When searching for the “best medicine for diabetes without side effects,” it’s important to understand that no medication is entirely free of potential side effects. However, many excellent diabetes medications exist today that are well-tolerated, have minimal or manageable side effects, and significantly improve health outcomes. The “best” approach often involves a combination of lifestyle changes and carefully chosen medications tailored to your individual needs and health profile. This guide explores options known for their favorable side effect profiles and how to find the right treatment plan for you.
Understanding “Minimal Side Effects” in Diabetes Medication

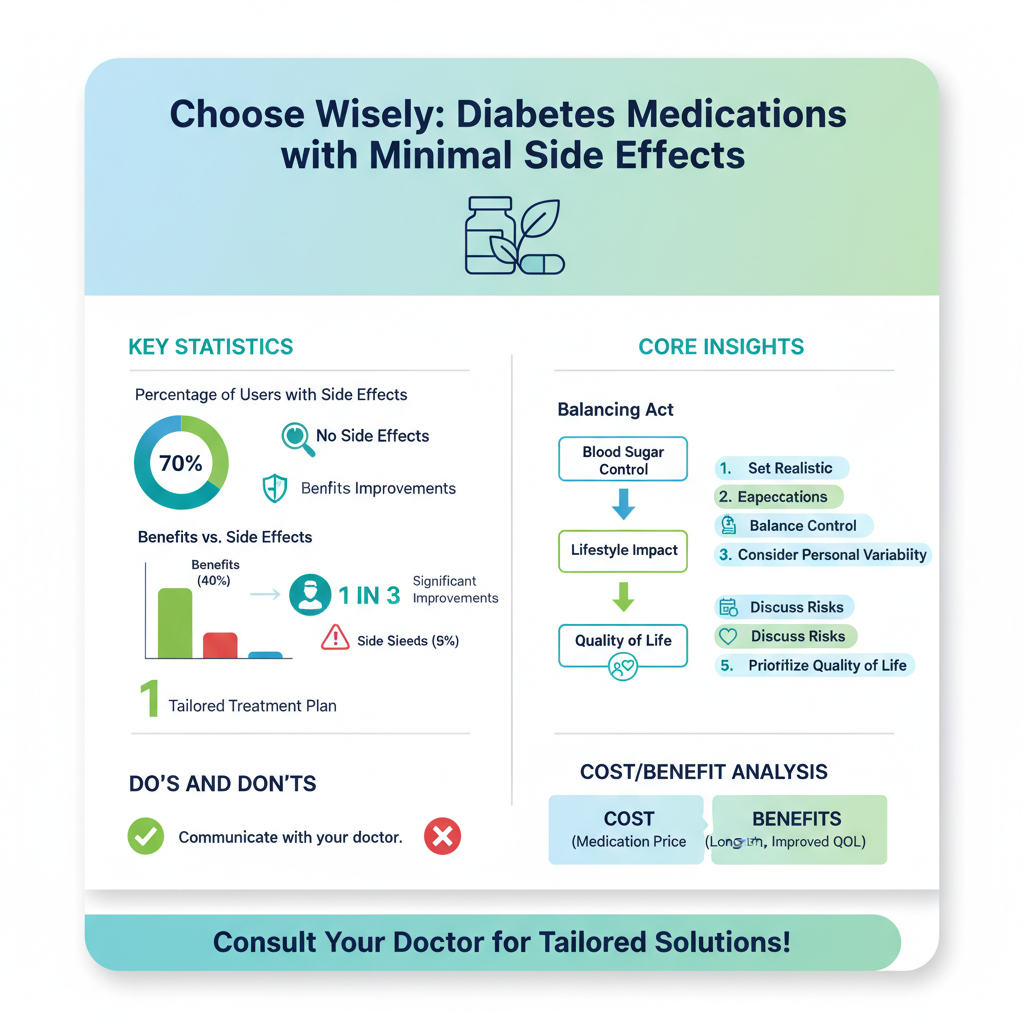
It’s completely natural to want a magic bullet for any health condition, especially one as persistent as diabetes, that comes without any downsides. When we talk about finding a “best medicine for diabetes without side effects,” it’s essential to set realistic expectations.
