The “best” medicine for Diabetes Type 2 isn’t a single magic pill; rather, it’s a dynamic, personalized combination of lifestyle changes and medications precisely tailored to your unique health profile, existing conditions, and specific treatment goals. While Metformin often takes the stage as the initial, first-line therapy due to its widespread effectiveness, impressive safety record, and affordability, a robust array of other oral and injectable medications are available, each bringing unique benefits and considerations to the table for effectively managing blood sugar, actively preventing complications, and genuinely improving your overall long-term health.
The Foundational Approach: Lifestyle & Metformin

When it comes to managing Type 2 Diabetes, it’s like building a strong house – you need a solid foundation. This foundation isn’t just about medication; it starts with how you live your life every day.
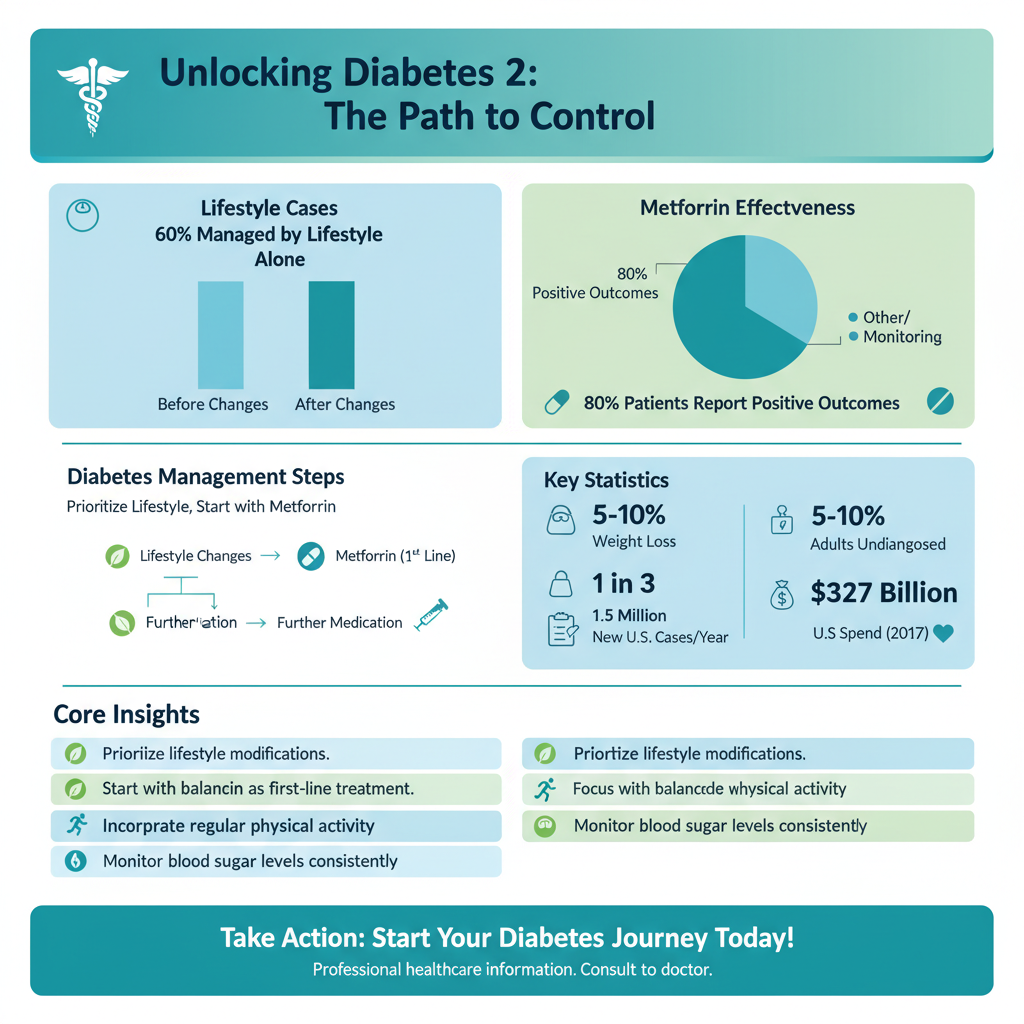
* Lifestyle Modifications are Key: Before we even talk about prescriptions, the most impactful steps you can take are centered around your daily habits. Think of diet changes as your primary fuel adjustment. This often means focusing on reducing refined carbohydrates and added sugars, increasing your intake of fiber-rich foods like vegetables, fruits, and whole grains, and paying attention to portion sizes. These adjustments help stabilize blood sugar levels and improve your body’s response to insulin. Beyond the plate, regular physical activity is a game-changer. It doesn’t mean you have to run a marathon; even consistent brisk walking, cycling, or strength training can significantly improve insulin sensitivity, help with weight management, boost cardiovascular health, and even lift your mood. Finally, weight management is incredibly crucial. Even a modest amount of weight loss (5-10% of your body weight) can dramatically improve blood sugar control and reduce the need for certain medications, sometimes even putting Type 2 Diabetes into remission. These lifestyle changes aren’t just “nice-to-haves”; they are often the most powerful tools in your diabetes management toolkit.
