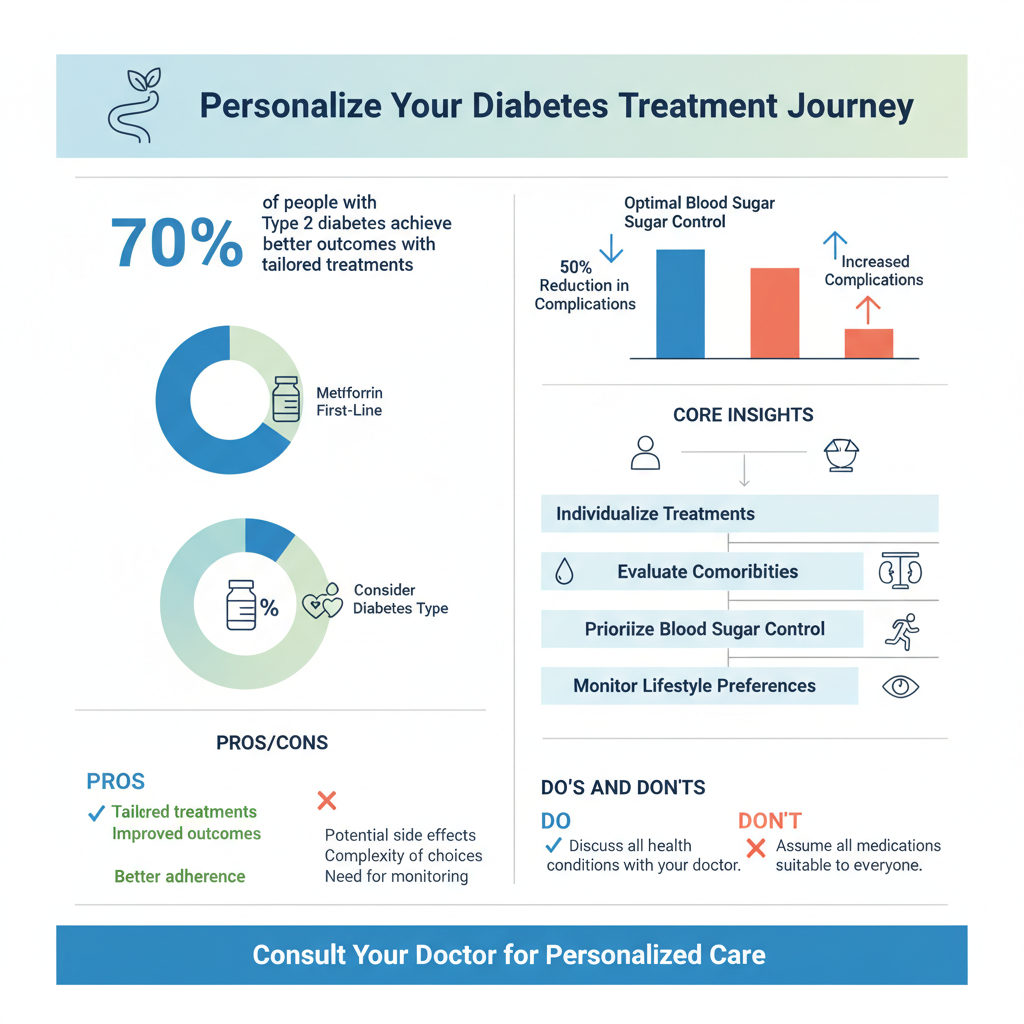
There isn’t a single “best” diabetes drug for everyone, as the most effective treatment is highly individualized. What works optimally depends on a range of factors including the type of diabetes, other existing health conditions, lifestyle, your specific A1C levels, and how your body responds to medication. This guide explores various drug classes and the critical factors your healthcare provider considers to tailor the ideal treatment plan for you, aiming to optimize blood sugar control while minimizing side effects and enhancing overall health.
The Personal Nature of Diabetes Treatment

When it comes to managing diabetes, the idea of a “one-size-fits-all” solution simply doesn’t exist. Your diabetes journey, and therefore your treatment plan, is incredibly personal, like a custom-tailored suit designed just for you. This approach is crucial because what might be highly effective for one person could be less suitable or even carry risks for another.