* Realistic Expectations: In the realm of medicine, the term “without side effects” is almost always a wish rather than a reality. Every medication, no matter how mild, carries potential risks and benefits. When healthcare professionals and patients discuss medications with “minimal side effects,” what we usually mean are treatments where any side effects are rare, mild, easily managed, or, most importantly, significantly outweighed by the substantial health benefits they provide. The goal isn’t absolute freedom from any potential issue, but rather finding a treatment that offers excellent control over your blood sugar while having the least disruptive impact on your daily life. Think of it as finding the gentlest yet most effective way to help your body.
* Balancing Act: The core objective of diabetes treatment is a delicate balancing act. On one side, we aim to achieve optimal blood sugar control to prevent or delay severe long-term complications like heart disease, kidney damage, nerve damage, and vision loss. On the other side, we want to minimize any adverse effects that could negatively impact your quality of life, comfort, or overall health. Your doctor’s job, and yours, is to weigh these factors carefully, ensuring that the chosen treatment path improves your health without introducing unnecessary burdens. This often involves discussing potential risks openly and understanding how to recognize and manage them if they arise.
* Personal Variability: One of the most fascinating and sometimes challenging aspects of medicine is how differently individuals can respond to the same treatment. What causes a bothersome side effect in one person might be perfectly tolerated by another. Factors like your genetic makeup, age, overall health status, other medications you’re taking, and even your lifestyle habits can all influence how your body reacts to a particular diabetes medicine. This personal variability underscores why a “one-size-fits-all” approach simply doesn’t work for diabetes management. It highlights the critical need for personalized care, where your unique physiology and circumstances guide the treatment choices.
Lifestyle: The Foundation of Diabetes Management

Before even considering medication, it’s crucial to understand that lifestyle modifications are not just helpful; they are often the most powerful “medicine” you have at your disposal. They form the unbreakable foundation upon which all other diabetes treatments are built, offering profound benefits with absolutely no pharmacological side effects.
* Dietary Changes: Adopting a balanced, low-glycemic diet is paramount in managing diabetes. This isn’t about deprivation, but rather a shift towards nutrient-dense whole foods. Focus on increasing your intake of fiber-rich vegetables, fruits (in moderation), lean proteins (like chicken, fish, beans, lentils), and healthy fats (avocado, nuts, olive oil). Minimizing processed foods, sugary drinks, and refined carbohydrates can dramatically stabilize blood sugar levels, reduce insulin resistance, and often lead to healthy weight loss. These changes can significantly improve your blood sugar control, potentially reducing the need for higher medication dosages or even delaying the need for medication in some cases of prediabetes or early Type 2 diabetes. Think of food as medicine – powerful, effective, and delicious!
* Regular Physical Activity: Moving your body regularly is a cornerstone of diabetes management. Consistent exercise, whether it’s brisk walking, swimming, cycling, dancing, or strength training, helps your body in multiple ways. It improves insulin sensitivity, meaning your cells become more responsive to the insulin your body produces, allowing glucose to enter cells more efficiently and lowering blood glucose levels. Physical activity also aids in weight management, strengthens your cardiovascular system, and boosts your mood. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, plus strength training a couple of times a week. Even small, consistent efforts can make a big difference in reducing your medication reliance and improving overall health.
* Stress Management & Sleep: We often overlook the profound impact of stress and sleep on our metabolic health. Chronic stress triggers the release of hormones like cortisol, which can elevate blood sugar levels and increase insulin resistance. Finding effective ways to manage stress—whether through mindfulness, meditation, yoga, spending time in nature, or engaging in hobbies—can directly support better blood sugar control. Similarly, adequate and quality sleep is vital. Poor sleep can disrupt hormone balance, leading to increased insulin resistance and higher blood glucose levels. Aim for 7-9 hours of restful sleep per night by establishing a regular sleep schedule, creating a comfortable sleep environment, and avoiding screens before bedtime. Prioritizing stress reduction and good sleep is an indirect yet incredibly powerful way to support your diabetes management and enhance the effectiveness of any medications you might be taking.
