Metformin is widely considered the best first-line medication for type 2 diabetes due to its long-standing safety record, affordability, and effectiveness at lowering blood sugar. However, newer classes of drugs, specifically GLP-1 receptor agonists (like Ozempic) and SGLT2 inhibitors (like Jardiance), are now ranked among the best options for patients who also need support with weight loss or cardiovascular health. This guide explores the most effective medications available today to help you understand which options might align with your specific health needs. Navigating the pharmaceutical landscape of diabetes management can be complex, as the “best” medication is no longer solely defined by how much it lowers glucose, but by how well it protects organs and fits a patient’s lifestyle.
Metformin: The Gold Standard First-Line Treatment

For decades, Metformin has remained the cornerstone of type 2 diabetes management. According to the American Diabetes Association (ADA) and major international health organizations, it is the preferred initial pharmacologic agent for the treatment of type 2 diabetes unless there are specific contraindications.
Mechanism of Action
Metformin belongs to a class of drugs called biguanides. It works primarily by targeting the liver, reducing the amount of glucose (sugar) the liver produces and releases into the bloodstream. Additionally, it acts as an insulin sensitizer, helping the body’s muscle cells respond more effectively to insulin so they can absorb glucose from the blood for energy. Unlike some other diabetes medications, Metformin does not stimulate the pancreas to produce more insulin, which is a key factor in its safety profile.
Key Benefits
The endurance of Metformin as the top choice is due to a “trifecta” of benefits:
* Cost-Effectiveness: It is widely available as a generic drug, making it affordable for almost all patients, regardless of insurance status.
* Weight Neutrality: Unlike older classes of drugs that often caused significant weight gain, Metformin is weight-neutral and may even promote modest weight loss in some patients.
* Long-Term Safety: With decades of clinical data, the long-term safety profile of Metformin is well-understood. It is also associated with a very low risk of hypoglycemia (dangerously low blood sugar).
Side Effects and Mitigation
The most common drawbacks of Metformin are gastrointestinal. Patients frequently report nausea, diarrhea, or abdominal discomfort, particularly when starting the medication. To mitigate these issues, physicians typically start patients on a low dose and gradually increase it. Furthermore, the extended-release (XR) formulation of Metformin is highly effective at reducing digestive side effects compared to the immediate-release version.
GLP-1 Receptor Agonists for Weight Management
