The “best food” for managing diabetes isn’t a single item, but rather a balanced dietary approach focused on whole, unprocessed foods rich in fiber, lean protein, and healthy fats. These foods help stabilize blood sugar, manage weight, and reduce the risk of diabetes complications. By prioritizing specific food groups, individuals with diabetes can significantly improve their health outcomes. This guide will outline the top food categories you should prioritize to effectively manage your diabetes.
Understanding Diabetes-Friendly Nutrition

Navigating nutrition with diabetes might seem daunting at first, but it truly boils down to making informed choices that support your body’s ability to manage blood sugar. It’s not about deprivation, but rather empowerment through knowledge! Thinking about your meals in terms of key nutritional principles can make a huge difference in your daily well-being and long-term health.
* Focus on Glycemic Index (GI): The Glycemic Index is a valuable tool that helps us understand how quickly a carbohydrate-containing food raises blood sugar. Foods with a low GI are digested and absorbed more slowly, leading to a gradual and more manageable rise in blood sugar, preventing those unwelcome spikes. Think of vibrant non-starchy vegetables, most fruits, whole grains, and legumes as your low-GI allies. Prioritizing these not only keeps your blood sugar steadier but also helps you feel fuller for longer, which can be a huge benefit for weight management. Conversely, high-GI foods like white bread, sugary drinks, and processed snacks cause rapid surges, so they are best limited or avoided. Understanding and applying GI principles doesn’t mean you can never enjoy a higher-GI food, but it encourages pairing it with protein and healthy fats to slow down its impact.
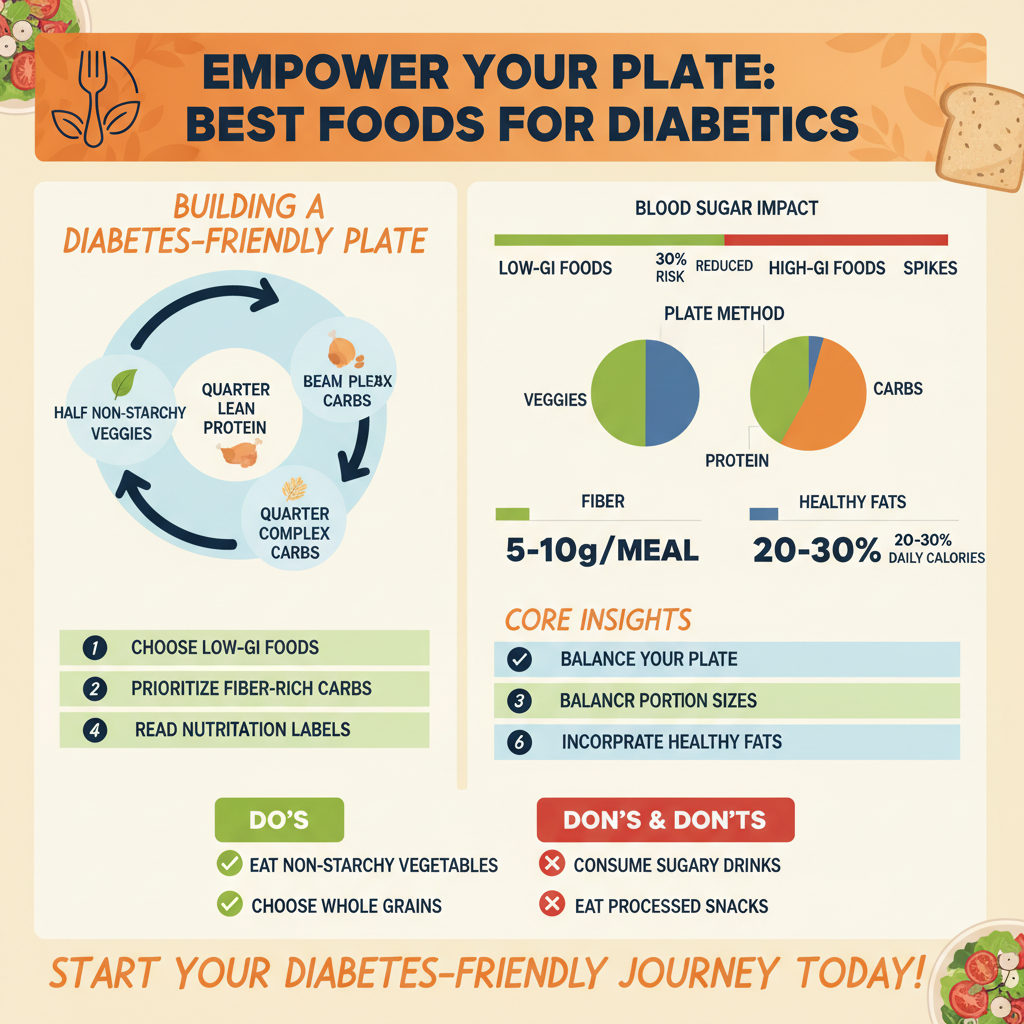
* Carbohydrate Management: Carbohydrates are a primary source of energy, but they also have the most direct impact on blood sugar levels. The key isn’t to eliminate them entirely, but rather to manage their quantity and quality. Focus on complex carbohydrates, often found in whole grains, vegetables, and legumes. These are rich in fiber, which slows digestion and sugar absorption, providing a steady release of energy. Simple carbohydrates, such as those found in candies, sodas, and many processed foods, lack fiber and nutrients, leading to rapid blood sugar spikes. Learning about appropriate portion sizes for carbohydrates is critical. Tools like the “plate method” – filling half your plate with non-starchy vegetables, a quarter with lean protein, and a quarter with complex carbohydrates – can be incredibly helpful for visually portioning meals and ensuring a balanced intake. Reading nutrition labels to check for total carbohydrates, fiber, and added sugars will become your superpower.
