There isn’t a single “best” type 2 diabetes medication; the most effective treatment is highly individualized, depending on factors like your specific health profile, existing conditions, potential side effects, and treatment goals. The optimal approach is always determined in close consultation with your healthcare provider. This guide will explore the major classes of medications used to manage type 2 diabetes, helping you understand their mechanisms, benefits, and key considerations, so you can have a more informed discussion with your doctor.
Initial & Foundational Therapies

Before diving into specific medications, it’s crucial to understand the bedrock of type 2 diabetes management. These initial steps are fundamental and often enhance the effectiveness of any medication you might take.
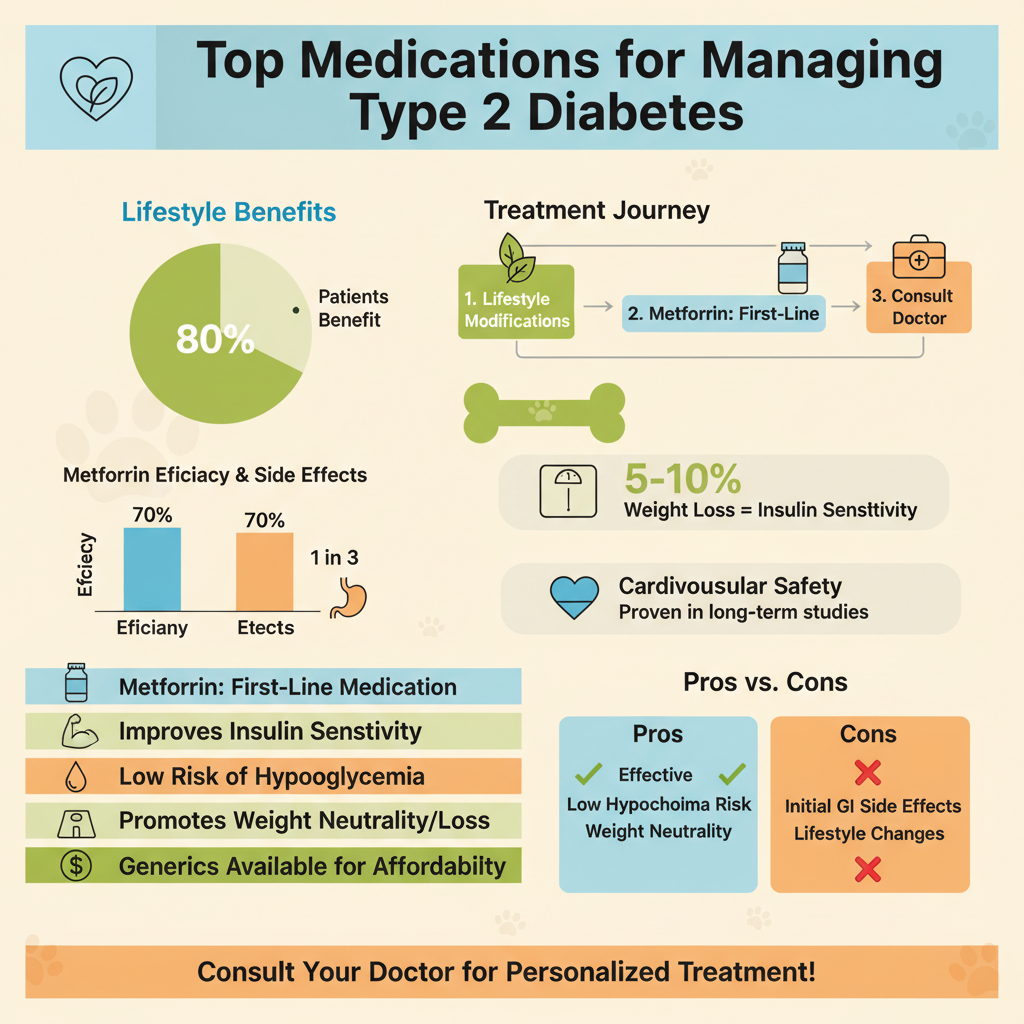
* Lifestyle Modifications: This isn’t just a suggestion; it’s the absolute cornerstone of all type 2 diabetes treatment. Making positive changes to your diet, engaging in regular physical activity, and managing your weight are incredibly powerful tools. A balanced diet, often emphasizing whole foods, lean proteins, and healthy fats, can significantly impact blood sugar levels. Even moderate weight loss (5-10% of body weight) can dramatically improve insulin sensitivity and reduce A1c levels. Regular exercise, whether it’s brisk walking, swimming, or strength training, helps your cells use glucose more efficiently and contributes to overall well-being. These changes lay the groundwork for success, often reducing the need for higher doses or multiple medications.
