The best fruits for diabetics are those with a low glycemic index and high fiber content, specifically berries, tart cherries, apples, and citrus fruits like grapefruit. These options allow you to satisfy a sweet craving without causing rapid spikes in blood glucose levels. Incorporating these nutrient-dense fruits into your diet helps manage diabetes effectively while providing essential vitamins and antioxidants. For individuals managing diabetes, fruit is not forbidden; rather, it is a strategic component of a balanced diet that requires careful selection and portion control. By prioritizing fruits that release glucose slowly into the bloodstream, patients can maintain glycemic stability while benefiting from the cardioprotective and anti-inflammatory properties found in fresh produce.
1. Berries: The Top Superfood Choice

When analyzing the nutritional landscape for diabetes management, berries—including strawberries, blueberries, raspberries, and blackberries—consistently rank as the superior choice. This distinction is due to their exceptionally low glycemic load and high concentration of polyphenols, particularly anthocyanins. These compounds are known to improve insulin sensitivity and reduce systemic inflammation, a common comorbidity in Type 2 diabetes. Unlike denser fruits that pack a significant carbohydrate load in a small volume, berries consist largely of water and fiber, allowing for a generous serving size with minimal metabolic impact.
From a glycemic perspective, raspberries and blackberries are particularly notable because they contain the highest fiber-to-carbohydrate ratio of common fruits. Fiber is the critical macronutrient for diabetics as it passes through the digestive system undigested, effectively blunting the spike in blood sugar that typically accompanies carbohydrate consumption. Furthermore, the antioxidants found in berries help combat oxidative stress, which is often elevated in diabetic patients and contributes to vascular complications.
Regarding portion sizes, berries offer a distinct psychological advantage. While a diabetic might be restricted to half a banana, a standard serving of berries is typically one full cup (approx. 150 grams). This volume provides a visually satisfying snack that feels substantial. For optimal blood sugar management, it is recommended to consume fresh or frozen berries without added sugars. If purchasing frozen varieties, careful label reading is essential to ensure they are not packed in sweetened syrup.
2. Tart Cherries and Stone Fruits
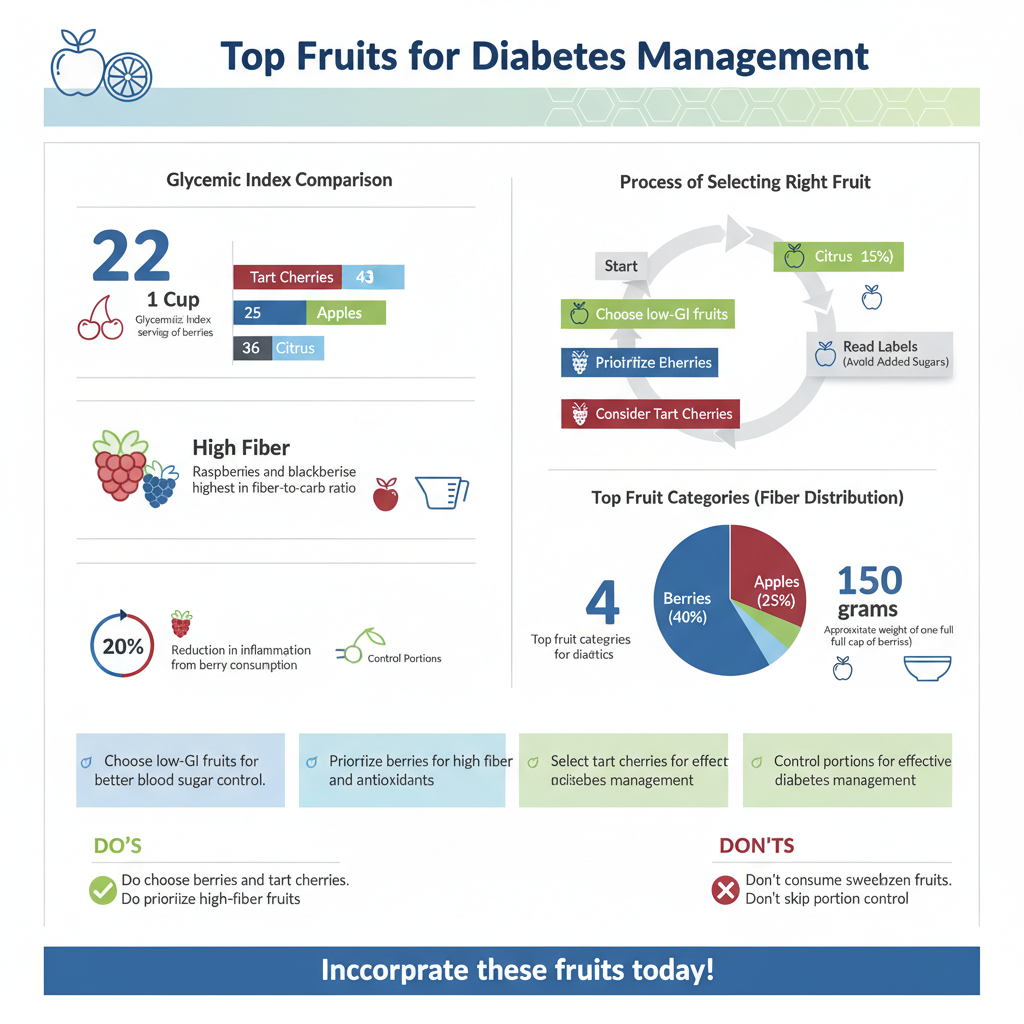

Stone fruits—fleshy fruits containing a pit, such as cherries, peaches, plums, and apricots—are excellent additions to a diabetic meal plan when chosen correctly. Tart cherries, in particular, deserve specific attention. Unlike their sweeter counterparts (such as Rainiers), tart cherries possess a very low glycemic index (GI), often scoring around 22 on the GI scale. This is significantly lower than many other fruits. Beyond their low sugar impact, tart cherries are rich in anti-inflammatory compounds that may help alleviate joint pain and reduce markers of inflammation associated with insulin resistance.
