When it comes to the “best” diabetes medication, there isn’t a single answer, as the most effective treatment is highly individualized. What works best for one person depends on their type of diabetes, overall health, lifestyle, other existing conditions, and specific treatment goals. This guide will explore the various categories of diabetes medications available today, helping you understand the choices and empowering you to have an informed discussion with your healthcare provider.
The Personalized Approach to Diabetes Treatment

Managing diabetes effectively is a journey that’s deeply personal, and your treatment plan should reflect that. There’s no magic bullet or universal “best” drug; instead, the optimal approach is a carefully constructed strategy tailored just for you.
* No “One-Size-Fits-All” Solution: Imagine diabetes care like a custom-made suit – it has to fit you perfectly. Your healthcare provider will consider a multitude of factors, including your specific diagnosis (whether it’s Type 1, Type 2, or gestational diabetes), the health of your kidneys and heart, your body weight, your personal risk of hypoglycemia (low blood sugar), and even practical considerations like medication cost and your personal preferences for administration (pill vs. injection). For instance, someone with pre-existing heart disease might benefit greatly from a medication known for its cardiovascular protective effects, while someone struggling with weight might prioritize a drug with weight-loss benefits.
* Collaborate with Your Healthcare Team: You’re the most important member of your diabetes care team! Your doctor, an endocrinologist (a hormone specialist), and a diabetes educator will work closely with you. They’ll assess your unique profile – taking into account your medical history, current health status, and lifestyle – to craft a medication regimen that’s designed to achieve the best possible outcomes for *you*. This collaborative approach ensures that the treatment plan is not only medically sound but also practical and sustainable for your daily life.
* Treatment Goals: While controlling blood sugar levels is a primary goal, modern diabetes management extends far beyond that. Your treatment goals often include preventing serious long-term complications like nerve damage (neuropathy), kidney disease (nephropathy), and eye problems (retinopathy). We also focus on managing weight, protecting your kidney and cardiovascular health, and ultimately, significantly improving your quality of life. It’s about not just living longer, but living better.
Oral Medications for Type 2 Diabetes
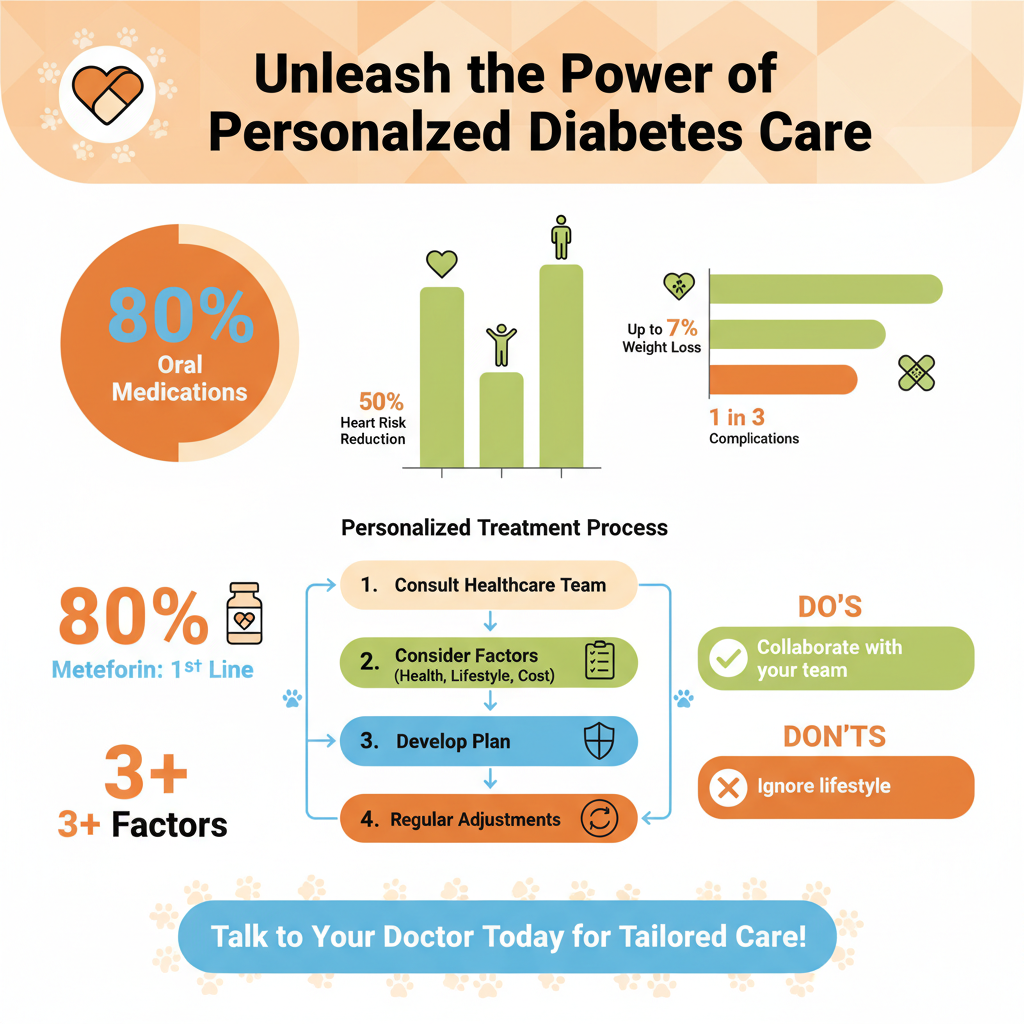

For many individuals with Type 2 diabetes, oral medications are the first line of defense, helping the body use insulin more effectively or reduce glucose production.
