For individuals with Type 2 Diabetes, Continuous Glucose Monitors (CGMs) offer a revolutionary way to track blood sugar, providing real-time data far beyond traditional fingersticks. While there isn’t a single “best” CGM for everyone, leading contenders like the Dexcom G7/G6 and FreeStyle Libre 3/2 are highly recommended, each offering unique features that can significantly improve diabetes management. The ideal CGM for you will depend on your specific needs, lifestyle, and preferences, always in consultation with your healthcare provider.
Understanding CGMs and Their Value for Type 2 Diabetes

Stepping into the world of CGMs can feel like gaining a superpower for managing your Type 2 Diabetes! These incredible devices take the guesswork out of blood sugar monitoring, giving you a continuous stream of insights into what’s happening inside your body.
* Continuous Glucose Monitoring Explained: Imagine having a tiny, discreet health assistant working 24/7 to keep an eye on your glucose levels. That’s essentially what a CGM does! It uses a small, disposable sensor inserted just under the skin – typically on your arm or abdomen – to measure glucose levels in the interstitial fluid (the fluid surrounding your cells) every few minutes, day and night. This sensor is connected to a transmitter that wirelessly sends data to a compatible smartphone app or a dedicated receiver, giving you a near real-time snapshot of your glucose trends without constant interruptions.
* Beyond Fingersticks: While traditional fingerstick tests provide a momentary “snapshot” of your blood sugar at a specific time, they miss a whole lot of the picture. CGMs, however, allow you to see the full story. You’ll discover how your glucose levels fluctuate throughout the day and night, identifying peaks and valleys that fingersticks might never catch. This continuous data helps you understand the direct impact of different foods, specific exercises, stress, sleep, and even medication timing on your blood sugar, moving you beyond guesswork to genuine understanding.
* Empowering Self-Management: The real magic of CGMs lies in their ability to empower you. By seeing your glucose levels in real time, along with trend arrows indicating whether they’re rising, falling, or stable, you can make informed, proactive decisions. This incredible insight can help prevent dangerous highs (hyperglycemia) and lows (hypoglycemia) before they become severe, optimize medication timing in collaboration with your doctor, and guide lifestyle adjustments – like choosing a different snack or taking a short walk after a meal – for better blood sugar control and, ultimately, a healthier A1C.
Leading CGM Systems for Type 2 Diabetes
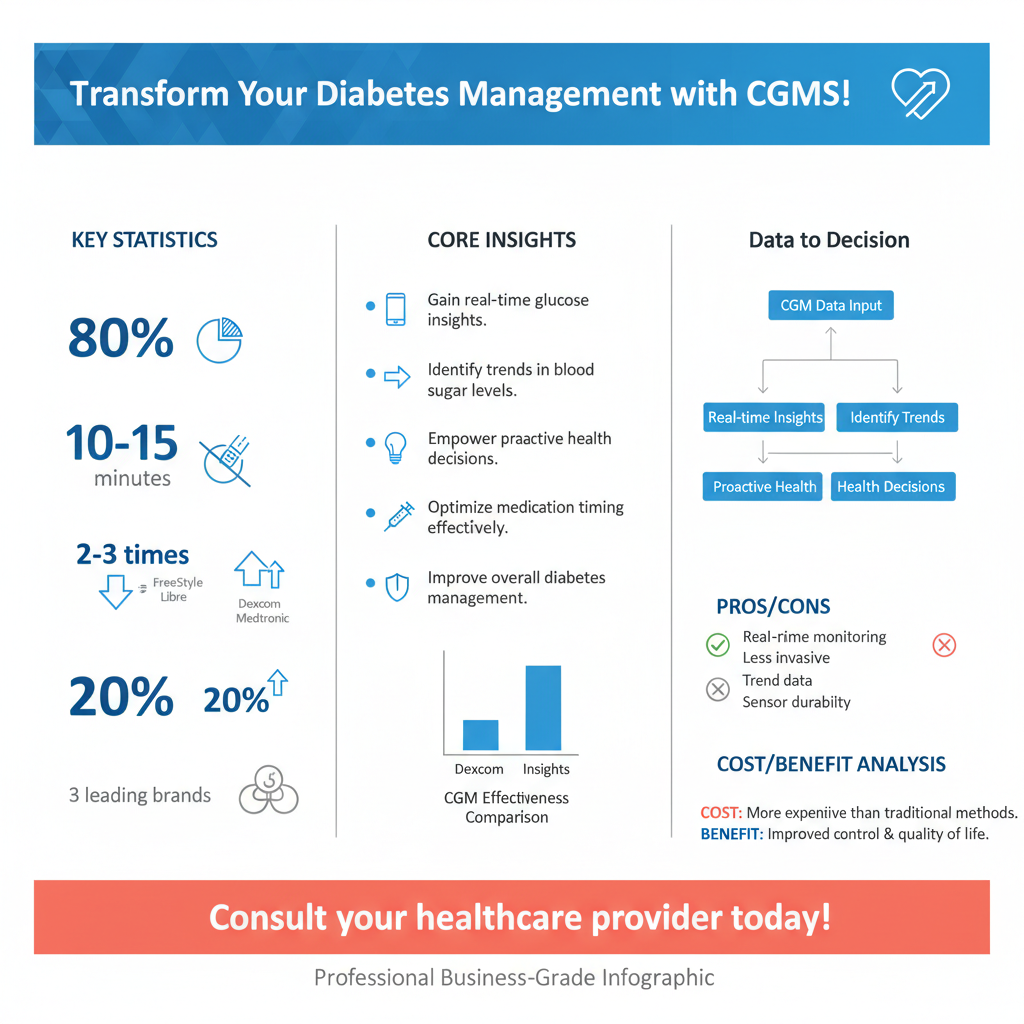

When it comes to choosing a CGM, two names frequently rise to the top for their reliability and user-friendly features: Dexcom and FreeStyle Libre. Let’s take a closer look at what makes each of them stand out.