Oral Medications with Favorable Side Effect Profiles

For many living with Type 2 diabetes, oral medications are a key part of their treatment plan. Several options stand out for their effectiveness and generally favorable side effect profiles.
* Metformin: Often hailed as the first-line treatment for Type 2 diabetes, Metformin is a true workhorse. It’s incredibly effective, widely available, and usually quite affordable. Metformin primarily works by reducing the amount of glucose your liver produces and improving your body’s sensitivity to insulin, helping your cells take up glucose more effectively. The most common side effects are gastrointestinal in nature, such as nausea, diarrhea, or stomach upset. The good news is that these often diminish over time as your body adjusts, especially if you start with a low dose and gradually increase it, or take it with food. Many people find these side effects manageable, and the long-term benefits of Metformin, including its potential for cardiovascular protection and modest weight loss, make it an invaluable tool in diabetes care.
* DPP-4 Inhibitors (Gliptins): Medications like sitagliptin (Januvia), linagliptin (Tradjenta), saxagliptin (Onglyza), and alogliptin (Nesina) belong to a class called DPP-4 inhibitors. These medications work by helping your body’s natural incretin hormones (which help release insulin after meals and reduce liver glucose production) last longer. They are known for their gentle approach to blood sugar control, offering a low risk of hypoglycemia ( dangerously low blood sugar) because they only stimulate insulin release when blood sugar levels are high. They are also typically weight-neutral, meaning they don’t cause weight gain, and are generally very well-tolerated. Common side effects are rare and usually mild, possibly including a headache or joint pain, making them a good option for many.
* SGLT2 Inhibitors (Flozins): Medications such as empagliflozin (Jardiance), canagliflozin (Invokana), dapagliflozin (Farxiga), and ertugliflozin (Steglatro) are part of the SGLT2 inhibitor class. These work in a unique way: they help your kidneys remove excess glucose from your body through your urine. While this mechanism can increase the risk of genitourinary infections, such as urinary tract infections (UTIs) or yeast infections (because of the sugar in the urine), these side effects are often manageable with good hygiene and prompt treatment. What makes SGLT2 inhibitors particularly exciting is their significant benefits beyond just lowering blood glucose. They have been shown to provide remarkable cardiovascular protection, reducing the risk of heart attack, stroke, and heart failure hospitalization, and also offer kidney protection, slowing the progression of kidney disease. For many, these profound protective benefits far outweigh the manageable risk of mild infections, making them a powerful choice in comprehensive diabetes management.
Injectable Therapies Beyond Insulin with Manageable Effects
Beyond oral pills, there are highly effective injectable medications that are not insulin but offer significant benefits for diabetes management, often with very manageable side effect profiles.
* GLP-1 Receptor Agonists: This class includes medications like liraglutide (Victoza), semaglutide (Ozempic, Rybelsus – which is an oral form), dulaglutide (Trulicity), and exenatide (Byetta, Bydureon BCise). GLP-1 receptor agonists mimic the action of a natural hormone in your body that helps regulate blood sugar. They work by stimulating insulin release when blood sugar is high, reducing the amount of glucose your liver produces, slowing down digestion (which helps you feel fuller longer), and promoting a feeling of satiety. This often leads to significant blood sugar control, notable weight loss, and, importantly, proven cardiovascular benefits. Common side effects are usually gastrointestinal, such as nausea, vomiting, or diarrhea, particularly when starting the medication or increasing the dose. However, these effects tend to improve significantly over time as your body adjusts. With options for daily or once-weekly injections (and even an oral pill!), GLP-1 agonists have become a game-changer for many individuals looking for potent control with added health advantages.
