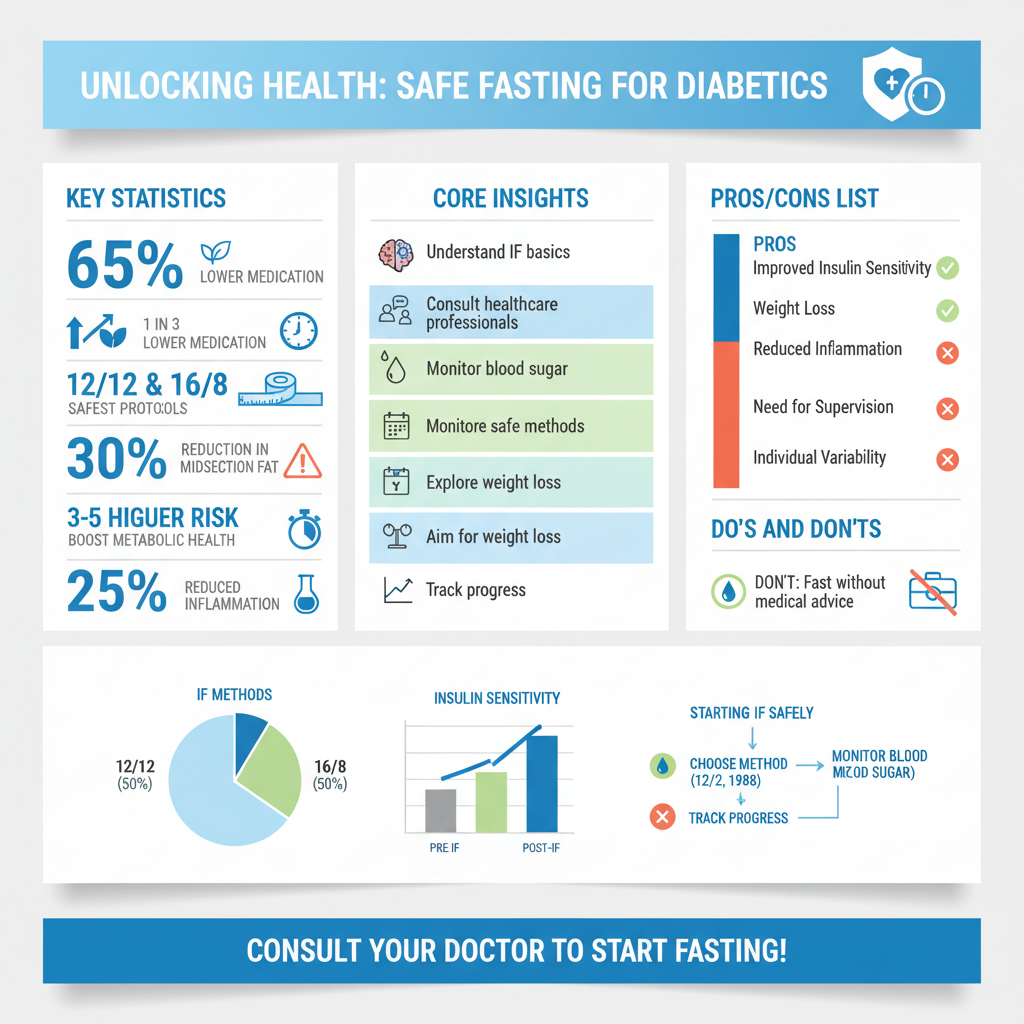
Navigating the world of intermittent fasting (IF) with diabetes requires careful consideration and, most importantly, medical guidance. While no single “best” method fits everyone, approaches like time-restricted eating (e.g., 12/12 or 14/10 methods) and the 16/8 protocol are generally considered safer and more manageable for individuals with diabetes, primarily due to their shorter fasting windows. These methods can potentially support improved insulin sensitivity and weight management, but they must always be implemented under the strict supervision of a healthcare professional to prevent dangerous fluctuations in blood sugar.
Understanding Intermittent Fasting and Diabetes

Intermittent fasting (IF) has gained significant attention in recent years for its potential health benefits, including weight management and metabolic improvements. For individuals living with diabetes, understanding what IF entails, its potential advantages, and its unique risks is paramount before considering any changes to their eating patterns.