* Metformin (Biguanide): Often the star player in Type 2 diabetes treatment, Metformin is typically the first medication prescribed. It works primarily by reducing the amount of glucose your liver produces and by improving how sensitive your body’s cells are to insulin, helping them absorb sugar more efficiently. Beyond blood sugar control, Metformin has the added benefits of being weight-neutral (and sometimes even aids in modest weight loss) and offering some cardiovascular protection. While generally well-tolerated, some people may experience mild gastrointestinal side effects like nausea or diarrhea, which often improve over time or by taking the medication with food.
* Sulfonylureas & Meglitinides: These older but still effective classes of drugs, like glipizide or glyburide (Sulfonylureas), and repaglinide or nateglinide (Meglitinides), stimulate your pancreas to produce and release more insulin. This can lead to a rapid lowering of blood glucose levels. However, because they directly stimulate insulin release, they carry a higher risk of hypoglycemia (low blood sugar) and can sometimes contribute to weight gain. They are often used when blood sugar needs to be lowered quickly.
* DPP-4 Inhibitors (“Gliptins”): Drugs like sitagliptin (Januvia) or saxagliptin (Onglyza) are known as DPP-4 inhibitors. They work by enhancing the body’s natural incretin hormones (GLP-1 and GIP), which are released after meals. These hormones help stimulate insulin release when blood sugar is high and reduce glucose production by the liver. Gliptins are generally well-tolerated, have a low risk of hypoglycemia (especially when not combined with sulfonylureas), and are typically weight-neutral, making them a good option for many.
* SGLT2 Inhibitors (“Flozins”): This relatively newer class, including empagliflozin (Jardiance) and canagliflozin (Invokana), has been a game-changer. They work in your kidneys, causing them to excrete more glucose in your urine, thereby lowering blood sugar. What makes SGLT2 inhibitors particularly exciting are their significant benefits beyond glucose control: they have been shown to powerfully protect the heart in people with heart failure and reduce the progression of kidney disease, even in those without diabetes. They also typically lead to modest weight loss. Potential side effects can include an increased risk of urinary tract infections and yeast infections due to the sugar in the urine.
* Thiazolidinediones (TZDs): Medications like pioglitazone (Actos) improve insulin sensitivity in your muscle and fat cells, helping your body use insulin more effectively. They don’t stimulate insulin production directly, so the risk of hypoglycemia is low. While effective, TZDs may have side effects such as weight gain and fluid retention, and require careful monitoring in individuals with heart conditions. They can also offer some benefits for liver health.
Injectable Non-Insulin Medications

For some individuals with Type 2 diabetes, especially when oral medications aren’t enough, injectable non-insulin options offer powerful new avenues for treatment.
* GLP-1 Receptor Agonists (e.g., Ozempic, Trulicity): These powerful drugs, like semaglutide (Ozempic/Wegovy) and dulaglutide (Trulicity), are administered via injection (though some oral forms are now available, like Rybelsus). They mimic the natural GLP-1 hormone, which has multiple beneficial effects. GLP-1 agonists slow down gastric emptying, helping you feel fuller for longer, suppress appetite, and stimulate insulin release only when blood sugar levels are high (reducing hypoglycemia risk). They are celebrated for leading to significant weight loss and offering strong protective effects for both cardiovascular and kidney health, making them a cornerstone for many patients, especially those with obesity or related heart/kidney conditions. Common side effects can include nausea, vomiting, or diarrhea, particularly when starting treatment.