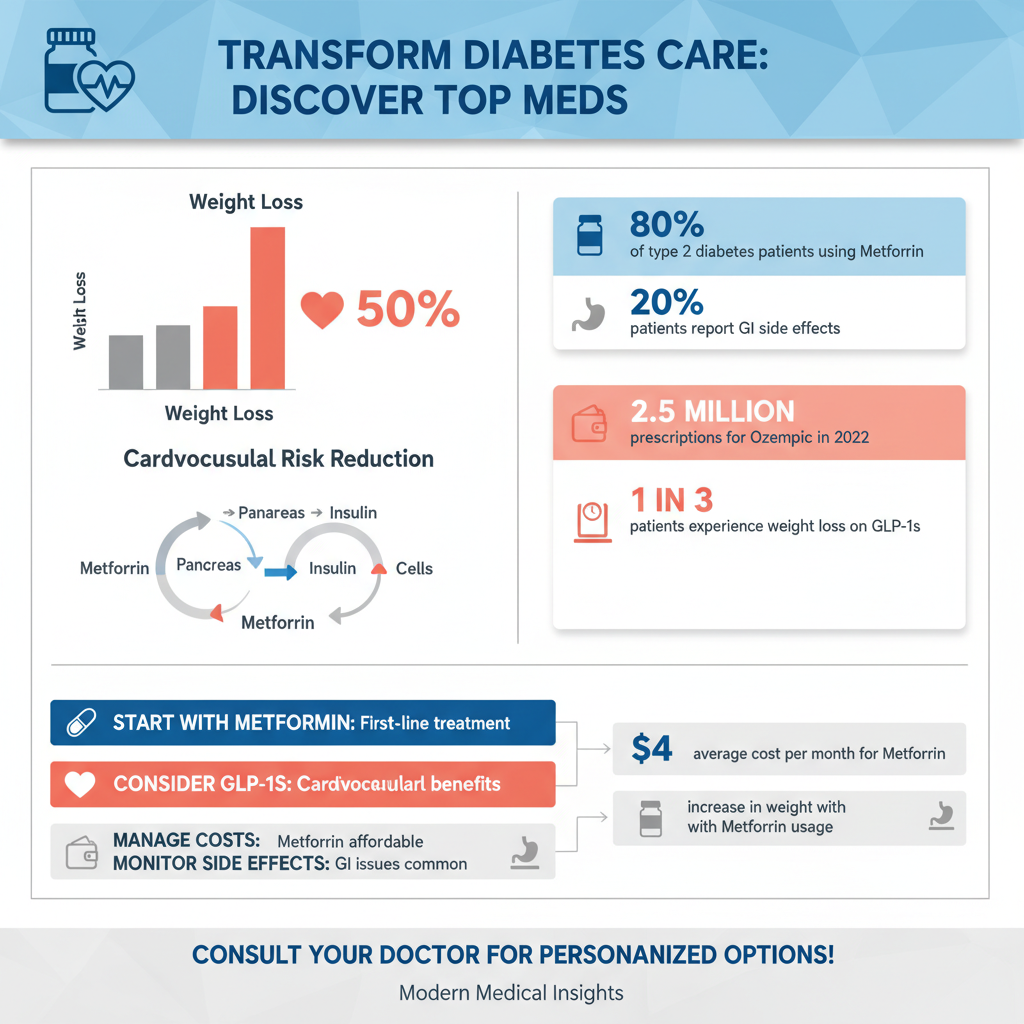

In recent years, Glucagon-like peptide-1 (GLP-1) receptor agonists have revolutionized diabetes care. Originally designed for glucose control, their potent effects on body weight have elevated them to top-tier status for diabetic patients struggling with obesity.
Top Brand Names
This class includes several widely recognized injectable medications. Ozempic (semaglutide) has become a household name due to its high efficacy. Other major options include Trulicity (dulaglutide) and Victoza (liraglutide). These are generally administered via a subcutaneous injection, with Ozempic and Trulicity requiring only weekly dosing, while Victoza is taken daily.
Dual Mechanism: Blood Sugar and Appetite
GLP-1 agonists work by mimicking the action of the endogenous GLP-1 hormone. This achieves glucose control through several pathways:
1. Insulin Secretion: They stimulate the pancreas to release insulin when blood sugar levels are high.
2. Glucagon Suppression: They prevent the liver from releasing too much sugar.
3. Gastric Emptying: Crucially, they slow down the rate at which the stomach empties food into the small intestine. This leads to a prolonged sensation of fullness (satiety) and a significant reduction in appetite.
Cardiovascular and Weight Benefits
Beyond glucose control, the ability of these drugs to induce significant weight loss—often ranging from 10% to 15% of body weight—is profound. Furthermore, clinical trials such as the LEADER and SUSTAIN trials have demonstrated that specific GLP-1 agonists reduce the risk of major adverse cardiovascular events (MACE), including stroke and heart attack, in patients with established cardiovascular disease.
SGLT2 Inhibitors for Heart and Kidney Health
Sodium-glucose cotransporter-2 (SGLT2) inhibitors represent another paradigm shift in diabetes management, moving the focus from simple glucose lowering to organ protection.
Popular Options and Mechanism
Leading medications in this class include Jardiance (empagliflozin) and Farxiga (dapagliflozin). Unlike most diabetes drugs that focus on insulin, SGLT2 inhibitors work on the kidneys. They block the reabsorption of glucose back into the bloodstream, prompting the kidneys to filter excess sugar out of the body through urine.
The “Best” Choice for Comorbidities
For patients with a history of heart failure or chronic kidney disease (CKD), SGLT2 inhibitors are often considered the best medical option, sometimes even independent of A1C levels.
* Heart Failure: These drugs have been proven to significantly reduce the risk of hospitalization for heart failure and cardiovascular death.
* Kidney Protection: They slow the progression of kidney disease, offering a vital protective mechanism for diabetic patients, who are at high risk for renal failure.
