There isn’t a single “best” medication for type 2 diabetes; rather, the most effective treatment plan is highly individualized, based on factors like your A1C levels, presence of comorbidities (like heart or kidney disease), potential side effects, and personal preferences. However, Metformin is almost always the first-line medication, often followed by newer classes like GLP-1 receptor agonists and SGLT2 inhibitors, which offer significant benefits beyond just blood sugar control. This guide will explore the primary medication options available to help you understand their roles in managing type 2 diabetes.
Understanding Type 2 Diabetes Medication Goals

Living with type 2 diabetes means actively managing your health to prevent complications and maintain a great quality of life. Medications play a crucial role in this journey, working towards several key objectives.
* Primary Goal: At the top of the list is lowering your blood glucose (sugar) levels, specifically your A1C. Your A1C provides an average picture of your blood sugar over the past two to three months. Keeping this number in a healthy range is paramount because consistently high blood sugar can silently damage various organs over time. This damage can lead to serious long-term complications like nerve damage (neuropathy), kidney disease (nephropathy), vision loss, heart attacks, and strokes. Medications are designed to help you reach and maintain your target A1C, significantly delaying or even preventing these challenging health issues.
* Secondary Goals: Beyond just blood sugar control, many modern diabetes medications offer exciting additional benefits. These include protecting vital organs such as your heart and kidneys, which are often at higher risk for complications in people with diabetes. Some medications can also help with weight management, which is a significant factor in type 2 diabetes, and improve your overall quality of life by reducing symptoms like fatigue or excessive thirst. These multi-faceted benefits are a real game-changer in diabetes care!
* Foundational Role: It’s super important to remember that medication is never a standalone solution. For optimal results, it works best in conjunction with consistent lifestyle modifications. This means adopting a balanced, diabetes-friendly diet, incorporating regular physical activity into your routine, and maintaining a healthy weight. Think of medications as powerful tools that amplify the positive effects of your healthy habits, creating a robust and comprehensive approach to managing your type 2 diabetes effectively.
First-Line Therapy: Metformin

If you’ve been diagnosed with type 2 diabetes, chances are high that Metformin will be one of the first medications your doctor discusses with you. It’s a true workhorse in diabetes management, and for good reason!
* Mechanism of Action: Metformin primarily works in two clever ways. First, it tells your liver to reduce the amount of glucose it produces. Our livers naturally make sugar, but in type 2 diabetes, they can sometimes make too much. By curbing this production, Metformin helps keep your blood sugar levels steadier. Secondly, it helps your body become more sensitive to insulin. In type 2 diabetes, your cells often resist the insulin your body makes, making it harder for sugar to get from your blood into your cells where it’s needed for energy. Metformin helps your cells “listen” to insulin better, allowing glucose to be utilized more efficiently.