* What Intermittent Fasting Entails: At its core, intermittent fasting isn’t a diet in the traditional sense, but rather an eating pattern that cycles between periods of eating and voluntary fasting. It shifts the focus from *what* you eat to *when* you eat. This can range from daily time-restricted eating, where you fast for a certain number of hours each day, to longer fasts performed less frequently. The goal is to allow your body to enter a metabolic state where it can burn stored fat for energy, a process called ketosis, and potentially improve cellular functions.
* Potential Benefits for Diabetics: When managed correctly under medical supervision, IF may offer several compelling benefits for individuals with Type 2 diabetes. One of the most significant potential advantages is improved insulin sensitivity. Fasting periods can give the pancreas a rest and help the body respond more effectively to insulin, potentially lowering blood sugar levels and reducing the need for medication over time. Additionally, IF often leads to weight loss, which is a key factor in managing and even reversing Type 2 diabetes. Reduced body fat, particularly around the midsection, can significantly enhance metabolic health. Furthermore, some research suggests that IF may reduce chronic inflammation, a common underlying factor in diabetes and its complications.
* Unique Risks for Diabetics: While the potential benefits are exciting, it’s crucial to acknowledge the unique and serious risks that intermittent fasting poses for individuals with diabetes. The primary concern is the potential for dangerous fluctuations in blood sugar. Fasting can lead to hypoglycemia (dangerously low blood sugar), especially for those on insulin or certain oral diabetes medications like sulfonylureas, which stimulate insulin production regardless of food intake. Symptoms of hypoglycemia can include dizziness, confusion, sweating, and even loss of consciousness. Conversely, if medication is improperly adjusted or if individuals overeat during their eating window, fasting can also lead to hyperglycemia (dangerously high blood sugar). For Type 1 diabetics, this risk is even higher, with potential for diabetic ketoacidosis (DKA), a life-threatening condition. These risks make medical supervision not just advisable, but absolutely crucial.
Safest Intermittent Fasting Methods for Diabetics

For individuals with diabetes, the emphasis should always be on safety and sustainability. While many IF protocols exist, some are significantly more suitable and less risky than others when managed carefully.
* Time-Restricted Eating (TRE): This is generally considered the most gentle and safest entry point for diabetics exploring IF. TRE involves limiting your eating to a specific window each day, usually between 8 to 12 hours, and fasting for the remaining hours.
* 12/12 Method: This involves a 12-hour eating window and a 12-hour fast. For example, if you finish dinner by 7 PM, you wouldn’t eat again until 7 AM the next morning. This method often aligns well with natural circadian rhythms and can be a very manageable starting point, as it typically involves simply skipping a late-night snack or pushing breakfast back slightly. It minimizes prolonged fasting risks, making it easier to manage blood sugar levels.
* 14/10 Method: Here, you fast for 14 hours and have a 10-hour eating window. For instance, if your last meal is at 7 PM, your first meal the next day would be at 9 AM. This is a slightly more extended fast than 12/12 but still relatively mild and less likely to cause drastic blood sugar drops compared to longer protocols. It allows for a good night’s sleep and often means simply pushing breakfast back an hour or two.
These TRE methods are often recommended as a gentle starting point because they minimize prolonged fasting risks, allowing for more frequent medication administration if needed, and make it easier to maintain stable blood glucose levels.
* The 16/8 Method: This is one of the most popular intermittent fasting protocols, involving fasting for 16 hours and eating all meals within an 8-hour window. A common example is finishing dinner by 8 PM and not eating again until 12 PM (noon) the next day, effectively skipping breakfast. While highly effective for many without diabetes, for individuals with diabetes, this approach requires closer monitoring and more careful medication adjustments. The longer fasting window means a greater potential for hypoglycemia, especially if medications aren’t perfectly calibrated. It’s an effective approach for metabolic benefits but should only be undertaken with very close medical supervision.
* Methods to Approach with Extreme Caution (or Avoid): Longer fasting protocols pose significant and often unacceptable risks for individuals with diabetes, particularly those on medication.
* 24-Hour Fasts (Eat-Stop-Eat): This involves fasting completely for 24 hours once or twice a week. The risk of severe hypoglycemia or hyperglycemia is dramatically increased, as blood sugar regulation becomes much harder over such an extended period without food.
* Alternate-Day Fasting (ADF): This involves fasting every other day, either completely or consuming a very small number of calories (e.g., 500 calories) on fasting days. This method is generally not recommended for individuals with diabetes due to the high risk of severe blood sugar dysregulation, electrolyte imbalances, and challenges in coordinating medication.