* Amylin Analogs (e.g., Symlin): Pramlintide (Symlin) is an injectable medication that is used alongside insulin, typically for both Type 1 and Type 2 diabetes. Amylin is a hormone co-secreted with insulin by the pancreas. Its analog helps slow down the absorption of food from the gut, reduces glucagon secretion (which prevents the liver from releasing too much glucose), and promotes a feeling of fullness (satiety). This can lead to better post-meal blood sugar control and, often, a reduction in the amount of insulin needed at mealtimes.
Insulin Therapy: Essential for Many
Insulin, discovered over a century ago, remains a lifesaving and critical medication for millions of people with diabetes.
* Lifesaving for Type 1 Diabetes: For individuals with Type 1 diabetes, insulin is not an option; it is an absolute necessity. In Type 1 diabetes, the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. Without external insulin, the body cannot process glucose, leading to dangerously high blood sugar levels that can be fatal. Insulin therapy in Type 1 diabetes is about replacing the insulin the body can no longer make, allowing glucose to enter cells for energy.
* For Advanced Type 2 Diabetes: While Type 2 diabetes initially involves insulin resistance, over time, the pancreas’s ability to produce insulin often declines. Many individuals with Type 2 diabetes will eventually require insulin as their pancreatic beta cells “burn out” or when oral medications and non-insulin injectables are no longer sufficient to maintain adequate blood sugar control. Starting insulin for Type 2 diabetes is not a sign of failure, but rather a natural progression of the disease and a necessary step to protect long-term health and prevent complications.
* Types of Insulin: Insulin comes in various forms, each designed to mimic the body’s natural insulin release patterns and cover different needs throughout the day:
* Rapid-acting insulin (e.g., Humalog, Novolog) works quickly (within 15 minutes) and is taken just before or with meals to cover the carbohydrate intake.
* Short-acting insulin (e.g., Novolin R, Humulin R) takes a bit longer to start working (30-60 minutes) and is also used to cover meals.
* Intermediate-acting insulin (e.g., Novolin N, Humulin N) has a delayed onset and lasts longer, often used once or twice daily.
* Long-acting insulin (e.g., Lantus, Levemir) provides a steady, basal (background) level of insulin for up to 24 hours, helping to control blood sugar between meals and overnight.
* Ultra-long-acting insulin (e.g., Tresiba) provides even longer and flatter basal coverage, sometimes lasting up to 42 hours.
Your doctor will help you determine the right combination and timing of insulin to create a regimen that fits your lifestyle and blood sugar patterns.
Emerging Therapies and Future Horizons
The field of diabetes treatment is constantly evolving, with exciting new medications offering even greater efficacy and broader benefits.
* Dual GIP/GLP-1 Receptor Agonists (e.g., Mounjaro): Representing the forefront of diabetes pharmacology, these newer injectables, like tirzepatide (Mounjaro), target not one, but two incretin hormones: glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1). By activating both receptors, they offer even greater efficacy in lowering blood sugar and inducing significant weight loss compared to single GLP-1 agonists. This dual action provides a more potent and comprehensive approach to managing Type 2 diabetes and its related metabolic challenges.
* Oral GLP-1 Receptor Agonists: While GLP-1 agonists have historically been injectable, the development of oral forms, such as semaglutide (Rybelsus), marks a significant step forward in accessibility and patient convenience. For many, the idea of a pill instead of an injection can improve adherence and make these powerful medications a more appealing option, offering similar benefits to their injectable counterparts in terms of blood sugar control and weight management.
* Focus on Multi-Organ Benefits: The future of diabetes medication is increasingly moving beyond just glycemic control. Researchers are developing and refining therapies that specifically aim to provide benefits for multiple organs, addressing the complex, systemic nature of diabetes. This includes medications that offer superior cardiovascular protection, reduce the risk and progression of kidney disease, and support significant weight loss. This holistic approach ensures that treatment plans are designed not just to lower blood sugar, but to improve overall health, prevent long-term complications, and enhance quality of life for individuals living with diabetes.
Beyond Medication: Lifestyle and Ongoing Management
While medications play a vital role, they are most effective when integrated into a comprehensive approach to diabetes care that prioritizes lifestyle and consistent monitoring.