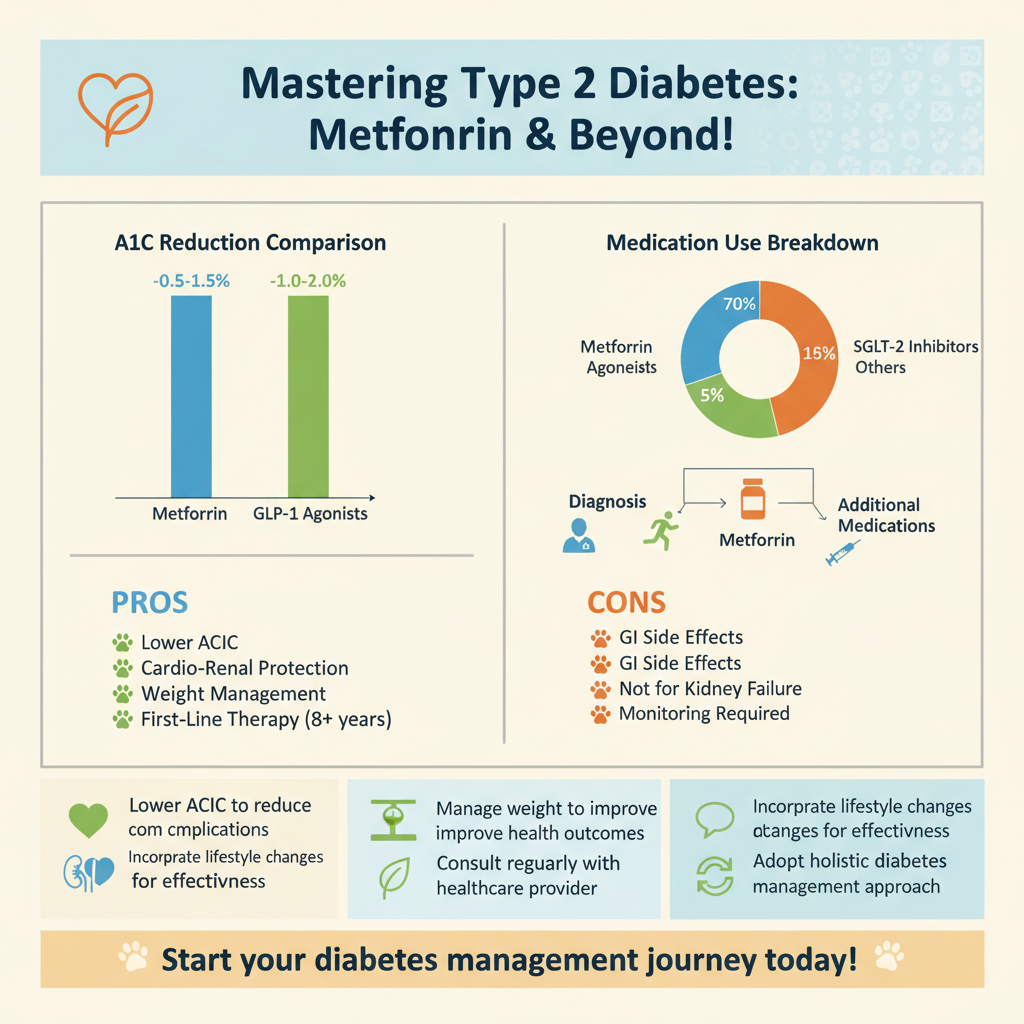
* Key Benefits: Metformin boasts an impressive list of advantages. It’s highly effective at lowering A1C levels, making it a cornerstone of treatment for most individuals. It’s also incredibly affordable and widely available, making it accessible to a vast number of people. Many individuals also experience a modest amount of weight loss when taking Metformin, which can be a welcome bonus given the strong link between weight and type 2 diabetes. Its long track record of safety and efficacy solidifies its position as the go-to initial treatment.
* Common Side Effects: While generally well-tolerated, Metformin can cause some gastrointestinal issues when you first start taking it. These might include nausea, diarrhea, stomach upset, or gas. The good news is that these side effects are usually mild and often subside as your body adjusts to the medication. Your doctor will typically start you on a low dose and gradually increase it, which helps minimize these initial digestive complaints. Taking Metformin with food can also be a helpful strategy to reduce stomach upset.
Modern Injectable Options: GLP-1 Receptor Agonists

Beyond oral medications, a class of modern injectable drugs has revolutionized diabetes treatment, offering impressive benefits that extend beyond simple blood sugar control. These are the GLP-1 receptor agonists.
* Examples: You might recognize some popular brand names like Semaglutide (available as Ozempic for injection or Rybelsus for oral use), Dulaglutide (Trulicity), and Liraglutide (Victoza). These medications have garnered significant attention for their powerful effects.