* Balance Macronutrients: Achieving a harmonious balance of complex carbohydrates, lean proteins, and beneficial fats in every meal is a cornerstone of diabetes management. This trio works synergistically to promote satiety, stabilize blood sugar, and provide sustained energy. Complex carbohydrates offer the primary energy source, but when paired with protein and healthy fats, their absorption slows down, preventing rapid blood sugar fluctuations. Protein helps build and repair tissues, keeps you feeling full, and has a minimal impact on blood sugar directly. Healthy fats, while calorie-dense, are vital for hormone production, nutrient absorption, and also contribute significantly to satiety. A well-balanced meal might include a serving of grilled salmon (protein and healthy fat) with a generous portion of steamed broccoli (fiber-rich carb) and a small side of quinoa (complex carb). This balance helps regulate appetite, reduce cravings, and maintains stable energy levels throughout the day.
Non-Starchy Vegetables: Your Plate’s Foundation

When building your ideal plate for diabetes management, non-starchy vegetables should be the cornerstone. Think of them as your vibrant, nutrient-dense superheroes, ready to fill you up without overwhelming your system with carbohydrates or calories. They are truly nature’s way of providing abundant health benefits.
* High Fiber, Low Carb: Vegetables like spinach, kale, broccoli, bell peppers, green beans, asparagus, cauliflower, and zucchini are superstars because they offer an incredible nutritional punch with minimal impact on blood sugar. They are brimming with essential vitamins (like Vitamin C and K), minerals (such as potassium and folate), and powerful antioxidants that protect your cells from damage. Most importantly, they are incredibly high in fiber, both soluble and insoluble. This fiber content is a game-changer for diabetics. It slows down digestion, meaning that any carbohydrates you consume are absorbed more gradually, preventing sharp blood sugar spikes. Furthermore, fiber helps improve gut health, can lower cholesterol, and promotes regular bowel movements, all contributing to overall well-being.
* Versatility in Meals: The beauty of non-starchy vegetables lies in their incredible versatility. You can effortlessly incorporate them into almost any meal, boosting nutrient intake without adding excessive carbohydrates or calories. Imagine starting your day with a fluffy omelet packed with spinach, mushrooms, and bell peppers. For lunch, a vibrant salad brimming with mixed greens, cucumber, tomatoes, and grilled chicken is a fantastic option. Dinner can feature roasted broccoli and asparagus alongside your lean protein, or a hearty stir-fry loaded with snap peas, carrots, and bok choy. Even sneaking them into smoothies or pureed soups is a clever way to increase your daily intake. Don’t be afraid to experiment with different cooking methods – steaming, roasting, grilling, or sautéing – to bring out their best flavors.