* Foundation of Treatment: Regardless of the medications you’re taking, a healthy lifestyle remains the absolute cornerstone of diabetes care. This includes a balanced and consistent nutrition plan (often guided by a registered dietitian), regular physical activity (aiming for at least 150 minutes of moderate-intensity exercise per week), sufficient sleep, and effective stress management techniques. These lifestyle factors don’t just complement your medication; they enhance its effectiveness and can significantly impact your blood sugar levels, weight, and overall well-being. Think of medication as a powerful tool, but lifestyle as the engine that drives your health forward.
* Continuous Monitoring: Staying on top of your numbers is crucial to assess how well your treatment plan is working and to make necessary adjustments. This involves regular blood glucose monitoring, which can be done through finger-prick tests or continuous glucose monitors (CGMs). You’ll also have periodic A1c tests to measure your average blood sugar over two to three months, as well as regular checks of your kidney and liver function, cholesterol levels, and blood pressure. These tests help your healthcare team fine-tune your medications and lifestyle interventions, ensuring you’re always on the most effective path.
* Adherence and Education: The best medication in the world won’t work if it’s not taken as prescribed. Understanding your medication – why you’re taking it, how it works, and potential side effects – is key to successful long-term management. Engaging in ongoing diabetes education, whether through certified diabetes educators, support groups, or reliable online resources, empowers you to become an active and knowledgeable participant in your own care. This continuous learning helps you navigate the challenges of living with diabetes and make informed decisions about your health.
Choosing the best diabetes medication is a dynamic and deeply personal process that evolves over time. It requires open communication with your healthcare team to weigh the benefits, risks, and side effects of different options against your individual health profile and lifestyle. By understanding the broad spectrum of available treatments and committing to a holistic approach that includes lifestyle management and continuous monitoring, you can effectively manage your diabetes and significantly improve your long-term health and well-being. Always consult your doctor to determine the most suitable and effective treatment plan for you.
Frequently Asked Questions
Is there a single “best diabetes medication” for everyone?
No, there isn’t one universal “best diabetes medication” as treatment is highly individualized. The most effective medication depends on your specific type of diabetes (Type 1 or Type 2), overall health, other medical conditions, lifestyle, potential side effects, and your blood sugar targets. Your healthcare provider will conduct a thorough assessment to determine the optimal treatment plan for your unique needs, aiming for effective blood sugar control and improved quality of life.
What are the main types of medications used to manage Type 2 diabetes?
For Type 2 diabetes, common medication classes include Metformin (often a first-line therapy), GLP-1 receptor agonists, SGLT2 inhibitors, DPP-4 inhibitors, sulfonylureas, and thiazolidinediones. These medications work through various mechanisms, such as increasing insulin sensitivity, reducing glucose production by the liver, or promoting glucose excretion through urine. In some cases, insulin therapy may also be prescribed, either alone or in combination with other oral medications, to achieve optimal blood sugar management.
How do doctors determine which diabetes medication is right for me?
Your doctor considers several crucial factors when selecting the best diabetes medication for you. These include your current A1C level, kidney and heart health, weight management goals, risk of hypoglycemia (low blood sugar), and potential medication side effects. They will also discuss your lifestyle, preferences, and ability to adhere to a specific regimen to ensure the chosen treatment effectively supports your overall health and helps you manage diabetes long-term.
Which diabetes medications offer additional benefits like weight loss or cardiovascular protection?
Certain newer diabetes medications are increasingly recognized for benefits beyond just blood sugar control. GLP-1 receptor agonists (e.g., Ozempic, Trulicity) and SGLT2 inhibitors (e.g., Jardiance, Farxiga) have shown significant advantages, including promoting weight loss and reducing the risk of major cardiovascular events or kidney disease in many patients with Type 2 diabetes. These classes are often considered for individuals with existing heart or kidney conditions or those needing help with weight management.
Why is it important to understand the potential side effects of diabetes medications?
Understanding the potential side effects of your diabetes medication is crucial for managing your health effectively and safely. Knowing what to expect allows you to identify adverse reactions early, differentiate them from other symptoms, and discuss any concerns promptly with your doctor. This informed approach helps ensure medication adherence and allows your healthcare provider to adjust your treatment plan if side effects become problematic, ultimately leading to better and safer diabetes management.
References
- https://www.niddk.nih.gov/health-information/diabetes/overview/medications-treatments
- https://diabetes.org/health-wellness/medications
- https://www.cdc.gov/diabetes/managing/medications.html
- Diabetes treatment: Using insulin to manage blood sugar – Mayo Clinic
- Diabetes medication
- https://www.who.int/publications/i/item/9789240035510
- https://www.med.stanford.edu/news/all-news/2023/10/diabetes-management.html
- https://www.bbc.com/news/health-67123530