* Benefits: GLP-1 receptor agonists are real superstars when it comes to diabetes management. They significantly lower A1C by mimicking a natural hormone called GLP-1, which helps your pancreas release more insulin when blood sugar is high and reduces glucose production from the liver. One of their most celebrated benefits is promoting substantial weight loss. They do this by slowing down the emptying of your stomach, which helps you feel fuller for longer, and by impacting appetite signals in the brain. But wait, there’s more! These medications also offer proven cardiovascular benefits, meaning they can actually reduce the risk of major cardiac events like heart attacks and strokes, making them incredibly valuable for protecting your heart health.
* Administration: While the idea of injections might sound daunting at first, these medications are typically administered via convenient daily or weekly injections, using very fine needles that are easy to use at home. The convenience of a weekly shot, for example, can be a huge advantage for many people. Plus, for those who prefer not to inject, an oral form of semaglutide (Rybelsus) is now available, offering a pill option with similar benefits.
Kidney and Heart Protective Pills: SGLT2 Inhibitors
Another groundbreaking class of oral medications, SGLT2 inhibitors, offers fantastic benefits, particularly for protecting your kidneys and heart, which are often vulnerable to the long-term effects of type 2 diabetes.
* Examples: You might encounter medications like Empagliflozin (Jardiance), Dapagliflozin (Farxiga), and Canagliflozin (Invokana). These brand names have become increasingly well-known due to their impressive and broad-reaching health advantages.
* Mechanism of Action: SGLT2 inhibitors work in a very unique way that’s different from most other diabetes medications. They target your kidneys. Normally, your kidneys filter glucose out of your blood but then reabsorb most of it back into your bloodstream. SGLT2 inhibitors block this reabsorption process. This means that instead of keeping the sugar, your kidneys excrete more glucose in your urine, effectively “peeing out” excess sugar. This mechanism directly lowers your blood sugar levels.
* Key Benefits: The advantages of SGLT2 inhibitors are truly remarkable. Not only do they achieve excellent A1C reduction by removing glucose from your body, but they also provide significant protection for your cardiovascular system and kidneys. For people with type 2 diabetes, reducing the risk of heart failure, heart attacks, and slowing the progression of kidney disease is incredibly important, and these drugs have demonstrated these protective effects in clinical trials. As an added bonus, many individuals also experience some modest weight loss and a reduction in blood pressure when taking SGLT2 inhibitors, contributing to overall better health.
Other Common Oral Medications
While Metformin, GLP-1 receptor agonists, and SGLT2 inhibitors often take center stage in initial and evolving treatment plans, several other oral medications play important roles in managing type 2 diabetes, each with its own benefits and considerations.
* DPP-4 Inhibitors (e.g., Sitagliptin/Januvia): These medications, such as Sitagliptin (Januvia) or Linagliptin (Tradjenta), work by preventing the breakdown of natural gut hormones (like GLP-1) that help your body produce more insulin when blood sugar is high and reduce glucose production. They offer moderate A1C reduction and are generally very well-tolerated, with a low risk of hypoglycemia (low blood sugar) because they only stimulate insulin release when blood sugar levels are elevated. Plus, they are weight-neutral, meaning they won’t cause weight gain. They can be a good option for those needing a gentle addition to their regimen.
* Sulfonylureas (e.g., Glipizide, Glyburide): These are older, more traditional medications like Glipizide (Glucotrol) and Glyburide (DiaBeta). They work by stimulating the beta cells in your pancreas to produce and release more insulin, regardless of your current blood sugar level. They are quite effective at lowering blood sugar and are very affordable. However, because they stimulate insulin release continuously, they carry a higher risk of hypoglycemia, especially if meals are skipped or delayed. They can also lead to weight gain, which is a consideration for many individuals.
* Thiazolidinediones (TZDs, e.g., Pioglitazone/Actos): Medications like Pioglitazone (Actos) fall into the TZD class. These drugs work by improving your body’s sensitivity to insulin, primarily in muscle and fat tissue. They help your cells better utilize the insulin your body produces, leading to lower blood sugar levels. TZDs are effective, particularly for individuals with significant insulin resistance. However, they can cause fluid retention, which might lead to weight gain and swelling, and are not suitable for people with certain heart conditions. Your doctor will carefully assess if a TZD is the right choice for you.