* Extended Fasts (e.g., 36-hour, 48-hour, or 5:2 diet with very low-calorie days): These methods significantly increase the risk of adverse events like severe hypoglycemia, dehydration, and electrolyte disturbances, and should almost always be avoided by individuals with diabetes. The potential benefits rarely outweigh the significant dangers.
The Absolute Necessity of Medical Supervision

For anyone with diabetes considering intermittent fasting, consulting a healthcare professional is not just a recommendation—it’s a non-negotiable prerequisite. The complexities of diabetes management, coupled with the potential impact of fasting on blood glucose, demand expert guidance.
* Personalized Medical Assessment: Before you even think about starting IF, a doctor or registered dietitian specializing in diabetes needs to conduct a thorough assessment of your individual health status. This includes reviewing your specific type of diabetes (Type 1 or Type 2), the severity of your condition, your current medication regimen, any co-existing health conditions (like kidney disease or heart issues), and your overall lifestyle. They can help determine if IF is appropriate and safe for *you*, or if it poses too many risks. A personalized approach is key, as what works for one person with diabetes might be dangerous for another.
* Medication Adjustments: This is perhaps the most critical aspect of medical supervision. Insulin and certain oral diabetes medications (like sulfonylureas or glinides) are designed to lower blood sugar in response to food intake. When you fast, your body isn’t receiving food, yet these medications might still be active, leading to a severe drop in blood sugar (hypoglycemia). Your doctor will need to carefully adjust your medication dosages and timing to align with your fasting schedule. This is an intricate process that *only* a qualified healthcare professional should manage. Attempting to adjust medications on your own can lead to life-threatening complications.
* Consistent Blood Glucose Monitoring: Frequent and diligent blood sugar testing is absolutely essential when practicing IF with diabetes. You’ll need to monitor your glucose levels before, during, and after your fasting periods, and especially when you break your fast. This continuous monitoring allows you and your healthcare team to identify any dangerous fluctuations promptly. Modern tools like continuous glucose monitors (CGMs) can be incredibly helpful, providing real-time data and alerting you to impending lows or highs. This data is vital for making informed decisions about medication adjustments, tweaking your eating window, and ensuring your safety throughout the process.
Optimizing Your Eating Window for Blood Sugar Control
While intermittent fasting focuses on when you eat, the quality of what you consume during your eating window is equally, if not more, important, especially for blood sugar management. Your food choices can make or break the effectiveness and safety of your IF protocol.
* Prioritize Nutrient-Dense Foods: When your eating window opens, it’s not a free-for-all. Focus on consuming whole, unprocessed foods that provide sustained energy and stable blood sugar.
* Lean Proteins: Include sources like chicken, turkey, fish, eggs, tofu, beans, and lentils. Protein helps with satiety, muscle maintenance, and has a minimal impact on blood sugar.
* Healthy Fats: Incorporate avocados, nuts, seeds (chia, flax), olive oil, and fatty fish (salmon). These fats contribute to fullness and slow down the absorption of carbohydrates, preventing rapid blood sugar spikes.
* Fiber-Rich Vegetables: Load up on non-starchy vegetables like leafy greens, broccoli, cauliflower, bell peppers, and asparagus. Fiber is crucial for digestive health, satiety, and slowing glucose absorption.
* Complex Carbohydrates: Choose whole grains like oats, quinoa, brown rice, and sweet potatoes in moderation. These provide sustained energy without the sharp blood sugar spikes associated with refined carbs.
* Maintain Stable Blood Sugar: To avoid the dreaded blood sugar roller coaster, be strategic about what you *don’t* eat.
* Avoid Sugary Drinks and Refined Carbohydrates: Steer clear of sodas, fruit juices, sweetened teas, white bread, pastries, sugary cereals, and pasta. These foods cause rapid and dramatic spikes in blood glucose, followed by crashes, which can counteract any benefits of fasting and lead to cravings and irritability.
* Limit Processed Foods: Highly processed snacks, fast food, and meals high in unhealthy fats and added sugars should be minimized. They offer little nutritional value and can negatively impact blood sugar and overall health.
* Balanced Meals: Aim for balanced meals that combine protein, healthy fats, fiber, and complex carbs to provide steady energy and prevent extreme blood sugar fluctuations throughout your eating window.
* Stay Hydrated: Hydration is key, both during your fasting and eating windows. Drink plenty of water, unsweetened tea, or black coffee. These beverages can help manage hunger pangs during fasting, prevent dehydration (which can sometimes mimic hunger), and support overall bodily functions. Avoid any caloric beverages during your fasting period, as they will break your fast. Proper hydration also supports kidney function, which is particularly important for individuals with diabetes.