Side Effects to Consider
Because these medications work by increasing sugar in the urine, they create an environment that can be conducive to bacterial and fungal growth. Consequently, the most common side effects are urinary tract infections (UTIs) and genital yeast infections. Patients are advised to maintain good hygiene and hydration to mitigate these risks.
DPP-4 Inhibitors for Daily Maintenance
Dipeptidyl peptidase-4 (DPP-4) inhibitors offer a solid, moderate treatment option for patients who need assistance managing blood sugar without the complexity of injections or the risks associated with older drugs.
Role and Mechanism
Commonly known by brand names like Januvia (sitagliptin) and Onglyza (saxagliptin), these oral medications work by blocking the enzyme that breaks down incretin hormones (like GLP-1). By keeping these natural hormones active longer, DPP-4 inhibitors help the body produce more insulin—but importantly, they do so mainly when blood sugar is elevated.
Weight-Neutral and Well-Tolerated
DPP-4 inhibitors are characterized by their tolerability. They are considered “weight-neutral,” meaning they do not cause weight gain, but they also do not typically induce weight loss. Their side effect profile is mild compared to other classes, causing fewer digestive issues than Metformin and virtually no risk of hypoglycemia when used alone.
Clinical Usage
Doctors typically prescribe DPP-4 inhibitors as an add-on therapy. If a patient is taking Metformin but has not yet reached their A1C goal, adding a drug like Januvia is a safe, effective next step, particularly for elderly patients or those who cannot tolerate the side effects of more aggressive therapies.
Sulfonylureas and Meglitinides
Before the advent of GLP-1s and SGLT2s, Sulfonylureas were the primary alternative to Metformin. While their usage has declined in favor of newer drugs with better cardiovascular profiles, they remain relevant in specific contexts.
Cost-Effective Pancreatic Stimulation
Medications such as Glipizide, Glimepiride, and Glyburide fall into this category. They work by directly stimulating the beta cells in the pancreas to release more insulin. They are highly effective at lowering blood sugar rapidly and are among the least expensive diabetes medications available, often costing pennies per dose.
Risks: Hypoglycemia and Weight Gain
The major downside to Sulfonylureas is their “blunt instrument” approach. Because they stimulate insulin release regardless of the current blood sugar level, they carry a significantly higher risk of hypoglycemia (low blood sugar) compared to newer agents. Additionally, because insulin is a storage hormone, these drugs often cause weight gain, which can be counterproductive for type 2 diabetes management.
Why They Are Still Used
Despite the risks, these medications are still used effectively for patients who need immediate, potent blood sugar reduction and for whom cost is a prohibitive barrier to accessing newer drugs like Ozempic or Jardiance.
Mounjaro (Tirzepatide): The New Dual Agonist
The most recent advancement in diabetes pharmacotherapy is Mounjaro (tirzepatide), a medication that is redefining efficacy standards.
First-in-Class Dual Action
Mounjaro is unique because it targets two different hormone receptors: glucose-dependent insulinotropic polypeptide (GIP) and GLP-1. By activating both receptors, it creates a synergistic effect that controls blood sugar more effectively than targeting GLP-1 alone.
Superior Clinical Data
Clinical trials, specifically the SURPASS program, have shown that Mounjaro is superior to standard GLP-1 agonists regarding A1C reduction. Perhaps more notably, it has demonstrated the highest weight loss potential of any diabetes medication currently on the market, with some patients losing over 20% of their body weight.
Availability and Status
Mounjaro is FDA-approved for the treatment of type 2 diabetes. While it comes with a higher price tag similar to other branded injectables, its dual efficacy makes it a premier option for patients with high A1C levels and significant obesity.
How to Choose the Right Medication for You
Selecting the “best” medication is a nuanced process that involves collaboration between the patient and the provider. There is no single pill that is perfect for everyone.
Factors Doctors Consider
Physicians rely on guidelines from the American Diabetes Association to tailor treatment. Key decision-making factors include:
* Comorbidities: If a patient has atherosclerotic cardiovascular disease, heart failure, or chronic kidney disease, guidelines strongly recommend prioritizing SGLT2 inhibitors or GLP-1 agonists, regardless of A1C.
* A1C Goals: The distance between a patient’s current A1C and their goal (usually <7%) dictates the potency of the required drug.