* Dexcom G7 & G6: Dexcom systems are renowned for their high accuracy and robust alerting features. The Dexcom G7 is their latest innovation, boasting an even smaller, all-in-one sensor (no separate transmitter needed!) that’s incredibly discreet and has a super-fast 30-minute warm-up time. It offers 10 days of continuous wear. The Dexcom G6, still widely used and highly effective, also provides 10 days of wear with a separate sensor and transmitter. Both the G7 and G6 are known for their predictive alerts, which can warn you when your glucose is trending high or low *before* it reaches a critical level, giving you time to intervene. They send real-time readings directly to your smartphone, and offer robust data-sharing options, allowing family members or caregivers to remotely monitor your glucose levels – a fantastic feature for peace of mind.
* FreeStyle Libre 3 & 2: Abbott’s FreeStyle Libre systems are celebrated for their simplicity, smaller size, and generally more accessible price point. The FreeStyle Libre 3 is currently the smallest and most discreet CGM sensor available, roughly the size of two stacked pennies. It provides minute-by-minute real-time readings *pushed* automatically to your smartphone and offers an impressive 14-day wear time. Crucially, it requires absolutely no fingerstick calibrations, ever! The FreeStyle Libre 2 also offers a 14-day wear time and doesn’t require fingerstick calibrations; however, it’s an “on-demand” system, meaning you scan the sensor with your smartphone to get your current glucose reading. It does offer optional high/low glucose alarms without requiring a scan. Both Libre systems are incredibly easy to apply and designed for comfort.
* Key Differences: When comparing these systems, a few key distinctions come to light. The most significant difference between Libre 2 and the others is the “on-demand” scanning versus real-time “push” data. While Libre 3, Dexcom G7, and G6 continuously send data to your device, Libre 2 requires you to actively scan the sensor to see your current reading (though alarms still function automatically). In terms of wear duration, Libre systems offer 14 days, while Dexcom offers 10 days. Dexcom is often lauded for its predictive low/high alerts and advanced data sharing, making it a strong choice for those who need comprehensive warnings and remote monitoring. Libre systems, especially Libre 3, excel in discreetness, ease of application, and longer wear time without calibration, appealing to users looking for maximum simplicity and comfort.
Key Features to Consider When Choosing Your CGM

Selecting the perfect CGM is a bit like choosing a car – there are many great options, but the “best” one fits your specific needs and lifestyle. Here are some essential features to keep in mind.
* Accuracy and Reliability: This is paramount. You need to trust the numbers your CGM provides to make safe and effective decisions about your diabetes management. Always prioritize systems with clinically proven accuracy, often measured by a low Mean Absolute Relative Difference (MARD) value. A consistently reliable CGM means you can confidently adjust your diet, exercise, or medication (under medical guidance) knowing the data is sound. Look for systems that maintain their accuracy throughout the entire wear period, from day one to the last day.
* Wear Time and Comfort: Think about how long you want to wear a sensor before needing to replace it. CGMs typically offer wear times ranging from 10 to 15 days, with 10 or 14 days being most common. Longer wear times mean fewer applications, which can be a huge convenience. Equally important is the comfort and discreetness of the sensor on your body. Will it be noticeable under clothing? Will it bother you during sleep or exercise? Look for small, low-profile sensors that adhere securely without causing irritation, allowing you to forget you’re even wearing it while you go about your daily life, showering and exercising with ease.
