When it comes to the “best” medicine for Type 2 Diabetes, there isn’t a single universal answer; instead, the most effective treatment is highly personalized. While Metformin is often the first-line therapy due to its efficacy and safety, the optimal regimen depends on an individual’s specific health profile, A1c targets, comorbidities like heart or kidney disease, potential side effects, and personal preferences. This guide will explore the primary categories of medications available to help you understand the options your healthcare provider may discuss.
The Personalized Approach to Diabetes Medication

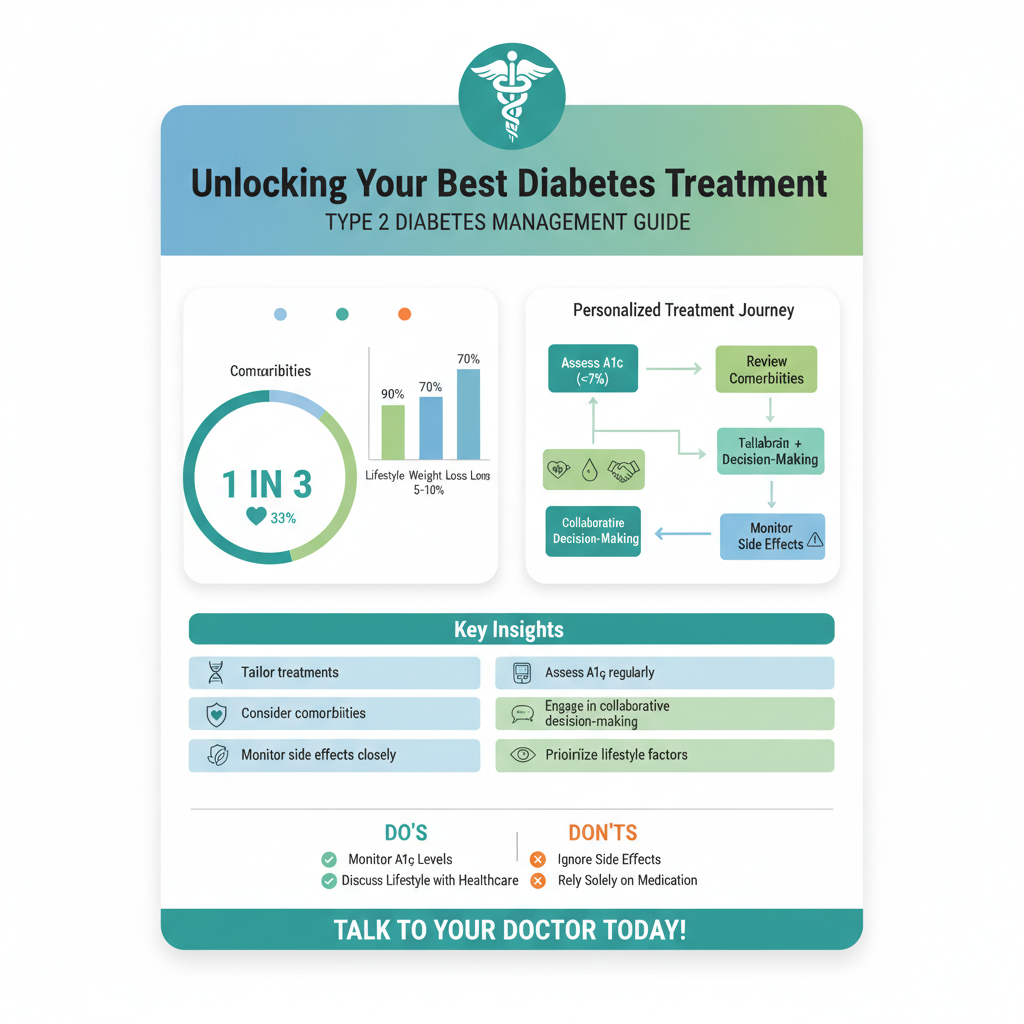
Managing Type 2 Diabetes is a deeply personal journey, and what works wonderfully for one person might not be the ideal choice for another. This is why the concept of a single “best” drug is a myth; instead, your healthcare team will craft a treatment strategy that is truly tailored to you.
