectable medications—though oral versions like Rybelsus now exist—that mimic a natural hormone called glucagon-like peptide-1.
When you eat, your body releases GLP-1 to tell your pancreas to release the right amount of insulin. These medications amplify that signal. However, they do more than just manage insulin. They also slow down gastric emptying, which means food stays in your stomach longer. This prevents sharp spikes in blood sugar after meals and sends a strong signal to your brain that you are full.
This mechanism leads to the “game-changing” aspect of GLP-1 agonists: significant weight loss. For many patients with Type 2 diabetes, carrying excess weight is a contributing factor to insulin resistance. By helping patients lose weight, these drugs tackle the root cause of the metabolic issue, not just the symptoms.
Furthermore, leading options in this class have been proven to offer robust heart health protection. Clinical trials have shown that for diabetics with established cardiovascular disease, taking a GLP-1 agonist can significantly reduce the risk of heart attack, stroke, and cardiovascular death. While they are more expensive and can cause nausea initially, the dual benefits of potent blood sugar control and cardiovascular defense make them a top contender for the “best” medication for many patients.
SGLT2 Inhibitors

Another exciting advancement in modern diabetes care is the class of drugs known as SGLT2 inhibitors. These include medications like Jardiance (empagliflozin), Farxiga (dapagliflozin), and Invokana (canagliflozin). Unlike most diabetes drugs that focus on insulin or the liver, SGLT2 inhibitors take a completely different approach: they put the kidneys to work.
Normally, your kidneys act as a filter that reabsorbs glucose back into the bloodstream so you don’t lose energy. SGLT2 inhibitors block this reabsorption process. Essentially, they open an “exit door” for excess sugar, allowing your body to flush it out through your urine. This mechanism lowers blood sugar without relying on insulin, which also minimizes the risk of low blood sugar events.
Beyond glucose control, these medications have emerged as superstars for organ protection. They are incredibly beneficial for patients with heart failure. By acting as a mild diuretic (water pill), they reduce the volume of fluid the heart has to pump, easing the strain on the cardiovascular system.
Additionally, they are highly protective of the kidneys themselves. Diabetic kidney disease is a common and serious complication, but SGLT2 inhibitors have been shown to slow the progression of kidney damage significantly. If you have Type 2 diabetes and are at risk for heart failure or kidney disease, your doctor might suggest this class of medication not just for your sugar levels, but to protect your vital organs for the long haul.
Insulin Therapy
Despite the advancements in oral and non-insulin injectable drugs, insulin remains a cornerstone of diabetes treatment. It is important to remove the stigma often associated with insulin; needing it does not mean you have “failed” at managing your diabetes. It simply means your body needs a tool that other medications cannot provide.
For people with Type 1 diabetes, insulin is non-negotiable. Their bodies have stopped producing this hormone entirely, so they must replace it via injections or a pump to survive. For those with Type 2 diabetes, insulin is often introduced as the condition progresses and the pancreas naturally produces less insulin over the years.
Insulin therapy is generally broken down into two main categories:
1. Basal (Long-Acting) Insulin: Think of this as your “background” insulin. Taken once or twice a day, it keeps your blood sugar stable overnight and between meals. It provides a steady, low level of insulin to handle the sugar your liver releases naturally.
2. Bolus (Rapid-Acting) Insulin: This is “mealtime” insulin. It works very quickly to handle the spike in glucose that occurs when you eat carbohydrates.
Modern insulin analogs are much more stable and predictable than older versions, allowing for flexibility in lifestyle and diet. While it requires more monitoring and carries a higher risk of hypoglycemia if the dose doesn’t match the food intake, insulin is the most potent agent available for lowering blood sugar.
DPP-4 Inhibitors and Sulfonylureas
While the newer drugs get a lot of attention, we shouldn’t overlook the “supporting cast” of diabetes medications: DPP-4 inhibitors and Sulfonylureas.
DPP-4 Inhibitors (like Januvia or Tradjenta) are oral medications that help the body continue to make insulin when it’s needed and reduce the amount of glucose being produced by the liver. They are generally “weight neutral” (they won’t cause weight gain) and are very well tolerated with few side effects. They are a great middle-ground option for patients who cannot tolerate Metformin or who need a little extra help without the intensity of injectable drugs.
Sulfonylureas (like Glipizide or Glimepiride) have been around for a very long time. They work by stimulating the pancreas to release more insulin. They are extremely effective at lowering blood sugar and are very inexpensive, often costing practically nothing with insurance.