* No single “best” drug universally applies; treatment is highly individualized. Imagine your body as a complex symphony orchestra. Each instrument (organ system) plays a vital role, and diabetes can affect different instruments in unique ways. Your doctor acts as the conductor, choosing the right medications to bring harmony back to your system. This means considering your unique genetic makeup, how long you’ve had diabetes, and even your daily routine and preferences.
* Key factors include diabetes type (Type 1 or Type 2), presence of comorbidities (heart disease, kidney issues), lifestyle, and patient preferences. For instance, someone with Type 1 diabetes will always require insulin, as their body produces none. However, for Type 2 diabetes, the choices are vast. If you have existing heart disease or kidney problems, certain drugs offer protective benefits beyond just lowering blood sugar, making them a preferred choice. Your lifestyle, including your diet and exercise habits, also plays a huge role. Do you prefer a daily pill or a weekly injection? Are you comfortable monitoring your blood sugar frequently? Your personal preferences and how a medication fits into your life are vital for long-term adherence and success.
* The primary goal is to achieve optimal blood sugar control while preventing complications and minimizing adverse effects. The ultimate aim of any diabetes treatment is to keep your blood glucose levels within a healthy target range. This not only helps you feel better day-to-day but, more importantly, reduces the risk of serious long-term complications like nerve damage, kidney disease, vision loss, and cardiovascular issues. Balancing effective blood sugar lowering with a good quality of life and minimal side effects is always at the forefront of your healthcare team’s mind.
Foundational Medications: Metformin and Sulfonylureas

For many individuals embarking on their Type 2 diabetes treatment journey, two classes of medication often come up first: Metformin and Sulfonylureas. These have been mainstays in diabetes care for decades, and for good reason, offering effective blood sugar control, often at an affordable cost.
* Metformin: Often the first-line therapy for Type 2 diabetes, working by reducing glucose production by the liver and improving insulin sensitivity. Think of Metformin as a diligent manager for your liver. It tells your liver to slow down its glucose production, especially overnight, which is a common issue in Type 2 diabetes. It also helps your body’s cells become more responsive to the insulin you do produce, essentially making your own insulin work more efficiently. A huge plus is that Metformin typically doesn’t cause weight gain and has a low risk of hypoglycemia (low blood sugar) when used alone. Many people also find it beneficial for its potential cardiovascular protective effects. While generally well-tolerated, some individuals might experience mild gastrointestinal side effects like nausea or diarrhea, especially when first starting the medication.
* Sulfonylureas: An older class of drugs that stimulate the pancreas to produce more insulin, commonly used alone or in combination. Sulfonylureas are like a gentle alarm clock for your pancreas, prompting it to release more insulin. This can lead to a quick and effective drop in blood sugar levels. They are often prescribed when Metformin alone isn’t sufficient or if Metformin isn’t tolerated. Because they actively stimulate insulin release, a key consideration with sulfonylureas is the increased risk of hypoglycemia, particularly if meals are skipped or delayed. They can also sometimes lead to modest weight gain. Despite these considerations, their effectiveness and affordability make them a valuable option in many treatment plans.
* Both have distinct benefits, potential side effects, and cost considerations, making them important early choices. Your doctor will weigh these factors carefully, considering your specific health profile. For example, if you have significant kidney issues, Metformin might not be the best choice. If you’re prone to erratic meal schedules, a sulfonylurea might need more careful management to avoid hypoglycemia. The good news is that these foundational medications provide excellent starting points for many people, often forming the backbone of their diabetes management plan before other options are explored.
Newer Classes with Added Benefits: SGLT2 Inhibitors

In recent years, the landscape of diabetes treatment has seen exciting innovations. Among the most impactful are the SGLT2 inhibitors, a class of drugs that not only lower blood sugar but also offer significant benefits for your heart and kidneys, making them game-changers for many.
* How they work: These drugs help the kidneys remove glucose from the body through urine, lowering blood sugar levels. Imagine your kidneys as filters that normally reabsorb almost all the sugar from your blood back into your body. SGLT2 inhibitors essentially “turn down” this reabsorption mechanism, allowing more glucose to be flushed out through your urine. This unique action helps reduce blood sugar independently of insulin, which is quite different from many other diabetes medications. It’s a clever way to lighten the glucose load on your system!