* Tailored Approach: The decision to use an injectable therapy beyond insulin is a highly personalized one. For some individuals, the benefits offered by GLP-1 receptor agonists – such as superior blood sugar control, considerable weight loss, and crucial cardiovascular protection – might make their side effect profile entirely acceptable, especially if the side effects are mild and transient. For instance, if you have significant weight to lose, or if you have existing cardiovascular disease or are at high risk, your doctor might recommend a GLP-1 agonist due to its protective effects, despite the potential for initial nausea. It’s about weighing the specific advantages for your individual health profile against any potential discomfort, always in close consultation with your healthcare provider.
The Importance of Personalized Diabetes Care
In diabetes management, there is no universal “best” medicine. What works wonderfully for one person might not be the right fit for another. This is where personalized care truly shines.
* Individualized Treatment Plans: Your diabetes treatment plan should be as unique as you are. Crafting the “best” medicine strategy involves a careful consideration of many factors. Your doctor will look at your specific type of diabetes (Type 1, Type 2, LADA, etc.), how long you’ve had it, your current A1c levels, and your overall health. They’ll also consider any co-existing medical conditions you might have, such as heart disease, kidney disease, high blood pressure, or obesity, as some medications offer benefits for these conditions too. Your lifestyle, personal preferences (e.g., preference for pills over injections, or a desire to avoid weight gain), your ability to afford medications, and even your cultural background can all play a role in finding the most suitable and sustainable treatment path for you.
* Collaboration with Your Healthcare Team: You are the most important member of your diabetes care team! Working closely with a multidisciplinary group of experts is absolutely crucial. This team often includes your primary care physician, an endocrinologist (a specialist in hormones and diabetes), a registered dietitian (to help with dietary changes), a certified diabetes educator (who can provide practical advice on medication use, monitoring, and lifestyle), and sometimes a pharmacist or mental health professional. Open communication with this team is key. Don’t hesitate to ask questions, voice your concerns, share your experiences with medications, and discuss any side effects you might be experiencing. Shared decision-making ensures that your treatment plan aligns with your values and goals.
* Continuous Evaluation: Diabetes is a dynamic condition, and your body changes over time. What works today might need adjustment tomorrow. Your treatment plan is not set in stone; it’s a living document that should be continuously evaluated and updated. Your doctor will monitor your blood sugar levels (including A1c), blood pressure, weight, kidney function, and other relevant markers during regular check-ups. As your body changes, new health challenges arise, or even as new, more advanced medications become available, your treatment regimen may evolve. This ongoing assessment ensures that your diabetes management remains effective, safe, and tailored to your evolving needs, always striving for the best possible outcomes.
Monitoring and Proactive Side Effect Management
Even with medications known for favorable side effect profiles, being vigilant and proactive about monitoring your health is incredibly important. This ensures that any potential issues are caught and addressed quickly.
* Regular Check-ups: Consistent follow-up appointments with your healthcare team are absolutely non-negotiable for effective diabetes management. These visits allow your doctor to meticulously monitor your progress, assess how well your current medications are controlling your blood sugar, and perform necessary tests (like A1c, kidney function, and liver function) to check on your overall health. Crucially, these appointments are prime opportunities for your doctor to detect any emerging side effects early, even those you might not have noticed or considered significant. Early detection means faster intervention and less disruption to your health and well-being. Think of these check-ups as your regular health “tune-up.”
* Open Communication: This is perhaps the most vital aspect of managing side effects. It’s absolutely essential that you report any new or worsening symptoms to your healthcare provider, no matter how minor or insignificant they may seem to you. Sometimes, a subtle change could be an early indicator of a developing side effect, or it could be something unrelated that still needs attention. Don’t wait until your next scheduled appointment if something is bothering you. A quick call or message to your doctor’s office can make a big difference. Being an active participant in your care means being honest and thorough about how you’re feeling on your current medications. Your detailed feedback provides crucial information that helps your care team optimize your treatment.