When Insulin Therapy Becomes Necessary
For many people with type 2 diabetes, oral medications and non-insulin injectables are highly effective. However, there are times when insulin therapy becomes a necessary and incredibly important part of the treatment plan. It’s crucial to understand that starting insulin is not a sign of failure, but rather a natural progression of the disease for some, or a strategic move to optimize health.
* Purpose: The primary purpose of insulin therapy in type 2 diabetes is to directly replace the insulin your body is no longer producing sufficiently, or to supplement your body’s own insulin to overcome significant insulin resistance. In type 2 diabetes, the pancreas’s ability to produce insulin can decline over time. When your body can’t make enough insulin or effectively use the insulin it does make, direct insulin administration becomes crucial to bring blood sugar levels back into a healthy range.
* Indications: Insulin is often introduced when oral medications and other injectable therapies are no longer sufficient to achieve your target A1C goals, despite maximum doses and consistent lifestyle efforts. It might also be needed during specific periods, such as times of significant physical stress, severe illness, surgery, or pregnancy, when blood sugar levels can be particularly challenging to control. In some cases, if your blood sugar is very high at diagnosis, your doctor might even start with insulin temporarily to quickly bring levels down before transitioning to other medications.
* Types: Modern insulin therapy offers a lot of flexibility to suit individual needs. Insulin is available in various forms, each with a different action profile. Long-acting (basal) insulins provide a steady background supply of insulin throughout the day or night, mimicking the body’s natural baseline production. Rapid-acting (mealtime or bolus) insulins are taken just before meals to cover the carbohydrate intake and prevent post-meal blood sugar spikes. There are also intermediate-acting and pre-mixed insulins, which combine different action profiles in one injection. Your healthcare provider will work with you to determine the best type and regimen based on your blood sugar patterns and lifestyle.
Personalizing Your Treatment Plan
Navigating the world of type 2 diabetes medications can feel like a complex puzzle, but the good news is that your healthcare team is there to help you put all the pieces together. The goal is always a highly personalized approach that fits you like a glove.
* Key Factors: When your doctor selects medications, they’ll consider a variety of crucial factors to craft the most effective and safest plan. Your current A1C level is a major starting point, as it indicates how aggressively your blood sugar needs to be lowered. Any existing heart or kidney conditions are incredibly important, as newer medications like GLP-1 receptor agonists and SGLT2 inhibitors offer specific protective benefits to these organs. Your weight goals will also play a role, as some medications promote weight loss while others can cause weight gain. Of course, potential side effects and your personal tolerance for them, as well as the cost and insurance coverage of the medications, are also vital considerations in making practical, sustainable choices.
* Combination Therapy: It’s very common, and often necessary, for people with type 2 diabetes to be on multiple medications. This isn’t a sign that one medication isn’t working; rather, it’s a strategic approach called combination therapy. Different medications work in different ways to lower blood sugar and protect your body. By combining them, doctors can leverage their unique mechanisms of action to achieve optimal blood sugar control, reduce side effects (by using lower doses of each), and provide comprehensive protection against long-term complications, especially to your heart and kidneys.
* Ongoing Evaluation: Your medication regimen for type 2 diabetes is not a “set it and forget it” situation. It’s a dynamic process that requires ongoing evaluation. Your body’s needs change over time, and your medication plan will need to evolve with you. Regular check-ups with your doctor are essential to monitor your progress, review your A1C, assess for any new health conditions, and discuss how you’re feeling on your current medications. Based on these evaluations, your treatment plan will be regularly reviewed and adjusted to ensure you’re always on the most appropriate and effective path for your unique health journey.
