Navigating the best diet for Type 2 diabetes can feel overwhelming, but the most effective approach centers on a balanced intake of whole, unprocessed foods, strategic carbohydrate management, and consistent eating patterns to stabilize blood sugar levels, manage weight, and support overall health. This isn’t about restrictive dieting, but rather adopting sustainable eating habits that empower you to take control of your health and reduce the risk of diabetes complications. It’s about making informed choices that nourish your body, improve insulin sensitivity, and foster long-term well-being, turning a challenging diagnosis into an opportunity for a healthier lifestyle.
Understanding the Core Goals of a Diabetes Diet

When you’re managing Type 2 diabetes, your diet becomes a powerful tool. Understanding the key objectives behind dietary recommendations can help you make more informed and motivated choices. It’s not just about what you eat, but why.
– Blood Sugar Management: This is often the immediate concern for anyone living with diabetes. The primary goal is to maintain stable blood glucose levels, preventing dangerous spikes and drops throughout the day. Consistently high blood sugar (hyperglycemia) can damage nerves, kidneys, eyes, and blood vessels over time, leading to serious long-term complications. By carefully selecting foods that release glucose slowly and consistently, you can keep your energy levels steady, reduce symptoms like fatigue and blurred vision, and protect your organs from damage. Think of it as keeping your body’s internal thermostat precisely regulated.
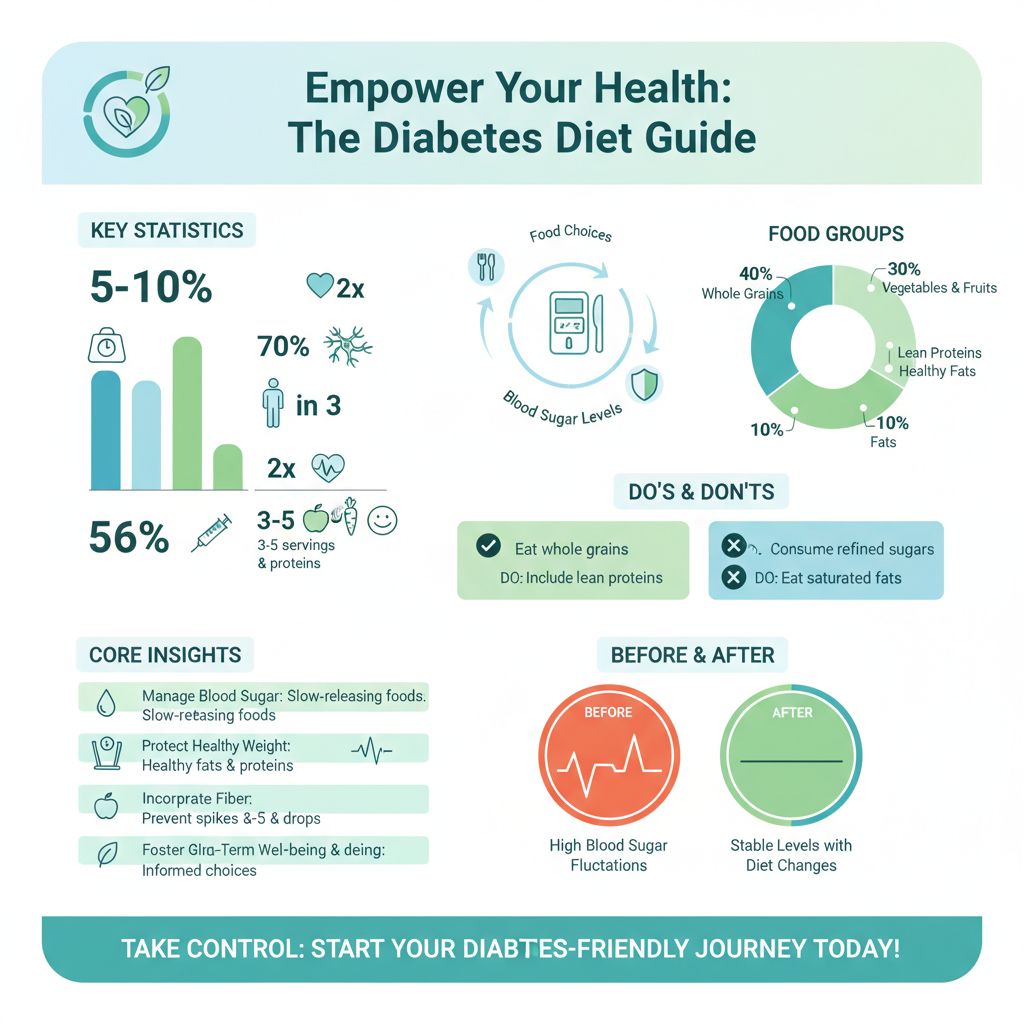
– Weight Management: Achieving and maintaining a healthy weight significantly improves insulin sensitivity and can even lead to diabetes remission for some individuals. Excess body fat, particularly around the abdomen, can lead to insulin resistance, making it harder for your cells to respond to insulin and absorb glucose from the blood. Losing even a modest amount of weight (5-10% of your body weight) can dramatically improve blood sugar control, lower blood pressure, and reduce cholesterol levels. It’s a cornerstone of diabetes management, offering profound benefits beyond just aesthetic appeal.