* Metformin: Often the first-line medication prescribed for type 2 diabetes, metformin has stood the test of time for its efficacy and safety profile. It primarily works by reducing the amount of glucose your liver produces (hepatic glucose output) and improving how effectively your body’s cells respond to insulin (insulin sensitivity), particularly in muscle and fat tissue. Unlike some other medications, metformin doesn’t stimulate the pancreas to produce more insulin, which helps reduce the risk of low blood sugar (hypoglycemia). It’s typically started at a low dose and gradually increased to minimize potential gastrointestinal side effects like nausea or diarrhea, which usually subside over time.
* Benefits of Metformin: The reasons metformin is so widely used are clear. It’s highly effective at lowering blood sugar and A1c levels. It carries a generally low risk of hypoglycemia, making it a safe option for many. Patients often experience modest weight loss or at least weight neutrality, which is a significant advantage compared to some other diabetes medications. Furthermore, long-term studies have shown metformin to have proven cardiovascular safety, meaning it doesn’t increase the risk of heart problems and may even offer some protective benefits. It’s also widely available as a generic, making it a cost-effective choice.
Oral Medications for Blood Sugar Control

Once lifestyle modifications and metformin are in place, your doctor might consider adding other oral medications to help you reach your blood sugar targets. Each class works differently to tackle various aspects of glucose control.
* Sulfonylureas & Meglitinides: These older classes of drugs work similarly by stimulating your pancreas to produce and release more insulin, which then rapidly lowers blood sugar. Sulfonylureas (like glipizide, glyburide, glimepiride) are often taken once or twice daily, while meglitinides (like repaglinide, nateglinide) are shorter-acting and typically taken just before meals. While effective, their main drawback is the increased risk of hypoglycemia because they continuously prompt insulin release regardless of your current blood sugar level. They can also lead to modest weight gain. For these reasons, they are often used with caution or when other options aren’t suitable.
* DPP-4 Inhibitors: These medications, such as sitagliptin (Januvia) or linagliptin (Tradjenta), work in a more sophisticated way by enhancing the body’s natural incretin hormones. Incretins are released after you eat and help regulate blood sugar by boosting insulin release and reducing glucagon (a hormone that raises blood sugar). DPP-4 inhibitors block an enzyme that breaks down these incretins, allowing them to stay active longer. The beauty of these drugs is their glucose-dependent action: they only enhance insulin release when blood sugar levels are high, significantly lowering the risk of hypoglycemia. They are generally weight-neutral and well-tolerated, making them a good option for many.
* Thiazolidinediones (TZDs): Drugs like pioglitazone (Actos) are often called “insulin sensitizers” because they improve insulin sensitivity in muscle and fat tissue. They achieve this by acting on specific receptors in your cells (PPAR-gamma receptors), allowing your body to use its own insulin more effectively. TZDs work more slowly than some other drugs, taking weeks to show their full effect, but they offer durable A1c lowering. However, their use requires careful monitoring due to potential side effects, including fluid retention, which can lead to swelling and, in some cases, worsen heart failure. They may also cause weight gain and have been associated with an increased risk of bone fractures. Your doctor will weigh these risks carefully against the benefits for your specific situation.
Injectable Non-Insulin Options

For many people with type 2 diabetes, oral medications alone might not be enough. Fortunately, there are highly effective injectable non-insulin options that can significantly improve blood sugar control and offer additional health benefits.
* GLP-1 Receptor Agonists (GLP-1 RAs): This class of medications (like liraglutide, semaglutide, dulaglutide) has revolutionized type 2 diabetes treatment. They mimic a natural hormone called glucagon-like peptide-1 (GLP-1) that the body releases after eating. GLP-1 RAs work on multiple fronts: they stimulate glucose-dependent insulin release from the pancreas, suppress glucagon secretion (which prevents the liver from releasing too much glucose), slow down gastric emptying (making you feel fuller longer), and act on the brain to reduce appetite.
* Key Benefits: The benefits of GLP-1 RAs are quite impressive. They lead to significant A1c reduction, often more substantial than many oral medications. A major plus for many patients is that they frequently lead to weight loss, which is incredibly helpful in managing type 2 diabetes. Perhaps most importantly, several GLP-1 RAs have demonstrated robust cardiovascular and renal protective effects, reducing the risk of heart attack, stroke, and kidney disease progression, making them a preferred choice for individuals with existing heart or kidney issues.