* Metformin: The First-Line Treatment: Once lifestyle changes are in motion, Metformin is typically the first medication prescribed if your blood sugar levels still need more help. It’s a true workhorse in the diabetes world, trusted by doctors and patients for decades. How does it work its magic? Primarily, Metformin targets the liver, reducing the amount of glucose it produces and releases into your bloodstream. Think of it as telling your liver to calm down a bit when it’s overproducing sugar. Additionally, it helps improve your body’s sensitivity to insulin, making your cells (like muscle and fat cells) more responsive to the insulin you do produce, allowing glucose to enter them more easily and lowering your blood sugar levels. It’s an efficient, well-understood medication that has helped countless people manage their Type 2 Diabetes.
* Benefits and Considerations: Metformin boasts an impressive list of benefits. It’s highly effective at lowering A1C (your average blood sugar over three months), generally very safe for most people, and incredibly cost-effective, making it accessible. Many people also experience a modest amount of weight loss, which is a welcome bonus for those managing Type 2 Diabetes. While it’s generally well-tolerated, it’s not without potential considerations. The most common side effects are gastrointestinal issues like nausea, diarrhea, and stomach upset, especially when first starting the medication. To help minimize these, doctors often advise starting with a low dose and gradually increasing it, and always taking it with food. These side effects often subside over time, but it’s always important to communicate with your doctor about any discomfort you experience.
Expanding Oral Options: SGLT2 Inhibitors & DPP-4 Inhibitors

When Metformin and lifestyle changes aren’t quite enough to reach your blood sugar targets, or if you have specific health considerations, your doctor might introduce other oral medications. Two popular and effective classes are SGLT2 inhibitors and DPP-4 inhibitors, each with unique mechanisms and benefits.
* SGLT2 Inhibitors (e.g., Empagliflozin, Dapagliflozin): These medications represent a newer generation of diabetes treatment, and they’ve been quite revolutionary due to their additional benefits beyond just blood sugar control. SGLT2 inhibitors work in a fascinating way: they target your kidneys. Normally, your kidneys reabsorb most of the glucose that filters through them back into your bloodstream. SGLT2 inhibitors block this reabsorption, causing your kidneys to remove more glucose from your body through your urine. This unique mechanism leads to lower blood sugar levels, but that’s not all. A truly significant benefit of SGLT2 inhibitors is their powerful protective effects on the heart and kidneys. Studies have shown they can reduce the risk of cardiovascular events (like heart attack and stroke) and slow the progression of chronic kidney disease in people with Type 2 Diabetes, making them a fantastic choice for those with these comorbidities. Other perks often include a modest amount of weight loss and a slight reduction in blood pressure. However, because they cause glucose to be excreted in urine, potential side effects can include an increased risk of urinary tract infections and yeast infections, and sometimes dehydration.
