When it comes to identifying the “best” diabetic medications, the most effective treatment is highly personalized, depending on your specific type of diabetes, overall health, lifestyle, and co-existing conditions. There isn’t a single, universally “best” drug; instead, treatment involves a tailored approach determined in close consultation with your healthcare provider. This article will guide you through the various categories of diabetic medications available today, helping you understand their mechanisms, benefits, and the factors that influence optimal treatment decisions.
Oral Medications for Type 2 Diabetes

For many individuals living with Type 2 diabetes, oral medications are the cornerstone of their treatment plan. These pills work in various ways to help your body manage blood sugar levels more effectively, and often, a combination of these is used to achieve optimal control.
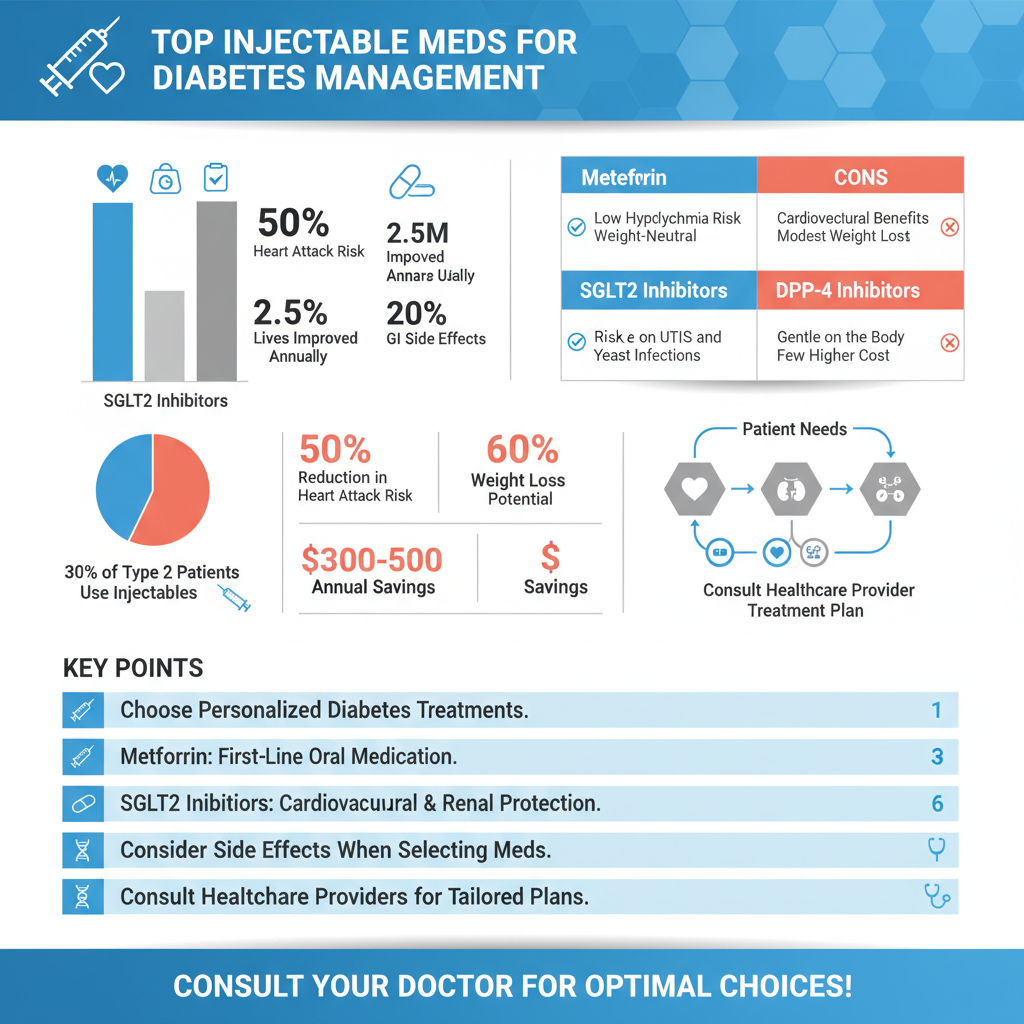
* Metformin: Often the first-line treatment for Type 2 diabetes, Metformin is a true workhorse. It primarily reduces glucose production by the liver, acting like a gentle “off switch” for excessive sugar release overnight and between meals. Beyond that, it improves the body’s sensitivity to insulin, meaning your cells can use the insulin you *do* produce more efficiently. This dual action makes it incredibly effective. Patients often appreciate that Metformin generally doesn’t cause weight gain and has a low risk of hypoglycemia (low blood sugar) when used alone. While generally well-tolerated, some individuals might experience mild gastrointestinal upset, especially when first starting the medication, which can often be mitigated by taking it with food or by using an extended-release formulation.