* Administration: GLP-1 RAs are administered via daily or weekly injections, typically using a pre-filled pen device, which is usually simple and less intimidating than it sounds. Common initial side effects include nausea, vomiting, or diarrhea, but these often improve over time as your body adjusts.
Medications Offering Heart & Kidney Protection
For individuals with type 2 diabetes, managing blood sugar is just one piece of the puzzle. Preventing cardiovascular disease (CVD) and kidney disease is equally critical, and some medications offer powerful protection beyond just glucose control.
* SGLT2 Inhibitors: These drugs, such as empagliflozin (Jardiance), canagliflozin (Invokana), and dapagliflozin (Farxiga), work in a unique way. They cause the kidneys to remove more glucose from the body through urine by blocking a protein called sodium-glucose co-transporter 2 (SGLT2). This process leads to lower blood glucose levels and also promotes a mild diuretic effect.
* Dual Benefits: Beyond their excellent blood sugar lowering capabilities, SGLT2 inhibitors have emerged as powerhouse medications for their impressive dual benefits. They significantly reduce the risk of major cardiovascular events (like heart attack and stroke) and, notably, reduce hospitalizations for heart failure, even in people without diabetes but with heart failure. Furthermore, they have shown remarkable ability to slow the progression of kidney disease and reduce the risk of kidney failure, making them invaluable for patients with or at risk of kidney complications.
* GLP-1 RAs (revisited): As mentioned earlier, many GLP-1 RAs also offer substantial benefits for cardiovascular health, reducing the risk of heart attack, stroke, and cardiovascular death. Similar to SGLT2 inhibitors, some GLP-1 RAs have also shown protective effects against kidney decline. For patients with established cardiovascular disease, heart failure, or chronic kidney disease, SGLT2 inhibitors and specific GLP-1 RAs are often prioritized in treatment plans, regardless of their A1c target.
When Insulin Therapy is Considered
Despite the array of oral and injectable non-insulin medications available, sometimes insulin therapy becomes a necessary and highly effective tool in managing type 2 diabetes. It’s important to view insulin not as a failure, but as a powerful, life-saving medication.
* Purpose: Insulin replaces or supplements the body’s own insulin when the pancreas is no longer able to produce enough or when other medications are insufficient to maintain healthy blood sugar levels. In type 2 diabetes, the pancreas’s ability to produce insulin gradually declines over time, and cells become more resistant to the insulin that is produced. Insulin therapy directly addresses this deficit, helping to lower blood sugar, prevent complications, and alleviate symptoms.
* Types of Insulin: Insulin comes in various forms, each designed to meet different needs. Long-acting (basal) insulin (e.g., glargine, detemir, degludec) provides a steady, continuous supply of insulin throughout the day and night, helping to control fasting and background blood sugar levels. Rapid-acting (bolus) insulin (e.g., aspart, lispro, glulisine) is typically taken before meals to cover the carbohydrate intake and manage post-meal blood sugar spikes. There are also pre-mixed options that combine rapid and intermediate-acting insulins, offering convenience but less flexibility. Your doctor will determine the best type and regimen for you.
* Decision Factors: Insulin may be initiated if A1c targets are not met despite optimized doses of other therapies. It’s often started when blood sugar levels are very high, accompanied by symptoms like excessive thirst, frequent urination, or unexplained weight loss. Insulin may also be temporarily or permanently used during acute illness, surgery, or pregnancy, when blood sugar control becomes more challenging. For individuals with significant kidney impairment, insulin often becomes a primary option as many other medications need dose adjustments or are contraindicated.
Personalizing Your Treatment: Key Considerations
Choosing the “best” medication is a collaborative process between you and your healthcare provider. It’s a personalized journey where many factors are carefully weighed to create the most effective and safest plan for you.
* Individual Health Profile: Your unique health situation is paramount. Your specific A1c target, for instance, might be tighter if you’re newly diagnosed and otherwise healthy, or more relaxed if you’re an older adult with multiple health conditions. Your kidney function, assessed by eGFR levels, heavily influences which medications are safe and effective, as many are cleared by the kidneys. The presence of existing heart disease (like a history of heart attack or stroke) or heart failure will often steer treatment towards medications with proven cardiovascular benefits, such as SGLT2 inhibitors or GLP-1 RAs. Similarly, if you have liver disease or a history of pancreatitis, certain medications might be avoided.
* Side Effects & Tolerability: Each medication class has potential side effects, and your body’s response is unique. Metformin’s common gastrointestinal upset, the risk of hypoglycemia with sulfonylureas, fluid retention with TZDs, or nausea with GLP-1 RAs are all factors to consider. Your doctor will discuss these potential side effects and strategies to manage them (e.g., slow dose titration, taking medication with food). Your ability to tolerate a medication is crucial for long-term adherence and success. Don’t hesitate to voice any concerns or uncomfortable symptoms you experience.