* No single “best” drug; treatment strategies are tailored to the individual patient. Think of it like a custom-fitted suit rather than off-the-rack clothing. Your unique physiological responses, lifestyle, and existing health conditions all play a role in determining the most effective medication plan. This personalized approach ensures that your treatment is not just about lowering blood sugar, but about optimizing your overall health and quality of life. The goal is to manage your diabetes effectively while minimizing risks and side effects that could impact your daily routine.
* Key factors influencing medication choice include A1c levels, existing health conditions (e.g., cardiovascular disease, kidney disease), body weight, and potential side effects. Your A1c level, which reflects your average blood sugar over the past two to three months, is a primary indicator of how well your diabetes is controlled. Higher A1c levels might necessitate more potent medications or a combination therapy. Beyond that, your doctor will carefully consider any other health challenges you face. For instance, if you have a history of heart attack, stroke, or kidney disease, certain newer medications offer protective benefits for these vital organs, making them a highly attractive choice. Similarly, if you’re struggling with weight, some medications can aid in weight loss, while others might cause weight gain, influencing the decision. Your tolerance for potential side effects is also crucial; some people might experience gastrointestinal issues with one drug, while others tolerate it well.
* Collaborative decision-making with your healthcare team is crucial to find the most suitable and sustainable treatment plan. This isn’t a monologue where your doctor dictates; it’s a dialogue. Your input, concerns, lifestyle, and preferences are incredibly valuable. Be prepared to discuss your daily routines, meal patterns, exercise habits, and any anxieties you might have about injections or medication costs. An open and honest conversation with your doctor, diabetes educator, and possibly a dietitian, empowers you to be an active participant in your care. Together, you can create a sustainable plan that you understand and can confidently adhere to, which is ultimately the “best” plan for you.
Metformin: The Foundation of Type 2 Treatment

For many individuals diagnosed with Type 2 Diabetes, Metformin is often the very first medication introduced, and for good reason! It has stood the test of time as a reliable and effective cornerstone of diabetes management.
* Often prescribed as the first-line medication due to its proven efficacy, safety profile, and cost-effectiveness. Metformin has been around for decades, and its track record is incredibly strong. Clinical studies consistently show its effectiveness in lowering blood glucose levels. What makes it particularly appealing is its generally favorable safety profile, especially when compared to older agents that carried a higher risk of severe hypoglycemia. Plus, as a generic medication, it’s widely available and incredibly affordable, making it accessible to a broad range of patients. For many, it’s the sensible starting point before considering more specialized or expensive options.
* Mechanism of action: primarily works by reducing glucose production by the liver and improving the body’s sensitivity to insulin. Let’s break down how this powerhouse drug works its magic. One of the main culprits in Type 2 Diabetes is an overactive liver, which produces too much glucose (sugar) even when it’s not needed. Metformin steps in to gently tell the liver to slow down this production, especially at night. Secondly, a common problem in Type 2 Diabetes is insulin resistance, where your body’s cells don’t respond effectively to the insulin your pancreas produces. Metformin helps to improve this sensitivity, allowing your own insulin to work more efficiently, pulling glucose out of your bloodstream and into your cells where it can be used for energy. This dual action makes it very effective at controlling blood sugar.
* Benefits include modest weight loss potential and a low risk of hypoglycemia (low blood sugar) when used alone. Unlike some other diabetes medications that can lead to weight gain, Metformin often has the pleasant side effect of modest weight loss or at least weight neutrality, which is a big plus for many with Type 2 Diabetes. Additionally, because Metformin doesn’t directly stimulate the pancreas to release more insulin (which can sometimes lead to too much insulin and a crash in blood sugar), it carries a very low risk of causing hypoglycemia when taken by itself. This makes it a safer option for many, though it’s still important to monitor your blood sugar regularly. Some common initial side effects can include gastrointestinal upset like nausea or diarrhea, but these often improve over time, especially when the medication is taken with food or slowly titrated up to the full dose.