* Promotes Satiety: One of the most significant advantages of non-starchy vegetables, particularly their high fiber content, is their ability to promote satiety – that wonderful feeling of fullness and satisfaction after a meal. When you fill half your plate with these low-calorie, high-volume foods, you naturally consume fewer calories from other, more carb-dense sources. This sustained feeling of fullness helps to curb cravings, prevent overeating between meals, and ultimately supports healthy weight management. Since maintaining a healthy weight is crucial for effective diabetes management, making these vegetables a staple of your diet is a strategic move for both blood sugar control and overall health.
Smart Fruit Choices for Natural Sweetness

Fruit is nature’s candy, offering natural sweetness along with a host of vitamins, minerals, and antioxidants. While fruits do contain natural sugars, known as fructose, they also come with fiber, which helps to mitigate the impact on blood sugar. The key is making smart choices and practicing moderation.
* Lower GI Fruits: When it comes to fruit and diabetes, not all fruits are created equal in terms of their glycemic impact. Opt for berries (strawberries, blueberries, raspberries), apples, pears, oranges, and grapefruit, which generally have a lower glycemic index. These fruits release their sugars more slowly into the bloodstream due to their higher fiber content and specific sugar profiles. Berries, in particular, are packed with antioxidants and fiber, making them excellent choices. An apple a day might not only keep the doctor away but also provide a satisfying, fiber-rich snack that helps stabilize blood sugar. Enjoying these fruits can satisfy your sweet tooth without causing dramatic blood sugar spikes, especially when consumed in appropriate portions.
* Portion Control is Key: Even with lower-GI fruits, portion control remains paramount due to their natural sugar content. A typical serving size might be one small apple or orange, a half-cup of berries, or a medium peach. It’s easy to overdo it, especially with grapes or cherries. Instead of eating directly from a large bag, measure out a serving and put the rest away. Consider pairing your fruit with a source of protein or healthy fat, like a handful of almonds or a spoonful of Greek yogurt. This pairing can further slow down the absorption of sugar, making the impact on your blood sugar even gentler and keeping you feeling full and satisfied for longer.
* Whole Fruit Over Juice: This is a crucial distinction for anyone managing diabetes. Always choose whole fruits over fruit juices, even 100% natural ones. When fruit is juiced, its beneficial fiber is typically removed, leaving behind concentrated fruit sugar. This lack of fiber means the sugars are absorbed much more quickly into your bloodstream, leading to a rapid and significant blood sugar spike. Whole fruits, on the other hand, retain all their fiber, which helps slow down sugar absorption, provides a greater sense of fullness, and offers a more gradual energy release. Think of an orange versus a glass of orange juice – the whole orange provides a more complete nutritional package and a far better blood sugar response.
Whole Grains and Legumes: Complex Carb Powerhouses
For individuals managing diabetes, whole grains and legumes are indispensable components of a healthy diet. They are not just sources of carbohydrates; they are nutrient-dense powerhouses that offer sustained energy and crucial benefits for blood sugar management.
* Slow-Release Energy: Unlike refined grains (like white bread or white rice) that can cause rapid blood sugar spikes, whole grains are processed minimally, retaining all parts of the grain kernel – the bran, germ, and endosperm. This means they are rich in fiber, which significantly slows down the digestion and absorption of glucose into the bloodstream. Foods like oats (especially steel-cut or rolled), quinoa, brown rice, whole-wheat bread and pasta, and barley provide a steady, slow release of energy, helping to maintain stable blood sugar levels throughout the day. Opting for these complex carbohydrates over simple, refined versions will help you feel fuller for longer, reduce cravings, and prevent the energy crashes often associated with high-sugar foods. Always check labels to ensure products are “100% whole grain.”
* Fiber-Rich Legumes: Legumes such as lentils, black beans, chickpeas, kidney beans, and cannellini beans are nutritional superstars. They are incredibly rich in both soluble and insoluble fiber, which is fantastic for blood sugar control and digestive health. Soluble fiber, in particular, helps slow the absorption of sugar and can even help lower cholesterol levels. Beyond fiber, legumes are also an excellent source of plant-based protein, which further aids in stabilizing blood sugar and promoting satiety. Including them in your meals, whether in soups, salads, stews, or as a side dish, can significantly boost your nutrient intake and contribute to a feeling of fullness, helping you manage your appetite and weight.