* Patient Preferences: Your preferences play a significant role in making a treatment plan sustainable. Cost is a major factor, as brand-name medications can be expensive, and insurance coverage varies. The administration route (oral pills versus daily or weekly injections) can impact your comfort level and willingness to adhere. The impact on weight is also important; some medications promote weight loss (GLP-1 RAs, SGLT2 inhibitors), while others can lead to weight gain (sulfonylureas, insulin, TZDs). Your lifestyle, including your meal schedule, travel habits, and ability to monitor blood sugars, will all factor into selecting a regimen that seamlessly fits into your daily life.
Navigating the various type 2 diabetes medications can feel complex, but remember that the “best” treatment is the one that works most effectively and safely for you. It’s a highly personalized journey that involves careful consideration of your health status, lifestyle, and treatment goals. Always have an open and honest discussion with your healthcare provider about all your options, potential side effects, and how each medication fits into your overall diabetes management plan. Regular follow-ups and blood sugar monitoring are essential to ensure your treatment remains optimized over time, helping you live a healthier, fuller life with diabetes.
Frequently Asked Questions
How do doctors choose the most effective type 2 diabetes medication for an individual?
Selecting the best type 2 diabetes medication is a personalized process based on several factors, including the patient’s A1c level, co-existing health conditions like heart disease or kidney issues, potential side effects, and cost. Healthcare providers consider a patient’s overall health profile, their ability to adhere to a medication regimen, and the drug’s specific benefits beyond glucose lowering, such as cardiovascular protection. The goal is to find a treatment plan that effectively manages blood sugar while minimizing risks and improving overall quality of life.
What are the different classes of type 2 diabetes medications and how do they help manage blood sugar?
Type 2 diabetes medications fall into several classes, each working differently to lower blood sugar. Metformin, often a first-line treatment, reduces glucose production by the liver and improves insulin sensitivity. Other classes include GLP-1 receptor agonists and SGLT2 inhibitors, which not only lower glucose but often provide cardiovascular and renal benefits. DPP-4 inhibitors, sulfonylureas, and thiazolidinediones (TZDs) also help by increasing insulin production or improving insulin utilization.
What are common side effects associated with type 2 diabetes medications, and how can they be managed?
Common side effects of type 2 diabetes medications vary by class but can include gastrointestinal issues like nausea, diarrhea (especially with metformin), or constipation. Some medications, such as sulfonylureas, carry a risk of hypoglycemia (low blood sugar), while SGLT2 inhibitors may increase the risk of urinary tract infections. Management often involves adjusting dosages, taking medication with food, or exploring alternative medications, with your doctor providing guidance on symptom relief and risk mitigation. Open communication with your healthcare provider is crucial to address any concerns.
Which newer type 2 diabetes medications offer benefits beyond just lowering blood sugar?
Newer type 2 diabetes medications like GLP-1 receptor agonists (e.g., Ozempic, Trulicity) and SGLT2 inhibitors (e.g., Jardiance, Farxiga) provide significant benefits beyond glycemic control. These drugs have demonstrated proven cardiovascular and kidney protection, reducing the risk of heart attacks, strokes, and progression of kidney disease in many patients. This makes them particularly valuable for individuals with type 2 diabetes who also have cardiovascular disease or chronic kidney disease.
Why might insulin be prescribed for type 2 diabetes, even when other medications are being used?
Insulin therapy is often initiated in type 2 diabetes when oral medications or other injectable drugs are no longer sufficient to achieve target blood sugar levels. This can occur as the disease progresses and the pancreas’s ability to produce insulin naturally declines over time. In some cases, insulin may be temporarily prescribed during illness, surgery, or pregnancy, or to quickly bring very high blood sugar under control before transitioning to other treatments. It’s a crucial tool to protect organs from damage due to chronic hyperglycemia.
References
- https://diabetesjournals.org/care/issue/47/Supplement_1/S1
- https://www.niddk.nih.gov/health-information/diabetes/overview/medications-treatments-type-2-diabetes
- https://www.cdc.gov/diabetes/managing/medication.html
- Diabetes treatment: Using insulin to manage blood sugar – Mayo Clinic
- https://en.wikipedia.org/wiki/Management_of_diabetes_mellitus_type_2
- https://www.who.int/publications/i/item/who-guideline-for-the-pharmacological-treatment-of-diabetes
- https://medlineplus.gov/diabetestype2medicines.html