* Insurance and Cost: Newer branded drugs can be expensive; formularies often dictate which specific brands are accessible.
Lifestyle and Preferences
Patient preference plays a massive role in adherence. Some patients have a phobia of needles, ruling out GLP-1s despite their benefits. Others may prioritize weight loss above all else. Dietary habits and the ability to manage potential gastrointestinal side effects also influence the choice.
Combination Therapy
It is important to understand that diabetes is a progressive condition. Monotherapy (using one drug) often eventually becomes insufficient. Combination therapy—such as taking Metformin alongside an SGLT2 inhibitor—is a common and effective strategy to attack the disease from multiple angles simultaneously.
Finding the best meds for type 2 diabetes is rarely a one-size-fits-all process; it requires balancing blood sugar control with other health priorities like weight management and heart protection. While Metformin remains the foundation of treatment, newer options like GLP-1s and SGLT2s offer powerful additional benefits that are changing how the disease is managed. Consult with your endocrinologist or primary care physician to review your current A1C levels and determine if adjusting your medication regimen could lead to better long-term health outcomes.
Frequently Asked Questions
What is the first-line medication usually prescribed for Type 2 diabetes?
Most healthcare providers prescribe **Metformin** as the primary treatment because it effectively lowers the amount of sugar your liver produces and improves how your body uses insulin. It is widely considered the standard of care due to its long history of safety, affordability, and neutral effect on weight compared to older drugs like sulfonylureas. However, doctors may skip Metformin if a patient has specific kidney issues or severe gastrointestinal intolerance.
Which Type 2 diabetes medications are best for promoting weight loss?
**GLP-1 receptor agonists** (such as Semaglutide, known by brand names like Ozempic and Rybelsus) and dual agonists (like Tirzepatide/Mounjaro) are currently considered the most effective options for significant weight loss. These medications work by mimicking hormones that slow down gastric emptying and signal fullness to the brain, helping patients reduce calorie intake while managing blood sugar. Because obesity is a major risk factor for diabetes complications, these drugs address both the root cause and the symptoms simultaneously.
How do SGLT2 inhibitors like Jardiance compare to other diabetes treatments?
Unlike medications that focus on insulin production or sensitivity, **SGLT2 inhibitors** (including Jardiance and Farxiga) lower blood sugar by preventing the kidneys from reabsorbing glucose, allowing it to be expelled through urine. These drugs are particularly valuable for patients with existing heart conditions or kidney disease, as clinical trials have shown they offer significant protection against heart failure and renal decline. They are often prescribed alongside Metformin for patients who need additional A1C reduction and cardiovascular support.
What are the common side effects of popular Type 2 diabetes drugs?
Side effects vary by drug class; for example, Metformin is frequently associated with initial stomach upset and diarrhea, which can often be mitigated by taking it with food or using the extended-release version. Newer injectables like **GLP-1 agonists** often cause nausea and vomiting as the body adjusts to the medication, while SGLT2 inhibitors carry a higher risk of urinary tract and yeast infections due to increased sugar in the urine. It is crucial to discuss these potential reactions with a doctor to find a tolerated balance between efficacy and comfort.
Can I eventually stop taking medication if I manage my diabetes with diet and exercise?
It is possible for some patients to achieve **diabetes remission** and discontinue medication through significant lifestyle changes, substantial weight loss, and dietary management. However, Type 2 diabetes is a progressive and chronic condition, meaning that even if blood sugar levels normalize temporarily, the underlying insulin resistance may persist. You should never stop taking prescribed medication without strict medical supervision, as sudden cessation can lead to dangerous spikes in blood glucose levels.
References
- Type 2 diabetes – Diagnosis and treatment – Mayo Clinic
- Insulin, Medicines, & Other Diabetes Treatments – NIDDK
- https://www.nhs.uk/conditions/type-2-diabetes/medicine/
- What Are My Options for Type 2 Diabetes Medications? | ADA
- https://my.clevelandclinic.org/health/treatments/13902-type-2-diabetes-medication
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes/type-2-diabetes-treatment
- Type 2 diabetes: Which medication is best for me? – Harvard Health
- https://www.cdc.gov/diabetes/managing/medication-insulin.html