* Nutrient Density: The benefits of whole grains and legumes extend far beyond just fiber and slow-release energy. They are packed with an array of essential vitamins, minerals, and antioxidants that are vital for overall health, especially for those with diabetes. You’ll find B vitamins (important for energy metabolism), magnesium (which plays a role in insulin sensitivity), iron (crucial for oxygen transport), and zinc in these foods. Their antioxidant content helps combat oxidative stress, which can be elevated in individuals with diabetes, thereby supporting cellular health and reducing the risk of long-term complications. Making these nutrient-dense options a regular part of your diet means you’re not just managing your blood sugar; you’re nourishing your entire body.
Lean Proteins: Building Blocks for Blood Sugar Control
Lean proteins are a crucial component of a diabetes-friendly diet, acting as powerful allies in managing blood sugar, preserving muscle, and keeping you feeling satisfied. Unlike carbohydrates, protein has a minimal direct impact on blood sugar levels, making it a safe and essential macronutrient to include in every meal.
* Satiety and Muscle Preservation: One of the most immediate benefits of lean protein is its incredible power to make you feel full and satisfied. Protein takes longer to digest than carbohydrates, which helps to slow down the emptying of your stomach. This leads to increased satiety, meaning you’ll feel full for longer, reducing the likelihood of overeating or snacking on less healthy options between meals. This is invaluable for weight management, a critical aspect of diabetes care. Furthermore, protein is the fundamental building block for muscle tissue. Maintaining and even building muscle mass is vital for metabolic health, as muscle burns more calories at rest than fat tissue, contributing to a healthier metabolism and improved insulin sensitivity.
* Minimal Blood Sugar Impact: Unlike carbohydrates, which directly influence blood sugar, protein has a very modest effect. When consumed, protein is primarily used for tissue repair, enzyme production, and other bodily functions, rather than immediately being converted to glucose. This makes lean protein sources an excellent choice for diabetics, as they provide necessary nutrients without causing rapid blood sugar spikes. Prioritizing lean options like skinless chicken breast, fish (especially fatty fish like salmon, tuna, and mackerel for their beneficial omega-3 fatty acids), tofu, tempeh, eggs, and Greek yogurt ensures you’re getting high-quality protein without excessive saturated fat.
* Pair with Carbs: While protein doesn’t directly raise blood sugar much, it plays a fantastic supporting role when paired with carbohydrates. Consuming protein alongside carbohydrates can significantly slow down the rate at which glucose enters the bloodstream. This means that if you’re having a complex carbohydrate like brown rice, adding a serving of lean chicken or lentils to your meal will help blunt the potential blood sugar rise, leading to a more gradual and controlled response. For example, instead of just a banana for a snack, pair it with a handful of almonds or a hard-boiled egg. This strategy not only helps stabilize blood sugar but also enhances the overall nutritional value of your meal, making it more balanced and satisfying.
Healthy Fats: Essential for Well-being
Often misunderstood, healthy fats are an indispensable part of a balanced diet for managing diabetes. Far from being something to avoid, the right kinds of fats are crucial for heart health, brain function, nutrient absorption, and contributing to satiety. The key is to choose wisely and consume them in moderation.
* Heart Health Benefits: For individuals with diabetes, who often have an increased risk of cardiovascular disease, prioritizing heart-healthy fats is paramount. Incorporate sources of monounsaturated fats (MUFAs) and polyunsaturated fats (PUFAs), especially omega-3 fatty acids, into your daily diet. Excellent sources include avocados, nuts (like almonds, walnuts, pecans), seeds (chia seeds, flaxseeds, pumpkin seeds), and olive oil. Fatty fish such as salmon, mackerel, and sardines are powerhouses of omega-3s, which are renowned for their anti-inflammatory properties, ability to lower triglycerides, and support overall heart function. These fats help lower “bad” LDL cholesterol while potentially increasing “good” HDL cholesterol, contributing to healthier arteries and reducing the risk of heart disease.