Newer Medications: Beyond Metformin

While Metformin remains a fantastic starting point, the field of diabetes treatment has seen incredible advancements in recent years. Newer classes of medications offer additional benefits, particularly for cardiovascular and kidney health, making them vital tools in a comprehensive treatment plan.
* GLP-1 Receptor Agonists (e.g., Ozempic, Trulicity): These medications represent a significant leap forward in diabetes care. Primarily administered as injectables (though an oral form, Rybelsus, is also available), GLP-1 RAs work by mimicking a natural hormone called glucagon-like peptide-1. This action has several powerful effects: they promote the release of insulin only when blood sugar levels are high, slow down gastric emptying (which helps you feel fuller longer and reduces post-meal blood sugar spikes), and suppress glucagon production (another hormone that raises blood sugar). The “cherry on top” is their often significant ability to lead to weight loss, which is a major benefit for many with Type 2 Diabetes. Crucially, many GLP-1 RAs have also demonstrated remarkable cardiovascular benefits, reducing the risk of heart attack, stroke, and cardiovascular death in people with established heart disease or high cardiovascular risk. This makes them a strong contender for patients needing both blood sugar control and heart protection.
* SGLT2 Inhibitors (e.g., Farxiga, Jardiance): These oral medications have revolutionized how we think about diabetes treatment due to their incredible organ-protective qualities. SGLT2 inhibitors work in a unique way: they block a protein in your kidneys called SGLT2, which is responsible for reabsorbing glucose back into your bloodstream. By blocking this protein, these drugs cause your kidneys to excrete more glucose (sugar) in your urine, effectively lowering blood sugar levels. Beyond glucose control, the most exciting aspect of SGLT2 inhibitors is their proven ability to protect the heart and kidneys. They significantly reduce the risk of heart failure hospitalizations, slow the progression of chronic kidney disease, and can even lower the risk of cardiovascular events in certain high-risk individuals. They also contribute to modest weight loss and a slight reduction in blood pressure. While generally well-tolerated, potential side effects can include an increased risk of urinary tract infections and yeast infections due to the sugar in the urine.
* DPP-4 Inhibitors (e.g., Januvia, Tradjenta): DPP-4 inhibitors are another class of oral medications that work by enhancing the body’s natural incretin hormones, similar to GLP-1 RAs, but with a different mechanism of action and generally milder effects. They prevent the breakdown of GLP-1 and GIP (another incretin hormone) that your body naturally produces, allowing these hormones to work longer. This leads to increased insulin release when blood sugar is high and reduced glucose production by the liver. DPP-4 inhibitors are generally very well-tolerated, are weight-neutral (they don’t cause weight gain or loss), and carry a very low risk of hypoglycemia when used alone. While they don’t offer the same dramatic weight loss or cardiovascular benefits as GLP-1 RAs or SGLT2 inhibitors, they are excellent options for steady, reliable blood sugar control, especially when used in combination with other drugs, or for patients who need a gentle yet effective treatment without significant side effects.
Other Established Oral Medications
While newer medications often garner a lot of attention, several established oral medications continue to play an important role in diabetes management, particularly for certain patient profiles or when used in combination therapies.
* Sulfonylureas (e.g., Glipizide, Glyburide): These older but still effective medications work by stimulating the beta cells in your pancreas to produce and release more insulin. They are very potent at lowering blood sugar, and for many years, they were a go-to option after Metformin. However, their mechanism of action means they can sometimes cause the pancreas to release *too much* insulin, leading to a higher risk of hypoglycemia (low blood sugar), which can be dangerous. They also tend to be associated with potential weight gain. Because of these side effects, and the advent of newer drugs with additional benefits, sulfonylureas are often considered when cost is a significant factor, or when other medications are not suitable. Careful monitoring and patient education are key when using this class of drugs.