* Alerts, Connectivity, and Integration: Modern CGMs are smart devices, and their ability to connect and alert you is a game-changer. Consider the types of alerts offered: customizable high and low glucose alerts are standard, but some systems also provide urgent low glucose alerts, predictive alerts (warning you *before* you go too low or high), and even rate-of-change alerts. Connectivity to a user-friendly smartphone app is crucial for viewing your data, trends, and reports. Also, think about integration capabilities: Can you share your data easily with family members, caregivers, or your healthcare provider? Some systems can even integrate with insulin pumps, offering an even more seamless management experience.
Maximizing CGM Benefits for Type 2 Management
Getting a CGM is just the first step; unlocking its full potential involves actively engaging with your data and collaborating with your healthcare team. This proactive approach can transform how you manage Type 2 Diabetes.
* Interpreting Your Data: Your CGM provides a wealth of information, but understanding what it all means is key. Take time to learn how to analyze your glucose trends, paying attention to the arrows that indicate if your levels are rising, falling, or stable. Look for patterns: Do certain foods consistently cause spikes? How does a morning walk impact your blood sugar compared to an evening workout? Identifying triggers for sudden dips or prolonged highs allows you to understand your body’s unique responses to diet, activity, stress, and medication. Focus on your “Time in Range” (TIR) – the percentage of time your glucose stays within your target range – as a powerful metric for overall control.
* Collaborating with Your Healthcare Team: Your CGM data is an invaluable tool for your doctor, dietitian, or diabetes educator. Don’t just show up to appointments; bring your CGM reports or share your data access with them! These comprehensive reports (often called Ambulatory Glucose Profiles or AGP reports) offer a holistic view of your glucose patterns, far beyond a single A1C number. They can help your team make more informed decisions about adjusting medication dosages or timing, refining your dietary plan to minimize spikes, or optimizing your exercise routines for better glucose stability. This partnership ensures your management plan is truly personalized and effective.
* Proactive Lifestyle Adjustments: One of the most empowering aspects of CGM use is the ability to make immediate, proactive changes. Seeing your glucose trending high after a particular meal might prompt you to take a brisk walk immediately, rather than waiting for hours. If you notice consistent morning highs, you and your doctor can discuss adjusting evening medication. Over time, these real-time insights lead to lasting lifestyle modifications. You’ll learn which foods agree with your body, the best times for exercise, and how small behavioral changes can maintain glucose levels within your target range, leading to improved energy, reduced complications, and overall better health outcomes.
Navigating Cost, Insurance, and Prescriptions
Understanding the financial and logistical aspects of obtaining a CGM is crucial, as these devices represent a significant investment in your health. Don’t let these factors deter you; many resources are available.
* Insurance Coverage: This is often the biggest hurdle, as insurance coverage for CGMs for Type 2 Diabetes can vary widely depending on your specific plan and provider. Historically, CGMs were primarily covered for individuals with Type 1 Diabetes or Type 2 Diabetes on intensive insulin therapy. However, coverage is expanding! Many plans now recognize the value of CGMs for Type 2 management, especially if you can demonstrate medical necessity (e.g., a history of problematic hypoglycemia, poor A1C control despite other efforts, or other significant risk factors). It’s essential to call your insurance provider directly, ask about their specific criteria for CGM coverage, and be prepared to work with your doctor to provide the necessary documentation.
* The Prescription Process: Regardless of insurance, a healthcare provider’s prescription is almost always required to obtain a CGM system. This typically involves a consultation with your endocrinologist, primary care physician, or diabetes specialist. During this visit, you’ll discuss your diabetes management history, current glucose control, and why a CGM would be beneficial for your specific situation. Your doctor will assess whether a CGM is medically appropriate for you and then write the necessary prescription, which you can take to your pharmacy or a durable medical equipment (DME) supplier.
* Affordability and Patient Programs: Even with insurance, out-of-pocket costs can be a concern. Thankfully, many manufacturers offer patient assistance programs, savings cards, or trial periods to help reduce the financial burden. Websites like those for Dexcom and FreeStyle Libre often have sections dedicated to helping patients navigate costs and find discounts. Don’t hesitate to ask your doctor or pharmacist about these programs. Comparing prices across different pharmacies can also sometimes yield savings. Remember, investing in a CGM can lead to better long-term health, potentially reducing future healthcare costs associated with diabetes complications.
Making the Right Choice with Your Healthcare Team
Choosing a CGM is a deeply personal decision, and the best way to ensure you make the right one is by having an open and honest conversation with your trusted healthcare team. They are your greatest allies in this journey!
* Personalized Recommendation: There’s no one-size-fits-all “best” CGM, because *you* are unique! Your doctor or diabetes educator understands your specific medical history, treatment goals, and current lifestyle. Are you highly active? Do you have dexterity challenges? Are you comfortable with smartphone apps, or would you prefer a dedicated receiver? Do you travel frequently? Discuss your daily routines, tech comfort level, budget considerations, and what you hope to gain from using a CGM. They can offer a personalized recommendation based on their clinical experience and your individual needs, helping you weigh the pros and cons of each system as it applies to you.