* Beyond glucose control: SGLT2 inhibitors have demonstrated significant cardiovascular and renal protective benefits, making them crucial for many. This is where SGLT2 inhibitors truly shine and have revolutionized diabetes care. Large clinical trials have shown that these medications can dramatically reduce the risk of heart failure, heart attacks, strokes, and the progression of kidney disease in people with Type 2 diabetes, even those without pre-existing heart or kidney conditions. For individuals already living with cardiovascular disease or chronic kidney disease, these benefits are particularly profound, making SGLT2 inhibitors a cornerstone of their treatment strategy.
* Common examples include empagliflozin, canagliflozin, and dapagliflozin, with specific considerations for each. You might recognize names like Jardiance (empagliflozin), Invokana (canagliflozin), or Farxiga (dapagliflozin). While they share the core mechanism, there can be subtle differences in their specific indications and side effect profiles. Common side effects include an increased risk of urinary tract infections (UTIs) and yeast infections due to the increased sugar in the urine. Your doctor will discuss these with you, along with other rare but serious potential side effects, to ensure this class is the right fit for your health profile and lifestyle.
Injectable Non-Insulin Options: GLP-1 Receptor Agonists
Another class of modern diabetes medications that has garnered significant attention are the GLP-1 Receptor Agonists. These injectables offer more than just blood sugar control; they bring a host of additional benefits that can greatly improve the health and well-being of many individuals with Type 2 diabetes.
* Mechanism: Mimic a natural hormone to boost insulin release, suppress glucagon, and slow gastric emptying, leading to improved blood sugar control and satiety. Our bodies naturally produce hormones called “incretins” when we eat, which help regulate blood sugar. GLP-1 receptor agonists are synthetic versions of one of these powerful incretins. They work in multiple ways: by telling your pancreas to release more insulin when blood sugar is high, by preventing your liver from releasing too much stored glucose (by suppressing glucagon), and by slowing down how quickly food leaves your stomach. This slower digestion not only helps manage post-meal blood sugar spikes but also contributes to a feeling of fullness.
* Key advantages: Often lead to weight loss and have shown strong cardiovascular benefits, making them valuable for specific patient profiles. The weight loss potential is a major advantage for many people living with Type 2 diabetes, as excess weight is often a contributing factor to the condition. This weight loss isn’t just cosmetic; it can further improve insulin sensitivity and overall metabolic health. Furthermore, similar to SGLT2 inhibitors, GLP-1 receptor agonists have demonstrated impressive cardiovascular benefits, reducing the risk of heart attacks and strokes in individuals with established cardiovascular disease. These dual benefits make them incredibly valuable, especially for those seeking both robust blood sugar control and help with weight management, alongside heart protection.
* Administered via injection (daily or weekly), examples include semaglutide, liraglutide, and dulaglutide. These medications are typically given as subcutaneous injections, using a small, easy-to-use pen device. The frequency can vary, with some requiring daily injections (like liraglutide, known as Victoza) and others offering the convenience of once-weekly dosing (such as semaglutide, branded as Ozempic or Rybelsus for its oral form, and dulaglutide, branded as Trulicity). Common side effects can include nausea, vomiting, or diarrhea, especially when first starting treatment, but these often improve over time. Your healthcare provider will guide you through the injection process and discuss how to manage any potential side effects.
Insulin Therapy: A Cornerstone for Many
When we talk about diabetes treatment, insulin often comes to mind, and for good reason. For millions, it’s not just a treatment option; it’s an essential, life-saving medication, playing a pivotal role in managing both Type 1 and Type 2 diabetes effectively.
* Essential for Type 1 diabetes: Insulin is life-saving and required for all individuals with Type 1 diabetes due to a lack of natural insulin production. If you have Type 1 diabetes, your body’s immune system has mistakenly attacked and destroyed the insulin-producing cells in your pancreas. This means your body produces little to no insulin, making daily insulin injections absolutely vital for survival. Without insulin, your body cannot use glucose for energy, leading to dangerously high blood sugar levels. Insulin therapy replaces the hormone your body can no longer make, allowing glucose to enter your cells and keep you healthy.