– Cardiovascular Health: A diabetes-friendly diet also aims to reduce the risk factors for heart disease, a common complication of diabetes, by managing cholesterol and blood pressure. People with Type 2 diabetes are at a significantly higher risk of heart attack, stroke, and other cardiovascular problems. This is because high blood sugar can damage blood vessels, leading to inflammation and plaque buildup. A diet rich in healthy fats, lean proteins, and fiber, while low in unhealthy fats and added sugars, directly supports a healthy heart. It helps lower “bad” LDL cholesterol, raise “good” HDL cholesterol, and maintain healthy blood pressure, providing comprehensive protection for your most vital organ.
Building a Diabetes-Friendly Plate

Picture your plate at mealtime – how does it look? A simple, visual approach can make healthy eating for diabetes much easier and more intuitive. It’s all about balance and smart choices for each component of your meal.
– Focus on Non-Starchy Vegetables: Make these vibrant powerhouses the star of your plate, filling half of it with colorful vegetables like leafy greens (spinach, kale), broccoli, cauliflower, bell peppers, asparagus, green beans, and cucumbers. These vegetables are incredibly low in calories and carbohydrates, yet bursting with essential vitamins, minerals, antioxidants, and most importantly, fiber. They add volume to your meals, helping you feel full and satisfied without impacting your blood sugar significantly. Sauté them, roast them, steam them, or enjoy them raw in salads – the more variety, the better!
– Lean Proteins are Key: Dedicate about a quarter of your plate to lean protein sources. These include skinless chicken breast, fish (salmon, tuna, cod, sardines), tofu, tempeh, legumes (lentils, black beans, chickpeas), and lean cuts of beef or pork. Protein helps with satiety, meaning it keeps you feeling fuller for longer, which can prevent overeating and snacking on less healthy options. It also plays a crucial role in muscle maintenance and repair, and importantly, it has a minimal impact on blood sugar levels compared to carbohydrates. Incorporating protein at each meal helps slow down the digestion of any carbohydrates you consume, leading to a more gradual rise in blood glucose.
– Incorporate Healthy Fats: Don’t shy away from fats, but choose them wisely! Healthy fats are vital for supporting heart health, reducing inflammation, and providing long-lasting energy. Focus on monounsaturated and polyunsaturated fats found in avocados, nuts (almonds, walnuts), seeds (chia, flax, sunflower), and olive oil. These fats can help lower “bad” LDL cholesterol and raise “good” HDL cholesterol, which is particularly beneficial for individuals with diabetes who are at an increased risk for cardiovascular disease. Use olive oil for cooking, add a slice of avocado to your salad, or snack on a small handful of nuts for a satisfying boost of healthy fats.
Smart Carbohydrate Choices and Portion Control

Carbohydrates are the primary nutrient that impacts blood sugar, but they’re not the enemy! The key is to make smart choices and manage portions. It’s about quality over quantity.
– Prioritize Complex Carbohydrates: Opt for whole grains such as oats, quinoa, brown rice, whole-wheat bread, and farro, as well as starchy vegetables like sweet potatoes and corn, and legumes like lentils and black beans. These complex carbohydrates are high in fiber and digest slowly, leading to a more gradual and stable rise in blood sugar compared to refined carbohydrates. They provide sustained energy, essential nutrients, and contribute to overall digestive health. Always choose the whole-grain version over refined options to maximize fiber and nutritional benefits.
– Mind Your Portions: Even healthy carbohydrates need careful attention to portion sizes. Carbohydrate counting or consistent carbohydrate intake can be vital for managing blood sugar levels effectively. Learn appropriate portion sizes for carb-rich foods to avoid overloading your system. For instance, a serving of cooked grains like brown rice or quinoa is typically about 1/2 cup, and a slice of whole-wheat bread is one serving. Using measuring cups, food scales, or even simple hand portioning (e.g., a cupped hand for grains) can help you stay on track and ensure your blood sugar remains within target ranges.