* Trial Periods and Training: Don’t be afraid to ask about trial periods or starter kits for different CGM systems. Sometimes experiencing a device firsthand is the best way to know if it’s the right fit. Many clinics also offer valuable training resources to help you get started confidently. This might include hands-on guidance for applying the sensor, navigating the smartphone app, and understanding the basic interpretation of your glucose data. A diabetes educator can be an invaluable resource, providing practical tips and support to ensure you feel comfortable and empowered from day one.
* Long-Term Support: Your relationship with your CGM and your healthcare provider doesn’t end after you’ve received your prescription. To achieve the best results, you’ll need ongoing support. This includes regular follow-up appointments to discuss your CGM data, refine your understanding of trends, troubleshoot any sensor issues or technical glitches, and adjust your diabetes management plan as needed. As your body changes or your goals evolve, your healthcare team can help you continue to maximize the benefits of your chosen CGM system, ensuring it remains an effective tool for your long-term health and well-being.
Choosing the best CGM for Type 2 Diabetes is a personal decision that can profoundly impact your glucose management and overall well-being. By considering the leading systems, evaluating key features, and discussing your individual needs with your healthcare team, you can select a device that empowers you to take control of your health. Don’t hesitate to consult your doctor or diabetes educator today to explore which CGM is the right fit for you and embark on a more informed path to managing your Type 2 Diabetes.
Frequently Asked Questions
What are the primary benefits of using a CGM for managing Type 2 diabetes?
Continuous Glucose Monitors (CGMs) offer significant advantages for Type 2 diabetes management by providing real-time glucose data, enabling immediate insights into how food, exercise, and stress impact blood sugar levels. This constant feedback helps identify patterns, prevent highs and lows, and empower individuals to make informed lifestyle adjustments. Ultimately, using a CGM for Type 2 diabetes can lead to improved glycemic control, reduced A1C, and a better understanding of one’s body.
Which continuous glucose monitors (CGMs) are generally considered best for Type 2 diabetes, and how do they compare?
For Type 2 diabetes, the Dexcom G7 and FreeStyle Libre 3 are widely considered leading CGM options due to their accuracy and user-friendly designs. The FreeStyle Libre 3 is often praised for its small size, direct-to-smartphone readings, and affordability, while the Dexcom G7 offers highly accurate real-time data with customizable alarms and robust connectivity. Both provide valuable insights, but the “best CGM for Type 2 diabetes” often depends on individual preferences for features, sensor wear time, and insurance coverage.
How does a CGM help Type 2 individuals understand their blood sugar responses to food and exercise?
A CGM provides a continuous stream of glucose readings, allowing Type 2 individuals to observe immediate and delayed effects of meals and physical activity. By logging food intake or exercise alongside the CGM data, users can pinpoint which foods cause significant spikes, how different exercise intensities affect levels, and the optimal timing for activities relative to meals. This personalized feedback is invaluable for fine-tuning diet and exercise plans to maintain stable blood sugar and optimize Type 2 diabetes management.
Is a CGM covered by insurance for Type 2 diabetes patients, and what are the typical costs?
Insurance coverage for CGMs for Type 2 diabetes patients has significantly expanded, though it often requires specific criteria, such as being on insulin or having a history of problematic hypoglycemia. Out-of-pocket costs can vary widely; without insurance, a month’s supply of sensors might range from $70-$150 for systems like FreeStyle Libre, while Dexcom G7 might be higher, often requiring a separate transmitter in addition to sensors. It’s crucial to check with your specific insurance provider and healthcare team to understand your eligibility and anticipated expenses for a *CGM for Type 2 diabetes*.
What key features should I look for when choosing a CGM specifically for Type 2 diabetes management?
When selecting a *CGM for Type 2 diabetes*, prioritize features like high sensor accuracy, especially in both high and low glucose ranges, and a discreet, comfortable sensor size for everyday wear. Look for user-friendly apps that provide clear data visualization, customizable alerts for high or low glucose, and easy data sharing options. Consider sensor wear time (e.g., 10 or 14 days) and whether it offers direct-to-phone connectivity versus requiring a separate reader, as these factors greatly impact convenience and daily management.
References
- https://diabetesjournals.org/care/article/46/Supplement_1/S110/148002/9-Pharmacologic-Approaches-to-Glycemic-Treatment
- https://diabetes.org/tools-resources/cgm
- Continuous Glucose Monitoring – NIDDK
- https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/cgm/art-20044365
- https://www.cdc.gov/diabetes/managing/cgm.html
- https://www.health.harvard.edu/blog/continuous-glucose-monitoring-the-future-of-diabetes-care-202302062886
- Continuous glucose monitor
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8900010/