Peaches, plums, and nectarines are also viable options, provided they are consumed in their fresh, whole state. These fruits provide a good source of vitamins A and C, as well as potassium. However, the method of preservation is a critical variable. Fresh stone fruits contain water and fiber that moderate sugar absorption. Conversely, canned versions are frequently processed in heavy or light syrup, which essentially bathes the fruit in concentrated sugar water.
Even stone fruits canned in “fruit juice” can pose a risk, as the juice itself lacks fiber and raises the total carbohydrate count of the serving. Therefore, the professional recommendation is to consume these fruits fresh during their peak season. If fresh options are unavailable, one should opt for frozen stone fruits or canned varieties packed exclusively in water, ensuring any excess liquid is drained before consumption to minimize incidental sugar intake.
3. Citrus Fruits for Vitamin C and Fiber

Citrus fruits, including grapefruit, oranges, and pomelos, are powerhouses of nutrition that play a supportive role in diabetes care. The primary benefit of citrus lies in its high soluble fiber content. Unlike insoluble fiber, soluble fiber dissolves in water to form a gel-like substance in the gastrointestinal tract. This process slows gastric emptying and the absorption of glucose into the bloodstream, leading to a more gradual rise in blood sugar levels rather than a sharp spike.
Grapefruit is frequently cited in diabetic nutrition guidelines due to its association with improved insulin resistance and weight management. However, a professional note of caution is necessary: grapefruit contains furanocoumarins, compounds that can interact with certain medications, including statins and blood pressure drugs often prescribed to diabetics. Patients should always consult their healthcare provider before making grapefruit a dietary staple.
A crucial distinction must be made between whole citrus fruit and fruit juice. While a whole orange is a diabetic-friendly snack (GI score approx. 40), a glass of orange juice is a concentrated source of sugar with the beneficial fiber removed. Without the fiber matrix to slow digestion, juice causes rapid glucose absorption, mimicking the metabolic effect of sugary sodas. For this reason, professional dietary guidelines universally recommend eating the fruit rather than drinking the juice to maximize satiety and glycemic control.
4. Apples and Pears: Eat the Skin
Apples and pears represent the “staple” fruits of a balanced diabetic diet due to their availability, portability, and nutrient profile. However, the way these fruits are consumed significantly alters their health value. The majority of the fiber, specifically pectin, and a significant portion of the antioxidants are located in or just below the skin. Peeling an apple or pear removes nearly half of its total fiber content, transforming a slow-digesting carbohydrate source into one that raises blood sugar more rapidly.
Pectin is particularly beneficial for diabetics because it improves gut health and has been shown to modestly lower LDL cholesterol levels—a vital consideration given that diabetes increases the risk of cardiovascular disease. The texture of the skin also requires more chewing, which slows down the rate of ingestion and increases satiety signals to the brain, preventing overeating.
Portion control remains a key strategy with these fruits. Modern agriculture has bred apples and pears to be significantly larger than they were in previous decades. A large apple found in a supermarket today can contain upwards of 30 grams of carbohydrates, equivalent to two slices of bread. To naturally control carbohydrate intake per serving, it is advisable to select smaller-sized fruits (roughly the size of a tennis ball) or to weigh the fruit to ensure the carbohydrate load fits within your specific meal plan targets.
5. Fruits to Limit or Avoid
While no fruit is inherently “bad,” certain varieties possess a high glycemic index or glycemic load that can make blood sugar management difficult. Tropical fruits such as pineapples, mangoes, papayas, and melons (cantaloupe and watermelon) generally contain higher natural sugar concentrations and less fiber than temperate fruits like berries or apples. For example, a very ripe banana has a high GI because as it ripens, its resistant starch converts almost entirely into simple sugars, leading to rapid absorption.