– Fiber is Your Friend: We can’t say it enough – fiber is incredibly beneficial for diabetes management. High-fiber foods, found in whole grains, vegetables, fruits, and legumes, slow down sugar absorption into the bloodstream, which prevents rapid blood sugar spikes. Fiber also improves gut health, promotes regularity, and contributes significantly to feelings of fullness, aiding in weight management. Aim for a variety of fiber sources in your diet daily to reap these comprehensive benefits.
Foods to Limit or Avoid for Better Blood Sugar
Just as important as knowing what to eat is understanding what to limit or steer clear of to best manage your blood sugar and overall health. These foods tend to work against your goals.
– Minimize Added Sugars and Sweetened Beverages: This is perhaps one of the most crucial changes. Sugary drinks (soda, sweetened teas, fruit juices with added sugar), candies, pastries, desserts, and many processed snacks are loaded with added sugars. These sugars cause rapid and dramatic blood sugar spikes because they are quickly absorbed into the bloodstream, offering little to no nutritional value. Consuming them regularly can lead to insulin resistance and weight gain. Read food labels carefully to spot hidden sugars like high-fructose corn syrup, dextrose, and maltose. Opt for water, unsweetened tea, or coffee instead.
– Reduce Refined Grains: Foods made with refined grains, such as white bread, white pasta, many processed cereals, and white rice, have had their fiber and nutrient-rich bran and germ removed during processing. This makes them digest quickly, causing a rapid rise in blood sugar levels, similar to pure sugar. They lack the valuable fiber that helps slow down glucose absorption and provide fewer essential nutrients. Swapping these for their whole-grain counterparts is a simple yet impactful step towards better blood sugar control.
– Limit Unhealthy Fats: While healthy fats are encouraged, trans fats and excessive saturated fats can negatively impact heart health and insulin resistance, which are particularly concerning for individuals with diabetes. Trans fats, often found in fried foods, baked goods (like commercial cookies, cakes, and crackers), and some processed snacks, raise “bad” LDL cholesterol and lower “good” HDL cholesterol, significantly increasing heart disease risk. Saturated fats, found in fatty meats, full-fat dairy, and some tropical oils (like coconut and palm oil), should also be consumed in moderation. Choose lean proteins and opt for plant-based fats whenever possible.
The Importance of Consistent Meal Patterns
It’s not just about what you eat, but when and how often. Establishing a routine for your meals and snacks can be a game-changer for blood sugar stability.
– Regular Meal Times: Eating meals and snacks at consistent times each day helps your body regulate blood sugar and insulin levels more effectively, preventing extreme fluctuations. When your body knows when to expect food, it can better anticipate and manage glucose release and uptake. This consistent rhythm helps your pancreas release insulin more efficiently and prevents both low blood sugar (hypoglycemia) and high blood sugar (hyperglycemia) caused by erratic eating. Aim for roughly the same meal schedule every day, even on weekends.
– Don’t Skip Meals: Skipping meals, especially breakfast, can lead to your blood sugar dropping too low, causing symptoms like dizziness, fatigue, and irritability. This often results in overeating at the next meal, leading to a rebound spike in blood sugar that is harder to control. Skipping meals can also mess with your metabolism and make weight management more challenging. Plan your meals and snacks ahead of time to ensure you’re nourishing your body consistently throughout the day.
– Strategize Snacks: If you need snacks to manage hunger or blood sugar between meals, choose them wisely and purposefully. Opt for nutrient-dense options that combine protein and fiber to keep hunger at bay and blood sugar stable. Good choices include a handful of nuts, a piece of fruit with a small amount of cheese or nut butter, Greek yogurt with berries, or vegetable sticks with hummus. Avoid sugary or highly processed snacks that will only lead to a quick spike and subsequent crash.
Hydration and Lifestyle Factors
Diet is a huge piece of the puzzle, but it’s not the only one. Holistic lifestyle choices play a critical role in supporting your diabetes management efforts.
– Stay Well-Hydrated: Water is absolutely the best beverage choice for hydration; it has no carbohydrates, no calories, and can help manage blood sugar by preventing dehydration, which can concentrate blood glucose. Drinking plenty of water also aids in kidney function, helping them flush out excess glucose. Make water your primary drink, and limit or completely avoid sugary drinks, including fruit juices, which are high in natural sugars and can spike blood sugar. Keep a water bottle handy throughout the day as a constant reminder to sip.
– Incorporate Physical Activity: Regular exercise, combined with a healthy diet, is crucial for improving insulin sensitivity and managing blood glucose. When you exercise, your muscles use glucose for energy, which helps lower blood sugar levels. Physical activity can also help with weight management, reduce stress, improve cardiovascular health, and boost your mood. Aim for at least 150 minutes of moderate-intensity aerobic activity per week (like brisk walking, swimming, or cycling) and incorporate strength training exercises at least twice a week. Even small bouts of movement throughout the day, like taking a short walk after meals, can make a difference.