However, there are trade-offs. Sulfonylureas carry a higher risk of hypoglycemia because they tell the pancreas to squeeze out insulin regardless of whether your sugar is currently high or low. They can also cause some weight gain. Doctors often have to balance the benefit of the low cost against these risks, usually reserving them for patients where cost is a major barrier or other medications haven’t worked well enough.
Choosing the Best Medication for You
So, with all these options, how do you and your doctor choose? There is no “one size fits all” pill. The decision is a personalized puzzle that considers your unique biological makeup and lifestyle.
First, doctors look at your A1C levels (your three-month average blood sugar). If it is very high, they may need to start with stronger therapies like insulin or combination drugs immediately. If it is only slightly elevated, lifestyle changes plus Metformin might be enough.
Kidney function is another major factor. Some medications, like Metformin, require dose adjustments or must be stopped if kidney function drops too low, whereas others, like SGLT2 inhibitors, are specifically prescribed to help protect the kidneys (up to a certain point).
Side effect tolerance is also key. If you have a sensitive stomach, your doctor might avoid GLP-1 agonists or start them very slowly. If you have a history of frequent yeast infections, SGLT2 inhibitors might be avoided as they can increase that risk.
Finally, we must talk about the practical side: cost and insurance. The newest drugs (GLP-1s and SGLT2s) can be expensive without good insurance coverage. Balancing your health goals with your financial reality is a valid and important part of the conversation.
The landscape of diabetes treatment has expanded significantly, offering options that not only manage blood sugar but also protect vital organs and aid in weight management. While Metformin remains the standard starting point for many, newer therapies like GLP-1 agonists and SGLT2 inhibitors are redefining what the “best” treatment looks like for complex cases. Always consult your healthcare provider to tailor a medication plan that aligns with your specific health profile and lifestyle needs.
Frequently Asked Questions
What is considered the first-choice medication for type 2 diabetes?
Metformin is widely regarded by medical professionals as the “gold standard” and first-line therapy for most people diagnosed with type 2 diabetes. It is favored because it is highly effective at lowering blood sugar, affordable, and carries a low risk of causing hypoglycemia (low blood sugar) compared to other drugs. Additionally, it helps improve the body’s sensitivity to insulin and may assist with modest weight management.
Which diabetes medications are best for significant weight loss?
GLP-1 receptor agonists, such as semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro), are currently considered the most effective diabetic medications for weight loss. These injectable treatments work by mimicking hormones that signal fullness and slow down digestion, leading to reduced calorie intake. Because obesity is a major risk factor for diabetes complications, these drugs are often prescribed to patients who need to lower their A1C and lose weight simultaneously.
How do SGLT2 inhibitors compare to other diabetic treatments?
SGLT2 inhibitors (like Jardiance and Farxiga) are unique because they lower blood sugar by preventing the kidneys from reabsorbing glucose, allowing it to be excreted through urine. They are often ranked as the best option for diabetic patients who also have heart failure or chronic kidney disease, as studies show they offer significant cardiovascular and renal protective benefits. Unlike insulin, they do not typically cause weight gain and can actually lower blood pressure.
What is the best diabetic medication for patients worried about hypoglycemia?
Medications that are “glucose-dependent,” such as DPP-4 inhibitors (Januvia) and GLP-1 agonists, are generally the safest options for avoiding dangerous drops in blood sugar. Unlike sulfonylureas or insulin, which can force blood sugar down regardless of current levels, these newer medications only stimulate insulin production when glucose levels are actually high. This makes them an excellent choice for elderly patients or those with irregular eating schedules.
When is insulin the best treatment option over oral medications?
Insulin is the necessary and best treatment for all people with type 1 diabetes and becomes essential for type 2 diabetics when the pancreas can no longer produce enough insulin to manage blood sugar levels. While many prefer oral pills for convenience, insulin remains the most potent agent for rapidly bringing down very high A1C levels and preventing immediate toxicity. Doctors often prescribe it when multiple oral medications fail to keep glucose within a target range.
References
- Diabetes treatment: Medications for type 2 diabetes – Mayo Clinic
- Insulin, Medicines, & Other Diabetes Treatments – NIDDK
- Diabetes Medicine | Insulin | MedlinePlus
- https://my.clevelandclinic.org/health/drugs/12170-oral-diabetes-medications
- https://www.nhs.uk/conditions/type-2-diabetes/medicine/
- What Are My Options for Type 2 Diabetes Medications? | ADA
- https://www.fda.gov/consumers/consumer-updates/diabetes-medicines
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes/oral-medicines-for-diabetes
- Not Found | American Heart Association | American Heart Association