Dried fruits represent a concentrated source of carbohydrates that diabetics should approach with extreme caution or avoid. When water is removed from fruit like grapes (to make raisins) or dates, the sugar content becomes dense. A small handful of raisins contains the same amount of carbohydrates as a large bowl of fresh grapes but lacks the volume to provide satiety. Consequently, it is very easy to overconsume carbohydrates when eating dried fruit.
Furthermore, processed fruit snacks, fruit leathers, and “gummies” marketed as being made with real fruit should generally be avoided. these products are essentially candy; the fiber is destroyed during processing, and they often contain added high-fructose corn syrup or cane sugar. The rapid spike in glucose caused by these processed items can lead to hyperglycemia, followed by a hypoglycemic crash, creating a roller-coaster effect on energy and mood.
6. Pairing Fruit with Protein
To maximize glycemic control, the “how” of eating fruit is just as important as the “what.” A highly effective professional strategy is to never consume fruit on a completely empty stomach (“naked carbs”). Instead, fruit should be paired with a source of healthy fat or protein. This combination is often referred to in nutritional counseling as “clothing your carbs.”
When carbohydrates are eaten alone, they are digested relatively quickly. However, when paired with protein (like Greek yogurt or cheese) or healthy fats (like walnuts, almonds, or avocado), the digestive process changes. Fat and protein take longer to digest, which delays gastric emptying. This means the sugars from the fruit enter the bloodstream at a much slower, more manageable rate, resulting in a flatter glucose curve rather than a sharp peak.
For example, pairing a sliced apple with a tablespoon of natural peanut butter, or adding a cup of berries to plain, high-protein Greek yogurt, transforms a simple snack into a balanced mini-meal. This strategy not only stabilizes blood sugar but also increases satiety, keeping hunger at bay for longer periods. This approach is fundamental to modern diabetic medical nutrition therapy, moving away from strict elimination and toward strategic food combining.
Incorporating fruit into a diabetic diet is not only possible but beneficial when you focus on low-glycemic, fiber-rich options like berries and apples. By making informed choices about the types of fruit you consume, emphasizing whole fresh produce over juices or dried varieties, and employing strategic pairing with proteins, you can enjoy the sweetness of nature without compromising your health. Remember to monitor your portion sizes and pair your fruit with protein to maintain stable blood sugar levels throughout the day. Consult with your dietitian to create a meal plan tailored to your specific health needs.
Frequently Asked Questions
Which fruits have the lowest glycemic index for diabetics?
Berries, including strawberries, blueberries, and raspberries, are among the best choices because they have a very low glycemic index (GI) and are packed with fiber and antioxidants. Tart cherries, citrus fruits like grapefruit, and firm fruits like apples and pears are also excellent options that release sugar slowly into the bloodstream. Choosing these low-GI foods helps satisfy sweet cravings without causing sharp glucose spikes, making them safe staples for a diabetic diet.
Can people with type 2 diabetes eat bananas and grapes?
Yes, diabetics can eat higher-sugar fruits like bananas and grapes, provided they practice strict portion control and monitor their total carbohydrate intake. To minimize blood sugar impact, it is best to pair these fruits with a source of protein or healthy fat, such as a handful of nuts or Greek yogurt, which slows down digestion. Additionally, choosing a slightly green banana over a fully ripe one can reduce the sugar load due to higher levels of resistant starch.
How many servings of fruit can a diabetic have per day?
Most health guidelines suggest that people with diabetes can safely consume two to three servings of fresh fruit per day as part of a balanced meal plan. A single serving is typically defined as one small whole piece of fruit (like an apple or orange) or about half a cup of sliced fruit or berries. However, individual carbohydrate tolerance varies, so testing your blood sugar levels two hours after eating is the most effective way to determine your personal limit.
Why are whole fruits better than fruit juice or dried fruit for diabetes management?
Fruit juice and dried fruits contain concentrated sugar and typically lack the essential dietary fiber found in whole, fresh fruit, leading to much faster and higher blood glucose spikes. Without the fiber to slow down digestion, the sugar enters the bloodstream rapidly, and the smaller volume of dried fruit makes it easy to accidentally overeat carbohydrates. Experts generally recommend choosing fresh or frozen whole fruit to ensure you feel full and maintain stable sugar levels.
What is the best way to eat fruit to prevent blood sugar spikes?
The most effective strategy is to never eat fruit alone on an empty stomach; instead, pair it with protein or healthy fats to buffer the absorption of fructose. For example, eating apple slices with peanut butter or berries with cottage cheese significantly reduces the rate at which glucose enters the bloodstream. Additionally, spreading fruit intake throughout the day rather than consuming all daily servings at one meal helps keep blood sugar levels consistent.
References
- https://health.clevelandclinic.org/best-fruits-for-diabetes
- Diabetes diet: Should I avoid sweet fruits? – Mayo Clinic
- Fruit, vegetables and diabetes | Eating with diabetes | Diabetes UK
- Healthy Living with Diabetes – NIDDK
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/diabetes-and-fruit
- Diabetes Teaching Center
- Healthy Eating | Diabetes | CDC