* DPP-4 Inhibitors (e.g., Sitagliptin, Linagliptin): If you’re looking for a medication that’s generally gentle and well-tolerated, DPP-4 inhibitors might be an option. These drugs work by tapping into your body’s natural systems to help manage blood sugar. They inhibit an enzyme called dipeptidyl peptidase-4 (DPP-4), which normally breaks down “incretin” hormones (like GLP-1 and GIP) in your gut. By blocking DPP-4, these medications allow incretin hormones to stick around longer. These hormones then stimulate your pancreas to release more insulin when blood sugar levels are high and reduce the amount of glucose produced by your liver. Because their action is glucose-dependent, they carry a very low risk of hypoglycemia (low blood sugar) when used alone, which is a major advantage for many patients. They are typically taken once a day, are weight-neutral, and have a mild side effect profile, often limited to common cold-like symptoms.
* Choosing the Right Option: The decision between these and other medications is a conversation between you and your healthcare provider. Your doctor will consider many factors, including your specific A1C targets, whether you have existing heart disease, heart failure, or kidney disease (which would make SGLT2 inhibitors a strong candidate), your weight goals, your risk of hypoglycemia, and your overall health profile. The good news is that with multiple options available, there’s a strong chance of finding a medication that effectively supports your health without unnecessary side effects. Often, these medications are added to Metformin therapy when additional blood sugar control is needed.
Advanced Options: GLP-1 Receptor Agonists & Insulin Therapy
Sometimes, despite lifestyle changes and initial oral medications, your body might need more robust support to manage Type 2 Diabetes effectively. This is where GLP-1 Receptor Agonists and, if necessary, insulin therapy come into play. These are powerful tools that can make a significant difference.
* GLP-1 Receptor Agonists (e.g., Semaglutide, Liraglutide): These medications are truly exciting for many people with Type 2 Diabetes, offering a comprehensive approach to blood sugar management. GLP-1 Receptor Agonists mimic the action of your body’s natural GLP-1 hormone, but in a more potent and longer-lasting way. This leads to several beneficial effects: they stimulate your pancreas to release more insulin only when blood sugar levels are elevated (reducing the risk of hypoglycemia); they suppress glucagon, a hormone that raises blood sugar; they slow down digestion, helping to prevent sharp blood sugar spikes after meals; and critically, they increase feelings of fullness, often leading to significant weight loss. While many are administered by injection (often once daily or weekly, using a convenient pen device), an oral form of semaglutide is also available. Beyond blood sugar and weight, many GLP-1 Receptor Agonists have demonstrated impressive cardiovascular benefits, reducing the risk of major adverse cardiac events in people with established heart disease. Potential side effects are mostly gastrointestinal, such as nausea, vomiting, or diarrhea, especially when starting the medication, but these often improve over time.
* Insulin Therapy: When Needed: For some individuals with Type 2 Diabetes, insulin therapy eventually becomes a necessary part of their treatment plan. It’s important to understand that needing insulin is not a sign of failure; it simply means that your pancreas, over time, is no longer producing enough insulin to meet your body’s needs. Type 2 Diabetes is a progressive condition, and the beta cells in the pancreas that make insulin can gradually wear out. When this happens, insulin therapy directly replaces the vital hormone your body isn’t producing, effectively lowering blood sugar and preventing the long-term complications associated with persistently high glucose levels, such as nerve damage, kidney disease, and eye problems. Embracing insulin therapy when recommended by your doctor is a crucial step in maintaining your health and quality of life.
* Types and Administration: Insulin isn’t a one-size-fits-all medication; it comes in various forms designed to meet different needs. Basal (long-acting or intermediate-acting) insulins provide a steady background level of insulin throughout the day and night. Bolus (rapid-acting or short-acting) insulins are taken with meals to cover the carbohydrate intake and manage post-meal blood sugar spikes. There are also premixed insulins that combine both. Insulin can be administered through traditional syringes, convenient pre-filled pens, or even insulin pumps that deliver a continuous infusion of rapid-acting insulin. Learning about your specific insulin type, proper injection technique, and careful dosing based on blood sugar monitoring is key. Your healthcare team will provide thorough education and support to help you feel confident and comfortable with insulin therapy.
Other Considerations: Older Oral Medications
While newer medications often come with additional benefits, some older oral medications still play a role in Type 2 Diabetes management, especially when cost or specific patient profiles are key considerations. It’s helpful to understand the range of options available.
