The best rice for diabetics generally includes whole grain varieties with a lower glycemic index (GI), such as brown rice, wild rice, and whole-grain Basmati rice. These options are rich in fiber and digest more slowly than refined white rice, preventing rapid spikes in blood sugar levels. For individuals managing diabetes, carbohydrate intake is a primary concern, but this does not necessitate the complete elimination of rice from the diet. Instead, it requires a strategic approach focused on selecting grains with complex carbohydrate structures and managing the context in which they are consumed. By prioritizing high-fiber varieties and adhering to strict portion controls, individuals can maintain stable glucose levels while enjoying this global staple.
Why Glycemic Index Matters for Rice

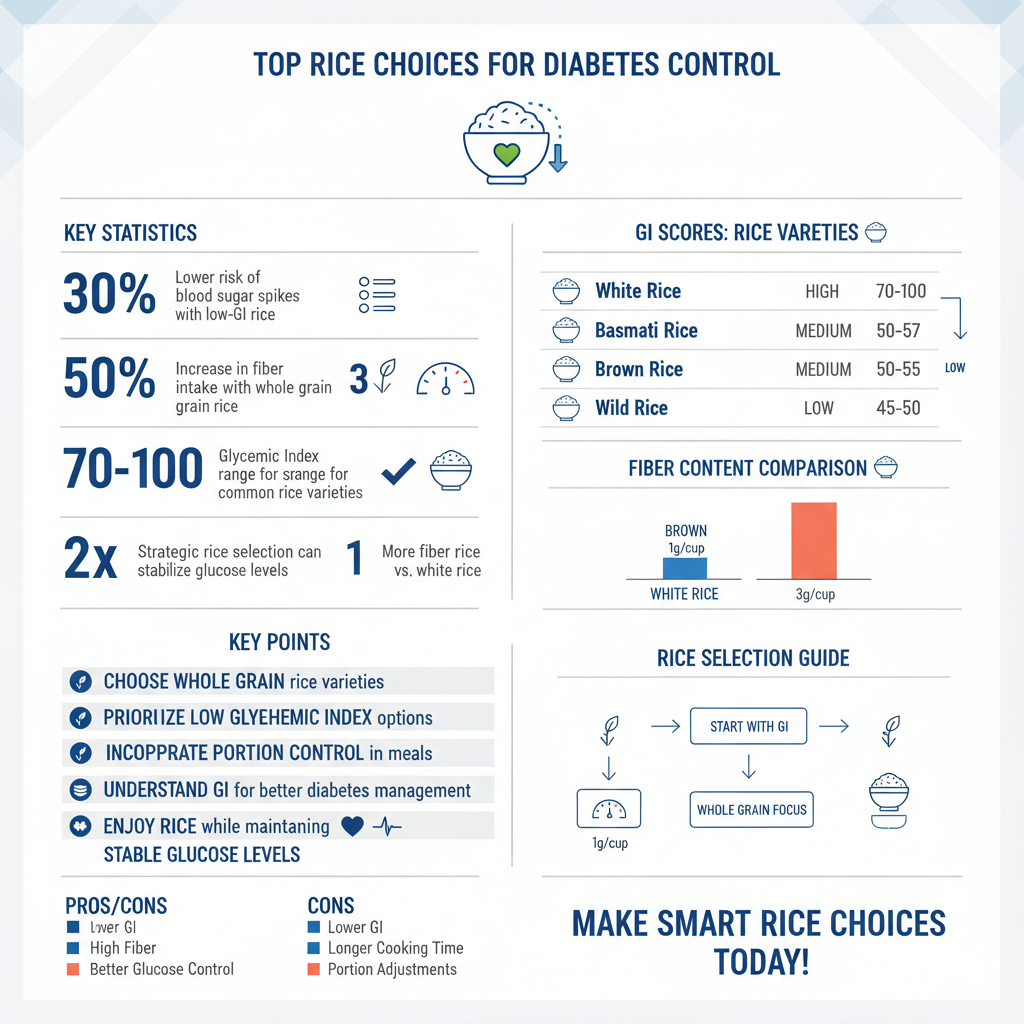
For individuals with diabetes, understanding the physiological impact of food is crucial, and the Glycemic Index (GI) serves as a vital tool in this regard. The GI is a ranking system that measures how quickly carbohydrate-containing foods raise blood glucose levels compared to pure glucose or white bread. The scale runs from 0 to 100, with lower numbers indicating a slower, more gradual release of sugar into the bloodstream.
When a person consumes high-GI foods, such as short-grain white rice or Jasmine rice, the body rapidly breaks down the simple starches into glucose. This results in a sharp “spike” in blood sugar, forcing the pancreas to release a surge of insulin. For a diabetic whose body is either resistant to insulin or unable to produce enough of it, this rapid spike can lead to hyperglycemia, fatigue, and long-term damage to blood vessels and nerves.
In contrast, lower-GI whole grain alternatives contain complex carbohydrate chains wrapped in fibrous layers. The body must work harder and take longer to break these grains down. This extended digestive process results in a slow, steady trickle of glucose into the bloodstream rather than a flood. This stability is the cornerstone of effective diabetes management, as it helps maintain energy levels and reduces the demand on insulin production. Therefore, selecting rice varieties based on their GI score is not merely a dietary preference but a medical necessity for optimal glycemic control.
Top Low-GI Rice Varieties