* Increased Satiety: Just like protein, healthy fats are incredibly effective at increasing satiety and helping you feel full and satisfied after meals. Fats take the longest to digest compared to carbohydrates and protein, which means they slow down the emptying of your stomach. This extended digestion period contributes to a sustained feeling of fullness, which can be invaluable in managing appetite, curbing cravings, and preventing overeating. When you feel genuinely satisfied, you’re less likely to reach for unhealthy snacks, supporting your weight management goals and ultimately, your blood sugar control.
* Moderate Intake: While healthy fats offer numerous benefits, it’s important to remember that they are calorie-dense. This means even beneficial fats should be consumed in appropriate portions. A small handful of nuts, a quarter of an avocado, or a tablespoon of olive oil are typical serving sizes. Overconsumption, even of healthy fats, can lead to excess calorie intake and potential weight gain, which can complicate diabetes management. Focus on integrating these fats as part of a balanced meal rather than adding them excessively. For instance, drizzle olive oil on your salad, add a few slices of avocado to your sandwich, or sprinkle some chia seeds into your yogurt. It’s about smart inclusion, not overindulgence.
Embracing a diet rich in non-starchy vegetables, smart fruit choices, whole grains, lean proteins, and healthy fats is the most effective strategy for managing diabetes. By making informed food choices, you can achieve better blood sugar control, reduce complications, and improve your overall quality of life. Remember that individual dietary needs can vary, so it’s crucial to consult with a healthcare professional or a registered dietitian to create a personalized meal plan tailored to your specific condition and health goals.
Frequently Asked Questions
What are the best foods for managing diabetes effectively?
The best foods for managing diabetes focus on whole, unprocessed options like non-starchy vegetables (leafy greens, broccoli), lean proteins (fish, chicken breast, tofu), and healthy fats (avocado, nuts, olive oil). These nutrient-dense choices help stabilize blood sugar levels, promote satiety, and provide essential vitamins and minerals crucial for overall diabetes health. Incorporating whole grains in moderation, based on individual needs, can also be beneficial.
Which types of carbohydrates are best for people with diabetes?
For optimal blood sugar control, prioritize complex carbohydrates with a low glycemic index, such as whole grains (oats, quinoa, brown rice), legumes (lentils, chickpeas), and most fruits and vegetables. These carbs are digested slowly, preventing rapid spikes in blood sugar compared to refined carbohydrates found in white bread, sugary drinks, and pastries. Always monitor portion sizes for any carbohydrate intake to manage your diabetic diet effectively.
How can individuals with diabetes plan healthy, balanced meals?
A practical method for planning healthy, balanced meals is the “plate method,” where half your plate is filled with non-starchy vegetables, one-quarter with lean protein, and the remaining quarter with complex carbohydrates. This approach helps ensure a balanced intake of nutrients while effectively managing portion sizes and blood sugar levels. Consulting a registered dietitian for personalized meal planning can also significantly improve diabetes management.
Why are fiber-rich foods so important for a diabetic diet?
Fiber plays a crucial role in managing diabetes by slowing down the absorption of sugar, which helps prevent sharp blood sugar spikes after meals. It also contributes to a feeling of fullness, aiding in weight management, and supports healthy digestion. Excellent fiber sources include vegetables, fruits with edible skins, whole grains, and legumes, all essential components of a diabetes-friendly eating plan.
What common foods should diabetics limit or avoid to maintain blood sugar control?
To effectively manage blood sugar, it’s crucial for individuals with diabetes to limit or avoid foods high in added sugars (sodas, candies, baked goods), refined carbohydrates (white bread, pasta, processed snacks), and unhealthy trans or saturated fats (fried foods, fatty processed meats). These items can cause rapid blood sugar surges, contribute to insulin resistance, and make overall diabetes management more challenging.
References
- https://diabetes.org/food-nutrition/eating-healthy/diabetes-plate-method
- https://diabetes.org/food-nutrition/eating-healthy/foods-we-eat/superstar-foods
- https://www.cdc.gov/diabetes/managing/eat-healthy.html
- Healthy Living with Diabetes – NIDDK
- Diabetes diet: Create your healthy-eating plan – Mayo Clinic
- Diabetes • The Nutrition Source
- https://www.nhs.uk/conditions/type-2-diabetes/diet/