* Thiazolidinediones (TZDs – e.g., Actos, Avandia): TZDs improve insulin sensitivity in muscle and fat cells, making your body’s own insulin work more effectively. This addresses a core problem in Type 2 Diabetes – insulin resistance. They are effective at lowering blood sugar over time and have a low risk of hypoglycemia when used alone. However, TZDs can be associated with weight gain and fluid retention, which can be problematic, especially for individuals with heart failure. Avandia (rosiglitazone) also faced concerns about cardiovascular safety, leading to restrictions on its use, though these restrictions have largely been lifted. Actos (pioglitazone) is more commonly used today and has even shown some potential cardiovascular benefits in specific patient populations. Despite their efficacy in improving insulin sensitivity, their side effect profile means they are often reserved for specific situations or as part of a combination therapy.
Injectable Therapies: Beyond GLP-1
While many people prefer oral medications, injectable therapies are indispensable for many individuals with Type 2 Diabetes, especially as the disease progresses or when specific therapeutic goals are paramount.
* Insulin Therapy: Insulin is a hormone naturally produced by the pancreas, essential for regulating blood sugar. In Type 2 Diabetes, the body initially develops insulin resistance, and over time, the pancreas may struggle to produce enough insulin to overcome this resistance or to meet the body’s needs. When oral medications and other injectables are no longer sufficient to achieve blood sugar targets, or in specific situations like severe illness or pregnancy, insulin therapy becomes essential. It directly replaces or supplements the insulin your body can’t produce. Insulin comes in various forms, categorized by how quickly they act and how long their effects last (e.g., rapid-acting taken before meals, long-acting/basal insulin taken once or twice a day to provide a steady background level). While the idea of injections can be daunting, modern insulin pens are designed to be user-friendly and make the process as comfortable as possible. Learning how to properly administer insulin and monitor your blood sugar is a vital part of its effective use.
* Amylin Mimetics (e.g., Symlin): This is a less commonly used injectable medication, but it plays a valuable role in specific scenarios. Amylin mimetics, specifically pramlintide (Symlin), are typically used in conjunction with insulin, often for people who are already on insulin but struggle to achieve their post-meal blood sugar targets. Amylin is a hormone that is co-secreted with insulin from the pancreas, and in diabetes, its production is often deficient. Pramlintide mimics the action of natural amylin by slowing gastric emptying (which prevents rapid spikes in blood sugar after meals), suppressing glucagon secretion (which prevents the liver from releasing too much glucose), and promoting a feeling of satiety, which can help with weight management. It’s usually injected before meals and can significantly improve post-meal glucose control and reduce overall insulin needs, though it does carry a risk of hypoglycemia, especially when first started with insulin.
Combination Therapy and Future Outlook
As Type 2 Diabetes is a progressive condition, it’s very common for treatment plans to evolve over time. What starts as one medication often progresses to two, three, or even a combination of oral and injectable therapies.
* Many individuals with Type 2 Diabetes eventually require a combination of medications to achieve and maintain their A1c targets, utilizing drugs with different mechanisms of action. This is not a sign of failure, but rather a natural progression of the disease and a smart strategy. Using medications that work in different ways creates a synergistic effect, targeting various aspects of diabetes pathophysiology more comprehensively. For instance, pairing Metformin (which reduces liver glucose production and improves insulin sensitivity) with an SGLT2 inhibitor (which promotes glucose excretion) can lead to more robust blood sugar control and offer additional organ protection than either drug alone. This multi-pronged approach helps to sustain blood sugar levels within the target range for longer, protecting against long-term complications. Your healthcare provider will often start with one medication and add others as needed to keep your A1c in check.
* Treatment regimens are continuously refined to address individual patient needs, manage comorbidities, and minimize the risk of long-term complications. The landscape of diabetes care is dynamic. Your doctor will regularly review your A1c, blood pressure, cholesterol levels, kidney function, and overall health to ensure your treatment plan remains optimal. If your blood sugar starts to creep up, or if new health issues arise (like developing early signs of kidney disease), your medication regimen will likely be adjusted. The overarching goal is not just to lower your blood sugar numbers, but to prevent the devastating long-term complications of diabetes, such as heart disease, stroke, kidney failure, nerve damage, and vision loss. The modern approach focuses on personalized risk reduction.