* SGLT2 Inhibitors (e.g., Jardiance, Farxiga): These medications represent a newer class that has truly revolutionized diabetes care due to their remarkable additional benefits. SGLT2 inhibitors work by causing the kidneys to remove more glucose from the body through urine. Think of them as helping your kidneys “flush out” excess sugar. What’s truly exciting about this class is their significant cardiovascular and renal protective benefits. Studies have shown they can reduce the risk of heart attack, stroke, hospitalization for heart failure, and slow the progression of kidney disease in people with Type 2 diabetes, even those without pre-existing heart or kidney conditions. They can also contribute to modest weight loss and a slight reduction in blood pressure, making them a fantastic option for many. Common side effects can include an increased risk of urinary tract infections or yeast infections due to the sugar in the urine.
* DPP-4 Inhibitors (e.g., Januvia, Tradjenta): If you’re looking for a medication that works gently with your body’s natural systems, DPP-4 inhibitors might be a good fit. These medications enhance the body’s natural incretin hormones. Incretins are hormones released after you eat that tell your pancreas to release more insulin when blood sugar is high and reduce the amount of glucose produced by the liver. DPP-4 inhibitors essentially “protect” these incretins, allowing them to work longer and more effectively. They primarily help lower blood sugar, especially after meals, and have a very low risk of hypoglycemia. They are generally well-tolerated, weight-neutral, and don’t typically cause the gastrointestinal side effects sometimes seen with other medications, making them a comfortable option for many.
* Sulfonylureas (e.g., Glipizide, Glimepiride): This older class of oral medications has been around for a long time and remains an effective tool for many. Sulfonylureas work by stimulating the pancreas to produce more insulin. They essentially give your pancreas a “nudge” to release more of its own insulin, which then helps lower blood glucose. While very effective at lowering blood sugar and often quite affordable, they do carry a higher risk of hypoglycemia (low blood sugar) compared to some other classes, especially if meals are skipped or delayed. They can also sometimes lead to weight gain, which is a consideration for some individuals. Careful dosing and consistent meal patterns are important when using sulfonylureas.
Injectable Medications

For some individuals, especially those with Type 1 diabetes or Type 2 diabetes that isn’t adequately controlled with oral medications, injectable treatments become a vital part of their management plan. These medications often provide powerful blood sugar lowering effects and, in some cases, offer significant additional health benefits.
* Insulin: Insulin is the lifeblood for all individuals with Type 1 diabetes, as their bodies produce little to no insulin. It’s also often necessary for Type 2 diabetes when the pancreas can no longer produce enough insulin on its own, or when oral medications are insufficient to control blood sugar. Insulin comes in various forms, each designed to mimic natural insulin patterns: rapid-acting (taken before meals to cover food), long-acting (provides a steady background level of insulin for 24 hours), and mixed insulins (a combination of rapid and intermediate-acting). Learning to administer insulin might seem daunting at first, but with proper education and support, it becomes a manageable and essential part of maintaining health and preventing complications. Your healthcare team will work closely with you to determine the right type and dose of insulin for your specific needs.
* GLP-1 Receptor Agonists (e.g., Ozempic, Trulicity): This class of injectable medications has become incredibly popular due to its multi-faceted benefits. GLP-1 receptor agonists mimic an intestinal hormone called GLP-1, which is released naturally after eating. They work by slowing digestion, helping you feel fuller for longer and reducing your appetite. They also stimulate insulin release from the pancreas *only when blood sugar is high*, significantly reducing the risk of hypoglycemia. Additionally, they reduce glucagon secretion, another hormone that raises blood sugar. Many of these medications offer substantial cardiovascular benefits, similar to SGLT2 inhibitors, and can be highly effective in aiding weight loss, which is a significant advantage for many people with Type 2 diabetes. They are typically administered once daily or once weekly, making them convenient for many lifestyles.