Potential Benefits and Risks for Diabetics
Intermittent fasting, when approached with extreme caution and under expert medical guidance, holds a unique set of potential advantages and significant risks for individuals with diabetes. It’s crucial to weigh both sides carefully.
* Key Potential Benefits:
* Improved Insulin Sensitivity: By providing periods where the body isn’t constantly processing glucose, IF can give the pancreas a break and help cells become more responsive to insulin. This means your body might need less insulin to move glucose from the blood into cells, potentially lowering insulin resistance, a hallmark of Type 2 diabetes.
* Reduced HbA1c: Over time, improved insulin sensitivity and better blood sugar control can lead to a lower HbA1c (glycated hemoglobin) level, which is a key indicator of long-term blood sugar management. A lower HbA1c signifies better diabetes control and reduced risk of complications.
* Potential Weight Loss: IF naturally often leads to a reduction in overall calorie intake, which can result in weight loss. Shedding excess pounds, especially visceral fat around organs, is highly beneficial for individuals with Type 2 diabetes, often improving metabolic health and reducing the burden on the pancreas.
* Better Blood Pressure Control: Weight loss and improved insulin sensitivity can also contribute to better blood pressure regulation, reducing the risk of cardiovascular disease, a common comorbidity with diabetes.
* Significant Risks to Be Aware Of:
* Hypoglycemia: This is the most immediate and dangerous risk, especially for those on insulin or insulin-stimulating medications. Fasting without proper medication adjustment can cause blood sugar to drop to dangerously low levels, leading to confusion, dizziness, tremors, seizures, or even coma.
* Hyperglycemia: Conversely, if medications are reduced too much, or if individuals overeat high-carb foods during their eating window, blood sugar can soar. For Type 1 diabetics, this carries the risk of diabetic ketoacidosis (DKA), a life-threatening condition.
* Dehydration: Fasting can sometimes lead to reduced fluid intake, increasing the risk of dehydration, which can worsen fatigue and impact blood sugar levels.
* Electrolyte Imbalances: Prolonged fasting can disturb the balance of essential electrolytes like sodium, potassium, and magnesium, leading to symptoms like muscle weakness, heart palpitations, and severe fatigue.
* Nutrient Deficiencies: If not carefully managed, limiting eating windows could lead to an insufficient intake of essential vitamins and minerals, especially if food choices are not nutrient-dense.
* Exacerbation of Existing Health Conditions: IF can place additional stress on the body and could worsen conditions like kidney disease, liver disease, or heart conditions if not properly monitored.
* Warning Signs to Heed: It is imperative to know the warning signs that indicate you need to stop fasting immediately and seek medical attention. These include:
Dizziness, lightheadedness, or fainting
Extreme fatigue or weakness
Confusion or difficulty concentrating
Irritability or mood swings
Excessive thirst or frequent urination
Blurred vision
Nausea or vomiting
Rapid or irregular heartbeat
Any unusual or severe symptoms
Who Should Be Cautious (or Avoid) Intermittent Fasting
While intermittent fasting can be a powerful tool for some, it is decidedly not for everyone, especially within the diabetic community. Certain individuals face significantly higher risks and should approach IF with extreme caution, or avoid it altogether.
* Type 1 Diabetics: Generally, individuals with Type 1 diabetes are strongly advised against intermittent fasting. The absolute dependence on external insulin for survival makes managing blood glucose during fasting periods incredibly complex and risky. The potential for severe hypoglycemia is very high, and there’s also an elevated risk of diabetic ketoacidosis (DKA) due to fluctuating insulin needs and the body’s metabolic response to prolonged fasting. The intricate balance required makes IF a dangerous endeavor without constant, expert medical oversight, and even then, it’s often deemed too risky.
* Individuals on Specific Medications: Those taking medications that actively lower blood sugar levels face increased risks. This includes:
* Insulin: Any form of insulin therapy (basal, bolus, pre-mixed) directly impacts blood sugar, and fasting without precise, real-time adjustments by a doctor can lead to life-threatening hypoglycemia.
* Sulfonylureas (e.g., glipizide, glyburide, glimepiride): These oral medications stimulate the pancreas to produce more insulin, regardless of food intake. Fasting while on these drugs can cause severe and prolonged low blood sugar.
* Glinides (e.g., repaglinide, nateglinide): Similar to sulfonylureas, glinides also boost insulin production and carry a significant risk of hypoglycemia if taken during fasting periods.