Navigating the various medications for type 2 diabetes can seem complex, but understanding the options is the first step toward effective management. While Metformin is typically the starting point, newer drugs like GLP-1 receptor agonists and SGLT2 inhibitors have emerged as powerful tools, particularly for their protective benefits to the heart and kidneys. Remember, the “best” medication regimen is one tailored specifically to you. Always consult with your healthcare provider to discuss your individual health profile, goals, and the most appropriate treatment plan for your type 2 diabetes.
Frequently Asked Questions
What are the primary types of oral medications used to manage type 2 diabetes?
The primary types of oral medications for type 2 diabetes include Metformin (often the first-line treatment), sulfonylureas, DPP-4 inhibitors, SGLT2 inhibitors, and thiazolidinediones. These *type 2 diabetes medications* work through different mechanisms, such as reducing glucose production by the liver, improving insulin sensitivity, stimulating insulin release, or increasing glucose excretion via urine. Your healthcare provider will select the *best oral medication* based on your individual health needs and other factors.
Which newer medications for type 2 diabetes offer additional cardiovascular and kidney benefits?
Newer classes of *type 2 diabetes medications*, specifically SGLT2 inhibitors (e.g., Jardiance, Farxiga) and GLP-1 receptor agonists (e.g., Ozempic, Trulicity, which are often injectable but belong to a class frequently discussed with oral therapies), have demonstrated significant benefits beyond just blood sugar control. These innovative *diabetes drugs* have been shown to reduce the risk of major adverse cardiovascular events like heart attack and stroke, slow the progression of kidney disease, and often lead to weight loss. This makes them particularly valuable *medications for type 2 diabetes* in patients with co-existing heart or kidney conditions.
How do doctors determine the best medication plan for an individual with type 2 diabetes?
Doctors personalize a *type 2 diabetes medication* plan by considering several factors, including the patient’s A1C level, the presence of comorbidities like heart or kidney disease, potential side effects of specific drugs, and cost. They also evaluate a patient’s lifestyle, personal preferences, and the specific goals of therapy, aiming to find the most effective and safest *diabetes treatment* that aligns with their overall health profile. This ensures an individualized approach to managing blood sugar and reducing long-term complications.
What are common side effects to be aware of when taking type 2 diabetes medications?
Side effects vary widely among *type 2 diabetes medications*. Metformin can cause gastrointestinal issues like nausea, diarrhea, or abdominal discomfort, especially when first starting. Sulfonylureas carry a risk of hypoglycemia (low blood sugar) and weight gain, while SGLT2 inhibitors may increase the risk of genitourinary infections. It’s crucial to openly discuss any side effects with your doctor, as they can often adjust dosages, switch medications, or provide strategies to manage these issues effectively, helping you adhere to the *best medications for type 2 diabetes* for your situation.
Is insulin therapy always necessary for type 2 diabetes, or can oral medications be sufficient long-term?
Insulin therapy is not always necessary for managing type 2 diabetes, especially in the early stages or for those who achieve good blood sugar control with *oral medications for type 2 diabetes* and consistent lifestyle changes. Many individuals can effectively manage their condition for years, or even decades, using a combination of oral drugs. However, as type 2 diabetes is a progressive disease, insulin may eventually become necessary to maintain target blood sugar levels when the pancreas’s ability to produce insulin significantly declines, even with maximum oral medication therapy.
References
- https://diabetesjournals.org/care/article/47/Supplement_1/S11/153920/10-Pharmacologic-Approaches-to-Glycemic-Treatment
- Type 2 diabetes – Diagnosis and treatment – Mayo Clinic
- https://www.niddk.nih.gov/health-information/diabetes/overview/type-2-diabetes/treatments
- https://www.cdc.gov/diabetes/managing/medication.html
- https://en.wikipedia.org/wiki/Type_2_diabetes_mellitus_management
- Treatment for type 2 diabetes – NHS
- https://my.clevelandclinic.org/health/diseases/21493-type-2-diabetes/management-and-treatment