* Amylin Mimics (e.g., Symlin): Amylin mimics are less commonly used but play a crucial role for certain individuals. These injections are used in conjunction with insulin (for both Type 1 and Type 2 diabetes) and help manage post-meal glucose spikes. They work by slowing stomach emptying, which helps prevent blood sugar from rising too quickly after a meal. They also reduce glucagon secretion and promote satiety, helping you feel full. Because they work synergistically with insulin, they can improve overall blood sugar control and sometimes lead to a reduction in mealtime insulin doses. Symlin is administered before meals and requires careful monitoring of blood sugar levels.
Combination Therapies and Newer Approaches

The world of diabetes treatment is constantly evolving, with researchers and pharmaceutical companies always striving for more effective, convenient, and personalized solutions. This has led to exciting developments in combination therapies and innovative new approaches.
* Fixed-Dose Combination Pills: To simplify treatment regimens and improve adherence, many medications combine two or more drug classes into a single pill. For example, you might find a pill that combines Metformin with a DPP-4 inhibitor, or Metformin with an SGLT2 inhibitor. These fixed-dose combinations are designed to target different pathways involved in blood sugar regulation simultaneously, often leading to more robust blood glucose control with the convenience of fewer pills. This can be a huge benefit for patients who might otherwise need to take multiple tablets at different times of the day, making their daily routine much easier to manage.
* Newer Formulations and Deliveries: Beyond new drug classes, there’s significant innovation in how medications are delivered. We’re seeing the development of longer-acting injectables that require less frequent administration, smart insulin pens that track doses, and even efforts to create “smart” insulin pumps that automatically adjust insulin delivery based on continuous glucose monitoring. Researchers are also exploring non-injectable forms of traditionally injectable medications, such as oral GLP-1 receptor agonists. These advancements aim to reduce the burden of daily diabetes management, improve comfort, and enhance patient adherence, ultimately leading to better health outcomes.
* Personalized Medicine: The future of diabetes care is increasingly moving towards personalized medicine. This means treatment strategies are being tailored based on individual patient characteristics, such as specific genetic markers, lifestyle patterns, unique disease progression, and even the body’s microbiome. Instead of a one-size-fits-all approach, healthcare providers can use advanced diagnostics to predict which medications will be most effective for a particular individual, minimize side effects, and optimize long-term health. This individualized approach promises more targeted and effective care, moving us closer to truly bespoke diabetes management.
Key Factors in Choosing the Right Medication
Choosing the “best” diabetic medication is a shared decision between you and your healthcare team. It involves carefully weighing multiple factors to find a treatment plan that not only effectively manages your blood sugar but also fits into your life and supports your overall well-being.
* Individual Blood Glucose Control & HbA1c Goals: The primary aim of any diabetes treatment is to effectively lower blood sugar levels and achieve your individualized HbA1c goal. Your doctor will assess your current blood sugar control, including your A1c (a measure of average blood sugar over 2-3 months), and determine what level of glucose lowering is needed. Some medications offer more potent glucose reduction, while others might be chosen for their complementary benefits. Your specific targets will guide the intensity and type of medication prescribed, always with the goal of preventing long-term complications.
* Impact on Weight, Cardiovascular & Renal Health: Beyond just blood sugar, modern diabetes care looks at the bigger picture. Many people with Type 2 diabetes also face challenges with weight, and are at higher risk for cardiovascular disease (heart attack, stroke) and kidney disease. Medications that offer protective benefits for the heart and kidneys (like SGLT2 inhibitors and GLP-1 receptor agonists) or promote weight loss are incredibly valuable considerations for many patients. Discussing your personal risk factors for these conditions with your doctor is crucial in selecting a medication that offers these crucial, holistic benefits.
* Potential Side Effects and Safety Profile: Every medication comes with potential side effects, and understanding these is essential for patient safety and adherence. Some drugs might cause gastrointestinal issues, others might carry a risk of hypoglycemia, and some have specific contraindications or drug interactions. Your doctor will review your complete medical history, including any other health conditions and medications you take, to choose an option with the most favorable safety profile for you. Openly discussing any concerns or side effects you experience is vital for adjusting your treatment plan.