Anyone taking high doses of any diabetes medication needs extremely close medical oversight if they consider IF.
* Other Contraindications: Several other health conditions or life stages make intermittent fasting unsuitable or dangerous:
* Pregnant or Breastfeeding Individuals: These periods require consistent and adequate nutrient intake to support both the mother and the developing baby or infant. Fasting can compromise nutrient delivery and is generally not recommended.
* Individuals with a History of Eating Disorders: IF can be a trigger for disordered eating patterns, body image issues, and relapse in those with a history of anorexia, bulimia, or binge eating disorder. The focus on restrictive eating windows can be psychologically damaging.
* Individuals with Severe Kidney or Liver Disease: Fasting can place additional metabolic stress on these vital organs, potentially exacerbating existing conditions.
* Those with Gout: Fasting can sometimes trigger gout attacks by increasing uric acid levels.
* Individuals with Adrenal Insufficiency: Fasting can strain the adrenal glands, which are already compromised in these individuals.
* Anyone who is underweight or malnourished, or has active infections or recent surgery should also avoid IF.
Implementing intermittent fasting for diabetes management is a highly personal journey that demands caution and expert medical guidance. By starting with gentler, time-restricted eating methods, prioritizing nutrient-rich foods during your eating window, and maintaining rigorous blood glucose monitoring under the watchful eye of your healthcare team, you can explore IF as a potential complementary strategy to improve your diabetes management safely and effectively. Remember, your health and safety are paramount, and no potential benefit is worth risking severe complications. Always consult your doctor before making any significant dietary changes.
Frequently Asked Questions
Which intermittent fasting schedule is safest and most effective for diabetics?
For diabetics, the safest and often most effective intermittent fasting schedules are typically less restrictive, such as time-restricted eating (TRE) windows like 12:12 or 14:10. These involve fasting for 12-14 hours and eating within a 10-12 hour window daily, which can help improve insulin sensitivity and glucose control without extreme blood sugar fluctuations. Always consult with a healthcare provider before starting, as individual responses to intermittent fasting for diabetics can vary significantly.
Is intermittent fasting safe for all types of diabetes, especially those on medication?
Intermittent fasting requires extreme caution and strict medical supervision for most diabetics, especially those on insulin or certain oral medications that increase insulin secretion, due to the high risk of hypoglycemia ( dangerously low blood sugar). It is generally not recommended for individuals with type 1 diabetes or those prone to ketoacidosis. For type 2 diabetics, a healthcare provider can assess suitability and safely adjust medication dosages to prevent complications.
How does intermittent fasting impact blood sugar levels and insulin sensitivity in people with diabetes?
Intermittent fasting can positively impact blood sugar levels and insulin sensitivity by reducing the frequency of glucose spikes throughout the day and extending periods where the body isn’t processing food. This allows the pancreas to rest and can lead to lower fasting blood glucose levels and improved insulin function over time. However, this metabolic shift must be carefully managed in diabetics to avoid adverse effects.
What are the crucial precautions diabetics should take before starting intermittent fasting?
Before attempting intermittent fasting, diabetics must first consult their doctor to review their current health status, diabetes type, and medication regimen. Essential precautions include carefully monitoring blood sugar levels multiple times a day, ensuring adequate hydration, and consuming nutrient-dense foods during eating windows to prevent deficiencies. A gradual approach, starting with shorter fasting periods, is also advisable under medical guidance.
Why is medical supervision essential for diabetics considering intermittent fasting?
Medical supervision is paramount for diabetics considering intermittent fasting because it carries significant risks, including severe hypoglycemia, hyperglycemia rebound, and potential nutrient deficiencies if not managed correctly. A doctor can provide a personalized plan, adjust medication dosages safely, monitor for complications, and ensure that intermittent fasting contributes positively to diabetes management without endangering health. This professional guidance is critical for safe and effective implementation of intermittent fasting for diabetics.
References
- https://www.diabetes.org/healthy-living/medication-treatments/intermittent-fasting
- https://www.niddk.nih.gov/health-information/diet-nutrition/eating-drinking-physical-activity/intermittent-fasting-what-to-know
- https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/is-intermittent-fasting-safe-for-people-with-diabetes
- https://healthmatters.wharton.upenn.edu/articles/intermittent-fasting-for-type-2-diabetes/
- https://health.clevelandclinic.org/intermittent-fasting-for-diabetes/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9399227/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9917542/
- Intermittent fasting