– Prioritize Sleep and Stress Management: The connection between sleep, stress, and blood sugar control is often underestimated but profoundly important. Poor sleep can disrupt hormones that regulate appetite and insulin sensitivity, leading to higher blood sugar levels. Similarly, chronic stress triggers the release of hormones like cortisol, which can raise blood glucose. Making sleep a priority (aim for 7-9 hours of quality sleep per night) and practicing stress-reducing techniques such as meditation, deep breathing exercises, yoga, or spending time in nature can significantly support your diabetes management. Taking care of your mental and emotional well-being is just as vital as your physical health.
Ultimately, finding the “best” diet for Type 2 diabetes is a personalized journey that emphasizes whole foods, balanced macronutrients, and mindful eating habits. While general principles apply, consistent effort in managing carbohydrate intake, prioritizing lean proteins and healthy fats, and incorporating plenty of non-starchy vegetables will set you on the path to better health. Remember, this is a marathon, not a sprint. Each small, positive dietary and lifestyle change contributes to a cumulative benefit, empowering you to effectively manage your diabetes and enjoy a vibrant, healthy life. Always consult with your doctor or a registered dietitian to create an individualized eating plan that aligns with your specific health needs, preferences, and medication regimen. They can provide tailored guidance and support to help you achieve your goals safely and effectively.
Frequently Asked Questions
What is the best overall diet approach for managing Type 2 diabetes effectively?
The most effective diet for managing Type 2 diabetes emphasizes whole, unprocessed foods and focuses on blood sugar control. Generally, a balanced eating plan rich in non-starchy vegetables, lean proteins, healthy fats, and complex carbohydrates from whole grains and legumes is recommended. This approach helps stabilize glucose levels, manage weight, and reduce the risk of diabetes complications. Consulting a registered dietitian can help tailor a personalized diabetes-friendly diet plan.
How can a low-carb diet help in managing Type 2 diabetes symptoms and blood sugar?
A low-carb diet can significantly help manage Type 2 diabetes by reducing the amount of glucose entering the bloodstream, thus lowering blood sugar levels and insulin requirements. By limiting foods high in carbohydrates like sugary drinks, refined grains, and starchy vegetables, individuals can experience improved glycemic control and potentially reduce medication needs. This dietary strategy can also aid in weight loss, which is often beneficial for diabetes management and overall metabolic health.
Which specific foods should I avoid or significantly limit if I have Type 2 diabetes?
To effectively manage Type 2 diabetes, it’s crucial to limit or avoid foods that cause rapid spikes in blood sugar. This includes sugary beverages, refined grains (white bread, pasta, pastries), processed snacks, and foods high in saturated and trans fats. Additionally, be mindful of hidden sugars in condiments, sauces, and low-fat products, as these can negatively impact your blood glucose control. Prioritizing whole, nutrient-dense options over highly processed items is key.
Why is fiber important for individuals with Type 2 diabetes, and what are good sources?
Fiber is incredibly important for individuals with Type 2 diabetes because it helps slow the absorption of sugar into the bloodstream, preventing rapid blood glucose spikes and promoting stable energy levels. Additionally, fiber contributes to satiety, aiding in weight management, and supports gut health. Excellent sources of dietary fiber include non-starchy vegetables (broccoli, spinach), legumes (lentils, beans), whole grains (oats, quinoa), and fruits with edible skins (berries, apples).
Can diet alone reverse or put Type 2 diabetes into remission?
While diet alone cannot universally “reverse” Type 2 diabetes in all cases, a well-structured and consistent dietary intervention, particularly combined with weight loss, can lead to diabetes remission for many individuals. Remission means achieving and maintaining normal blood sugar levels without medication. Intensive lifestyle changes, often involving significant calorie restriction and carbohydrate management, have shown promising results in restoring insulin sensitivity and improving overall metabolic health in those committed to the regimen.
References
- https://diabetes.org/healthy-living/recipes-nutrition/eating-healthy
- https://www.niddk.nih.gov/health-information/diabetes/overview/diet-eating-physical-activity
- https://www.cdc.gov/diabetes/managing/eat-well.html
- Diabetes diet: Create your healthy-eating plan – Mayo Clinic
- https://www.hsph.harvard.edu/nutritionsource/disease-prevention/diabetes-prevention/type-2-diabetes-diet-sheet/
- Diet in diabetes
- https://health.clevelandclinic.org/what-is-the-best-diet-for-diabetes/
- Not Found | American Heart Association | American Heart Association
- https://www.nhs.uk/conditions/type-2-diabetes/food-and-diet/