* For Type 2 diabetes: Insulin therapy becomes necessary when oral medications or other injectables are no longer sufficient to control blood sugar. While Type 2 diabetes initially involves insulin resistance or insufficient insulin production, over time, the pancreas can become “tired” and produce less and less insulin. When other medications can no longer effectively manage blood sugar levels, or if your A1C is very high at diagnosis, your doctor may recommend adding insulin. It’s important to understand that needing insulin for Type 2 diabetes is not a sign of failure; it’s simply the natural progression of the disease for many individuals, and a powerful tool to protect your health.
* Various types exist (rapid-acting, long-acting, pre-mixed), chosen based on individual needs and lifestyle. Insulin isn’t a single drug; it’s a family of medications with different durations of action.
* Rapid-acting insulins (like lispro, aspart, glulisine) are taken just before or with meals to cover the glucose spike from food.
* Long-acting insulins (like glargine, detemir, degludec) provide a steady basal level of insulin throughout the day or night, helping to control blood sugar between meals and overnight.
* Intermediate-acting and pre-mixed insulins also exist, offering various combinations and durations.
Your doctor will work closely with you to determine the best type and regimen based on your blood sugar patterns, diet, physical activity, and overall lifestyle, empowering you to live your fullest life while managing your diabetes.
Other Oral Agents and Combination Therapies
Beyond the foundational and newer, high-benefit classes, there are several other oral agents that play important roles in diabetes management. Often, these medications are used in combination with others to create a comprehensive and effective treatment strategy, highlighting the individualized approach to diabetes care.
* DPP-4 Inhibitors: Enhance the body’s natural incretin system to improve insulin secretion and reduce glucagon levels, generally well-tolerated. Think of DPP-4 inhibitors (like sitagliptin, saxagliptin, linagliptin) as protectors of your body’s natural incretins. These are hormones (like GLP-1) that help stimulate insulin release and lower glucose levels, but they are quickly broken down by an enzyme called DPP-4. DPP-4 inhibitors block this enzyme, allowing your natural incretins to work longer and more effectively. The beauty of these drugs is that they typically don’t cause weight gain, have a low risk of hypoglycemia when used alone, and are generally very well-tolerated, with few side effects. They’re a gentle yet effective way to fine-tune blood sugar control, often used as an add-on therapy.
* Thiazolidinediones (TZDs): Improve insulin sensitivity in muscle and fat tissue, but require careful monitoring for specific side effects. TZDs, such as pioglitazone, work by making your body’s cells more responsive to insulin, particularly in muscle and fat tissues. This helps glucose move out of your bloodstream and into your cells where it can be used for energy. They can be very effective in lowering A1C and offer durable glucose control. However, they do come with specific considerations, including a risk of fluid retention (which can be a concern for those with heart failure), weight gain, and a slightly increased risk of bone fractures. Due to these potential side effects, your doctor will carefully assess your overall health and monitor you closely if a TZD is part of your treatment plan.
* Combination Pills: Many single pills combine two or more drug classes, simplifying treatment regimens for patients. To make managing diabetes simpler and improve adherence, pharmaceutical companies have developed combination pills. These medications pack two or even three different diabetes drugs into one tablet. For example, you might find a pill that combines Metformin with a DPP-4 inhibitor, or Metformin with an SGLT2 inhibitor. This approach reduces the number of pills you need to take each day, making your treatment regimen less complex and easier to remember, which can lead to better overall blood sugar control. Your doctor might suggest a combination pill if you need multiple medications to reach your blood sugar goals.
Partnering with Your Healthcare Provider
Navigating the complexities of diabetes treatment is a team effort, and you are the most important member of that team. Your healthcare provider is your guide, but active participation and open communication from your side are absolutely crucial for finding and maintaining the “best” diabetes drug regimen for you.
* Regular consultations and monitoring are crucial to assess treatment effectiveness, manage side effects, and make necessary adjustments. Diabetes is a dynamic condition, and your body’s needs can change over time. Regular check-ups with your doctor are not just about getting prescriptions; they’re opportunities to review your progress, discuss your blood sugar readings, check your A1C, and monitor other important health markers like blood pressure, cholesterol, and kidney function. This ongoing monitoring allows your healthcare team to ensure your current medication plan is working effectively, make small tweaks, or even suggest more significant changes if needed. Remember, this isn’t a static plan but a living, evolving strategy!