* Sulfonylureas (e.g., Glipizide, Glyburide): These medications have been around for a long time and are still commonly prescribed. They work by directly stimulating the beta cells in your pancreas to produce and release more insulin, regardless of your current blood sugar level. Their main advantage is their effectiveness in lowering A1C and their affordability, making them an accessible option for many. However, because they constantly stimulate insulin release, they carry a higher risk of hypoglycemia (low blood sugar) compared to some newer drugs, especially if meals are skipped or delayed. They can also lead to modest weight gain. For these reasons, while still effective, they are often used with caution or as a second or third-line option, especially if a patient is prone to hypoglycemia or weight gain.
* Thiazolidinediones (TZDs) (e.g., Pioglitazone): TZDs, like pioglitazone, primarily work by improving insulin sensitivity in your body’s muscle, fat, and liver cells. They make your cells more receptive to the insulin that your body already produces, allowing glucose to be taken up more efficiently from the bloodstream. This leads to lower blood sugar levels. TZDs are known for their durable A1C lowering effects and may have some potential cardiovascular benefits (pioglitazone, specifically). However, they come with certain considerations. They can cause fluid retention, leading to edema (swelling) and making them unsuitable for individuals with heart failure. They may also cause weight gain and have been associated with an increased risk of bone fractures, particularly in post-menopausal women. Rarely, pioglitazone has been linked to a very slight increase in the risk of bladder cancer. Due to these potential side effects, careful patient selection is crucial for TZD therapy.
* Alpha-Glucosidase Inhibitors (e.g., Acarbose): These medications take a different approach to blood sugar control. Alpha-glucosidase inhibitors work in your digestive tract, specifically in the small intestine, to slow down the digestion and absorption of carbohydrates. By doing so, they help to reduce the sharp rise in blood sugar levels that often occurs immediately after meals. They are primarily focused on managing post-meal glucose spikes and have a modest impact on overall A1C. A significant advantage is that they do not cause hypoglycemia when used alone, as they don’t directly stimulate insulin release. However, their primary downside is a high incidence of gastrointestinal side effects, such as flatulence, bloating, and diarrhea, because undigested carbohydrates ferment in the colon. These side effects can be significant enough to impact patient adherence, making them a less common choice in many clinical settings today.
Crafting Your Personalized Treatment Plan
Understanding the various medications is one thing, but figuring out your best plan is a truly individualized journey. Diabetes management is never a “set it and forget it” situation; it’s a dynamic process that requires close collaboration with your healthcare team.
* Factors Influencing Choice: When your doctor helps you craft your treatment plan, they take into account a multitude of factors, creating a truly bespoke approach. They’ll consider your age and the duration of your diabetes, your overall A1C target, and perhaps most importantly, any existing health conditions you may have, such as heart disease, heart failure, or kidney disease. These comorbidities often guide the selection towards medications with specific protective benefits, like SGLT2 inhibitors or GLP-1 receptor agonists. Other crucial considerations include your risk of hypoglycemia, your weight goals, any other medications you’re currently taking (to avoid adverse drug interactions), your kidney and liver function, and even your personal preferences, comfort with injections, and, of course, the cost and accessibility of medications. This comprehensive assessment ensures the plan is perfectly suited to you.
* Dynamic Treatment: It’s essential to remember that diabetes is often a progressive condition, meaning your treatment plan isn’t static. What works perfectly today might need adjustment six months or a year down the line as your body changes or as the disease naturally evolves. Your pancreas might produce less insulin over time, or your insulin resistance might worsen. This doesn’t mean you’re doing anything wrong; it’s just the nature of Type 2 Diabetes. Furthermore, the field of diabetes treatment is constantly advancing, with new research, medications, and technologies emerging regularly. This dynamic nature means your doctor will continually evaluate your progress and be prepared to modify your regimen to ensure you’re always receiving the most effective care possible.
* Regular Monitoring and Adjustments: Consistent and vigilant monitoring is the cornerstone of effective diabetes management. This includes regular self-monitoring of blood glucose levels at home, which provides immediate feedback on how your body responds to food, exercise, and medication. Your doctor will also order periodic A1C tests (typically every three to six months) to get an overall picture of your average blood sugar control. Beyond glucose, regular checks of kidney function (e.g., eGFR, albuminuria), lipid profiles, and blood pressure are crucial to monitor for and prevent long-term complications. These ongoing assessments, combined with regular consultations with your physician, a registered dietitian, or a certified diabetes educator, allow for timely adjustments to your medication regimen, diet, and exercise plan, ensuring your treatment remains optimized for your best health outcomes. Your active engagement in this monitoring process is invaluable.