* Ongoing research is focused on developing even more effective, convenient, and targeted treatments for diabetes management. The future of diabetes treatment is incredibly promising! Scientists are constantly working on new drug classes, improved formulations (like weekly oral medications), and even potential cures. Research includes exploring novel targets beyond glucose metabolism, developing “smart” insulins that respond to blood sugar levels, and refining technologies for glucose monitoring and insulin delivery (e.g., artificial pancreas systems). This continuous innovation means that people living with Type 2 Diabetes can look forward to even more sophisticated, easier-to-use, and more effective options for managing their condition and living full, healthy lives.
Choosing the “best” diabetes type 2 medicine is a highly individualized process that involves carefully considering your unique health profile, lifestyle, and treatment goals. While Metformin often serves as the cornerstone, a diverse array of newer and established medications offers significant benefits, especially in preventing complications like heart and kidney disease. The most crucial step is to engage in an open dialogue with your healthcare provider to discuss all available options, understand their benefits and risks, and collaboratively develop a personalized treatment plan that is right for you. Regular monitoring and adherence to your prescribed regimen, combined with healthy lifestyle choices, are key to effectively managing Type 2 Diabetes and improving your overall well-being.
Frequently Asked Questions
Is there a single “best” medicine for type 2 diabetes?
No, there isn’t one universal “best” medicine for type 2 diabetes; treatment is highly individualized. The most effective diabetes management plan depends on various factors, including your specific health profile, current blood sugar levels, other medical conditions, potential side effects, and personal preferences. Your doctor will work with you to find the optimal medication or combination of medications to achieve your target blood sugar control.
How do doctors choose the most effective type 2 diabetes medication for an individual?
Doctors determine the most effective type 2 diabetes medication by considering several key factors, including the patient’s A1C level, kidney function, cardiovascular health, risk of hypoglycemia, and potential impact on weight. They also evaluate co-existing conditions, such as heart failure or chronic kidney disease, as some medications offer protective benefits beyond blood sugar control. The goal is to create a personalized treatment plan that effectively manages blood glucose while minimizing adverse effects and improving overall health.
What are the main categories of oral medications for type 2 diabetes?
The main categories of oral medications for type 2 diabetes include biguanides (like metformin), sulfonylureas, glinides, DPP-4 inhibitors, SGLT2 inhibitors, thiazolidinediones (TZDs), and alpha-glucosidase inhibitors. Each class works differently to lower blood sugar: for example, metformin reduces glucose production in the liver, while SGLT2 inhibitors help the kidneys remove glucose through urine. Often, a combination of these oral medicines is prescribed to achieve optimal glycemic control.
Which type 2 diabetes medications can help with weight management?
Several type 2 diabetes medications offer benefits for weight management, which can be crucial for many patients living with the condition. GLP-1 receptor agonists (such as Ozempic, Trulicity, Wegovy) and SGLT2 inhibitors (like Farxiga, Jardiance) are notable for often leading to weight loss in addition to effectively lowering blood sugar. These drug classes can help improve metabolic health and are frequently considered for individuals with type 2 diabetes who are also struggling with excess weight.
Why might my diabetes type 2 medication change over time?
Your diabetes type 2 medication plan might change over time because type 2 diabetes is a progressive condition, meaning the body’s ability to produce or use insulin can gradually decline further. Factors like changes in your A1C levels, the development of new health conditions, experiencing side effects, or the emergence of newer, more effective treatment options can all necessitate adjustments. Regular monitoring and open communication with your healthcare provider are essential to ensure your diabetes treatment remains optimal and responsive to your evolving needs.
References
- https://www.niddk.nih.gov/health-information/diabetes/overview/type-2-diabetes/medicines-type-2-diabetes
- https://www.cdc.gov/diabetes/basics/type2.html
- https://diabetes.org/healthy-living/medication-treatments/type-2-medicines
- Type 2 diabetes – Diagnosis and treatment – Mayo Clinic
- https://en.wikipedia.org/wiki/Management_of_diabetes_mellitus_type_2
- https://www.nih.gov/news-events/news-releases/nih-funded-study-finds-certain-diabetes-drugs-superior-others-protecting-heart-kidneys
- https://medlineplus.gov/type2diabetes.html