* Openly discuss your health goals, lifestyle, potential side effects, and financial considerations with your doctor. Don’t be shy about sharing everything that impacts your diabetes management. Do you have specific health goals, like losing weight or lowering your risk of heart disease? What does your daily routine look like – do you travel frequently, or have a busy work schedule? Are you experiencing any bothersome side effects that impact your quality of life? Are cost or insurance coverage a concern? All these factors are incredibly important. Your doctor needs this information to truly tailor a plan that works *for you*, not just on paper, but in your real life. Your honest feedback is invaluable for shared decision-making.
* The “best” diabetes drug evolves as your condition changes and new research emerges, emphasizing continuous collaboration with your medical team. What’s optimal today might not be optimal five years from now. Diabetes can progress, your body’s response to medication can shift, and exciting new drugs and research are constantly emerging. Staying in close communication with your doctor, diabetes educators, dietitians, and pharmacists ensures you’re always on the most effective and up-to-date treatment path. This continuous partnership empowers you to adapt to changes and take advantage of new advancements, keeping you ahead in your diabetes management journey.
Ultimately, identifying the “best” diabetes drug is a journey that requires close collaboration with your healthcare team. There isn’t a one-size-fits-all solution, but rather a personalized strategy that considers your unique health profile, lifestyle, and treatment goals. By staying informed and actively participating in your care, you can work towards an effective treatment plan that helps you manage your diabetes and lead a healthier life. Always consult your doctor before making any changes to your medication regimen.
Frequently Asked Questions
What is considered the “best” diabetes drug for someone newly diagnosed with Type 2 diabetes?
There isn’t a single “best” diabetes drug for everyone, as treatment is highly individualized. However, metformin is typically the first-line medication recommended for most people newly diagnosed with Type 2 diabetes due to its effectiveness, low risk of hypoglycemia, and potential cardiovascular benefits. Its role is crucial in improving insulin sensitivity and reducing glucose production by the liver, making it a cornerstone of initial diabetes management.
How do healthcare providers choose the right diabetes medication for an individual?
Healthcare providers consider several factors when selecting the optimal diabetes medication, including the patient’s A1C level, duration of diabetes, presence of comorbidities like heart disease or kidney disease, weight concerns, potential side effects, and cost. They also take into account patient preferences and lifestyle, aiming for a personalized approach that effectively manages blood sugar while minimizing risks and improving overall quality of life.
Which diabetes medications also offer the benefit of weight loss for people with Type 2 diabetes?
Several newer classes of diabetes medications offer the additional benefit of weight loss, which can be particularly advantageous for individuals with Type 2 diabetes. These include GLP-1 receptor agonists (like semaglutide or liraglutide) and SGLT2 inhibitors (such as empagliflozin or dapagliflozin). These drugs work through different mechanisms to help reduce blood sugar levels while also promoting weight reduction, offering a dual benefit for many patients.
Why is it crucial to discuss potential side effects with your doctor before starting a new diabetes drug?
Discussing potential side effects with your doctor before starting any new diabetes drug is crucial for several reasons. It helps you understand what to expect, enables your doctor to monitor for adverse reactions, and ensures the medication is safe given your other health conditions. Open communication allows for adjustments to the treatment plan if side effects are intolerable or if other health issues arise, ensuring effective and safe blood sugar management.
Can lifestyle changes, like diet and exercise, ever replace the need for diabetes medication?
For some individuals, particularly those in the early stages of Type 2 diabetes or prediabetes, significant and sustained lifestyle changes, including a healthy diet and regular exercise, can dramatically improve blood sugar control and, in some cases, delay or even prevent the need for medication. However, for many, especially as the disease progresses, medication remains an essential component of optimal blood sugar management alongside lifestyle modifications to prevent complications.
References
- https://diabetes.org/health-wellness/medication
- https://diabetesjournals.org/care/issue/47/Supplement_1/S116
- https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/in-depth/diabetes-medications/art-20046902
- https://www.niddk.nih.gov/health-information/diabetes/overview/medications-treatments
- https://www.cdc.gov/diabetes/managing/medication.html
- Diabetes medication
- https://www.who.int/publications/i/item/9789240078832
- https://www.nytimes.com/guides/well/how-to-treat-type-2-diabetes