* Cost, Convenience, and Lifestyle: Practical considerations play a huge role in the success of any medication regimen. The cost of medication can be a significant barrier for many, and your doctor will consider what is covered by your insurance or what affordable options are available. Convenience is also key: Is it a once-daily pill or multiple injections? Does it need to be taken with food? How does it fit into your daily routine and travel plans? A medication, no matter how effective, won’t work if it’s too difficult or expensive to take consistently. Your lifestyle, preferences, and ability to adhere to the regimen are paramount to achieving long-term success.
Navigating the landscape of diabetic medications can seem complex, but understanding the different classes and how they work is the first step toward effective management. From foundational oral agents like Metformin to advanced injectable therapies and cutting-edge combination pills, each medication plays a crucial role in managing blood sugar and preventing long-term complications. Remember, the “best” diabetic medication for you is one that aligns with your individual health needs, lifestyle, and treatment goals. Always consult with your doctor or endocrinologist to discuss these options and determine the most appropriate and effective treatment plan for your personalized diabetes management journey. Your healthcare provider is your best partner in making informed decisions for a healthier future.
Frequently Asked Questions
What are the main types of medications available for managing diabetes?
The primary categories of diabetic medications include oral drugs and injectable therapies like insulin. Oral medications often prescribed for Type 2 diabetes include biguanides (e.g., Metformin), sulfonylureas, DPP-4 inhibitors, SGLT2 inhibitors, and GLP-1 receptor agonists (also available as injectables), each working through different mechanisms to lower blood glucose. Insulin therapy, which replaces or supplements the body’s natural insulin, is crucial for Type 1 diabetes and often necessary for advanced Type 2 diabetes management. The choice of *best diabetic meds* depends on individual needs and health profiles.
How do doctors determine the best diabetic medication for an individual patient?
Doctors consider several factors when selecting the *best diabetic medication*, including the patient’s type of diabetes, current A1c levels, other co-existing health conditions (like heart or kidney disease), potential side effects, and lifestyle. They also assess factors such as the patient’s ability to adhere to treatment, cost implications, and personal preferences. The goal is always to achieve optimal blood sugar control while minimizing risks and improving overall health outcomes with a personalized approach.
Are there diabetic medications that offer additional benefits beyond blood sugar control, such as weight loss or cardiovascular protection?
Yes, certain newer *diabetic medications* provide significant benefits beyond just lowering blood glucose. GLP-1 receptor agonists (e.g., Ozempic, Trulicity) are known to aid in weight loss and have shown cardiovascular benefits, reducing the risk of heart attacks and strokes. SGLT2 inhibitors (e.g., Jardiance, Farxiga) also offer remarkable cardiovascular and kidney protective effects, making them top choices for many patients with Type 2 diabetes who have or are at risk for these conditions.
What are the common side effects to be aware of with popular diabetic medications?
Common side effects vary widely among different *diabetic meds*. Metformin can cause gastrointestinal issues like nausea, diarrhea, or stomach upset, especially when first starting. Sulfonylureas are associated with a risk of hypoglycemia (low blood sugar) and weight gain. SGLT2 inhibitors may increase the risk of urinary tract infections and yeast infections, while GLP-1 receptor agonists can lead to nausea or vomiting. It’s crucial to discuss any concerns with your doctor to manage or mitigate these potential side effects effectively.
Why might a doctor change or adjust my diabetic medication regimen even if my current treatment seems to be working?
Doctors may adjust *diabetic medication* regimens for several reasons, even if current treatment appears effective. This can include the natural progression of diabetes requiring more aggressive therapy, a change in your health status (e.g., developing heart or kidney disease), or new research emerging about more effective or safer medications. Furthermore, if your A1c levels aren’t consistently at target, or you experience unacceptable side effects, your doctor might explore alternative or combination therapies to optimize your diabetes management and long-term health.
References
- Diabetes medication
- Diabetes management
- https://www.niddk.nih.gov/health-information/diabetes/overview/medication-management
- https://www.cdc.gov/diabetes/managing/medication.html
- https://diabetes.org/health-wellness/medication
- Diabetes treatment: Using insulin to manage blood sugar – Mayo Clinic
- https://my.clevelandclinic.org/health/articles/11202-diabetes-medications