* Adjustments and Alternatives: If a medication causes bothersome side effects that impact your quality of life, remember that you have options! Your doctor can often make adjustments that alleviate the problem. This might involve reducing the dosage of the medication, changing the timing of when you take it (e.g., taking it with food), or even trying a different medication within the same class (as sometimes individual formulations can be tolerated differently). If those approaches don’t work, your doctor can switch you to an entirely different class of drugs that works through a different mechanism and may therefore have a different side effect profile. The goal is always to find a balance where your diabetes is well-managed, and you feel good. There’s almost always an alternative or adjustment available, so never feel stuck with a medication that isn’t working for you.
Finding the optimal diabetes medicine involves a dynamic process of combining healthy lifestyle choices with carefully selected medications that offer the greatest benefits with the fewest manageable side effects. Remember, your personal “best” solution is one that effectively controls your blood sugar, supports your overall health goals, and maintains your quality of life. Don’t hesitate to discuss your concerns and explore all available options with your healthcare provider to tailor a treatment plan that’s right for you.
Frequently Asked Questions
Is it possible to find a diabetes medication with absolutely no side effects?
While no medication is entirely without potential side effects, many diabetes treatments are generally well-tolerated, and their benefits often outweigh the risks. The goal in diabetes management is to find the most effective medicine that causes the fewest and most manageable side effects for an individual. Your healthcare provider can help you navigate options to control your blood sugar effectively with minimal discomfort.
Which types of diabetes medications are generally considered to have the fewest or most manageable side effects?
Medications like metformin, often a first-line treatment for type 2 diabetes, are usually well-tolerated, though some gastrointestinal issues can occur initially. Newer classes such as GLP-1 receptor agonists and SGLT2 inhibitors also have good safety profiles for many people, often with benefits for cardiovascular and kidney health, despite potential initial digestive or genitourinary side effects, respectively. The “best” medicine depends entirely on your individual health profile and how your body responds.
How can I work with my doctor to find the best diabetes medication for me with minimal side effects?
Open communication with your doctor is crucial; clearly describe any side effects you experience, no matter how minor. Your healthcare provider can adjust dosages, switch medications, or suggest strategies to mitigate side effects, like taking medicine with food. Regular monitoring of your blood glucose levels and overall health will also help tailor your treatment plan for optimal control and minimal discomfort.
What lifestyle changes can complement diabetes medication to potentially reduce the need for higher doses or more aggressive treatments?
Significant lifestyle changes can greatly enhance the effectiveness of diabetes medication and sometimes even reduce the need for higher doses. Adopting a balanced diet, incorporating regular physical activity, maintaining a healthy weight, and managing stress are powerful tools. These actions not only help manage blood sugar levels but also improve overall health, potentially lessening the burden on medication alone.
Why do different diabetes medications have varying side effect profiles, and what are common ones to watch for?
Diabetes medications have different side effect profiles because they work through various mechanisms in the body to lower blood sugar. For instance, insulin can cause hypoglycemia (low blood sugar), while metformin might lead to digestive upset. SGLT2 inhibitors can increase the risk of genitourinary infections, and GLP-1 agonists may cause nausea. Understanding these potential effects with your doctor allows for informed choices and proactive management.
References
- https://www.niddk.nih.gov/health-information/diabetes/overview/medications-treatments
- Diabetes treatment: Using insulin to manage blood sugar – Mayo Clinic
- https://diabetes.org/health-wellness/medication
- https://www.cdc.gov/diabetes/managing/medicines.html
- https://my.clevelandclinic.org/health/articles/12061-oral-medications-for-type-2-diabetes
- https://www.health.harvard.edu/diseases-and-conditions/type-2-diabetes-drugs-and-you
- Diabetes management
- Treatment for type 2 diabetes – NHS