Managing Type 2 Diabetes effectively is undeniably a multi-faceted and highly personalized journey. There isn’t a singular “best” medicine that fits everyone, but rather an optimal, evolving combination of dedicated lifestyle interventions and pharmacological therapies meticulously tailored specifically for you. From the foundational importance of diet, exercise, and Metformin, through the cardiovascular and renal protective benefits of SGLT2 inhibitors and GLP-1 receptor agonists, to the precise glucose control offered by insulin therapy, the array of options is vast. It is absolutely crucial to work closely and openly with your healthcare provider to develop, diligently monitor, and flexibly adjust your treatment plan. This collaborative approach ensures you achieve the best possible outcomes for your long-term health and vibrant quality of life.
Frequently Asked Questions
What is considered the “best” initial medication for newly diagnosed Type 2 diabetes?
Metformin is almost universally recommended as the first-line medication for most individuals with newly diagnosed Type 2 diabetes, often alongside significant lifestyle changes. It works by decreasing glucose production by the liver and improving insulin sensitivity. Its effectiveness, low risk of hypoglycemia, and potential cardiovascular benefits make it a cornerstone of initial Type 2 diabetes treatment.
How do doctors choose the most effective medicine for Type 2 diabetes?
Doctors consider several factors when selecting the best medicine for Type 2 diabetes, including a patient’s A1C level, other health conditions (like heart disease or kidney issues), potential side effects, and cost. The goal is a personalized treatment plan that effectively manages blood glucose while minimizing risks and improving overall health. This comprehensive approach ensures the chosen medication aligns with the individual’s specific needs and health profile.
Are there non-insulin medications for Type 2 diabetes, and when are they prescribed?
Yes, there are many effective non-insulin medications for Type 2 diabetes, often prescribed when Metformin alone isn’t sufficient or isn’t tolerated. These include GLP-1 receptor agonists, SGLT2 inhibitors, DPP-4 inhibitors, and sulfonylureas, among others. These drug classes work through different mechanisms to lower blood sugar and can be particularly beneficial for patients with cardiovascular disease or kidney disease, offering additional protective benefits beyond glucose control.
Why might a doctor switch or add to my Type 2 diabetes medication, and what are the options?
A doctor might switch or add to your Type 2 diabetes medication if your blood sugar levels are no longer well-controlled by your current regimen, you experience intolerable side effects, or if new medical conditions develop that could benefit from a different drug class. Options often include adding a second oral agent, introducing a GLP-1 receptor agonist, or initiating insulin therapy to achieve optimal glucose management. This adjustment ensures your treatment plan remains effective as your condition evolves.
What are the newer and most effective drug classes for managing Type 2 diabetes, beyond Metformin?
Beyond Metformin, two drug classes have shown significant effectiveness and additional health benefits: GLP-1 receptor agonists and SGLT2 inhibitors. GLP-1s help lower blood sugar, promote weight loss, and have proven cardiovascular benefits, while SGLT2 inhibitors not only reduce blood sugar but also offer protection for the heart and kidneys. These newer medications are increasingly recommended for patients with existing cardiovascular or kidney disease due to their profound organ-protective effects.
References
- https://www.niddk.nih.gov/health-information/diabetes/overview/managing-diabetes/medications
- https://www.cdc.gov/diabetes/managing/medications.html
- https://diabetes.org/health-wellness/medication
- https://diabetesjournals.org/care/article/47/Supplement_1/S168/153966/Pharmacologic-Approaches-to-Glycemic-Treatment
- Type 2 diabetes – Diagnosis and treatment – Mayo Clinic
- https://www.nejm.org/doi/full/10.1056/NEJMcp2203923
- https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)00153-5/fulltext
- https://en.wikipedia.org/wiki/Type_2_diabetes_mellitus_treatment_and_management