When selecting rice, the goal is to find varieties that offer nutritional density alongside a moderate to low glycemic impact. The following three options are widely considered the gold standard for diabetic-friendly grains.
Basmati Rice
Basmati rice, particularly the whole-grain or brown variety, is a standout option for diabetics. Unlike the sticky, short-grain rice often used in sushi, Basmati is a long-grain variety with a high content of amylose. Amylose is a type of starch that is difficult for the body to gelatinize and digest, resulting in a naturally lower GI.
While refined white Basmati has a lower GI than standard white rice, whole-grain Basmati is superior. It retains the outer bran layer, providing essential dietary fiber. A typical serving of whole-grain Basmati has a GI ranging between 50 and 58, categorizing it as a low-to-medium GI food. Its distinct aroma and fluffy texture make it an excellent culinary substitute for less healthy white rices in curries and pilafs.
Wild Rice
Despite its name, wild rice is not technically rice; it is the seed of a semi-aquatic grass native to North America. From a nutritional standpoint, it is a powerhouse. Wild rice boasts a significantly lower carbohydrate count and a higher protein content than true rice varieties.
Its benefits for diabetics are multifaceted. First, it has a low GI (approximately 57). Second, it is rich in antioxidants, specifically anthocyanins, which are known to reduce inflammation—a common complication of diabetes. Furthermore, wild rice is high in dietary fiber, zinc, and magnesium. Magnesium is particularly important as it plays a role in the body’s secretion of insulin and maintenance of insulin sensitivity. The texture of wild rice is chewy, which encourages slower eating and better satiety signals.
Brown Rice
Brown rice is the most accessible whole-grain alternative to white rice. It is essentially white rice that has not had the bran and germ removed during milling. These outer layers are where the vast majority of the grain’s nutrients reside.
The bran provides insoluble fiber, which acts as a physical barrier to digestion, slowing the absorption of the starchy endosperm. Brown rice generally has a GI of around 50 to 55, making it a safe staple when portioned correctly. Beyond glycemic control, the germ contains essential fatty acids and vitamins B and E. Switching from white to brown rice has been associated with a reduced risk of developing type 2 diabetes and better glycemic control in those already diagnosed.
Healthy Rice Alternatives

For those aiming for tighter glucose control or adhering to a low-carbohydrate diet (such as keto), traditional rice—even the brown varieties—might still contain too many carbohydrates. In these cases, rice alternatives offer similar textures with a fraction of the glycemic load.
Cauliflower Rice
Cauliflower rice has emerged as the premier low-carb substitute in the culinary world. Made by pulsing raw cauliflower florets in a food processor until they resemble rice grains, this vegetable substitute contains approximately 5 grams of carbohydrates per cup, compared to over 45 grams in a cup of brown rice.
Because it is a non-starchy vegetable, cauliflower rice has a negligible impact on blood sugar. It allows diabetics to fill their plate and enjoy the sensation of eating rice without the metabolic consequence. It absorbs flavors well, making it ideal for fried rice dishes, stir-fries, and burrito bowls.
Quinoa
Quinoa is a seed that is prepared and eaten like a grain. While its carbohydrate content is comparable to rice, its nutritional profile is far superior. Quinoa is one of the few plant sources that is a complete protein, meaning it contains all nine essential amino acids.
With a GI of around 53, quinoa is digested slowly. It is packed with fiber and minerals like potassium and iron. The high protein content is particularly beneficial for diabetics, as protein helps blunt the blood sugar response of a meal and keeps you feeling full longer, reducing the likelihood of snacking on high-sugar foods later.
Barley
Hulled barley is an underutilized grain that deserves a place in a diabetic diet. It has one of the lowest GI scores of all grains (around 28). The secret to barley’s efficacy is beta-glucan, a type of soluble fiber also found in oats.
When ingested, beta-glucan forms a viscous gel in the gut. This gel slows down gastric emptying and traps sugars, preventing them from being absorbed rapidly. Studies have shown that barley can significantly improve insulin sensitivity and lower cholesterol levels. Its chewy texture and nutty flavor make it an excellent substitute for rice in soups, stews, and risottos.
Importance of Portion Control
Choosing the right type of rice is only half the battle; the quantity consumed is equally critical. Even low-GI foods can cause hyperglycemia if eaten in excess. This concept is known as the “glycemic load,” which accounts for both the quality of the carbohydrate and the serving size.
The “Plate Method”
To manage portions without needing to weigh food constantly, the American Diabetes Association recommends the “Diabetes Plate Method.” In this visual guide, a standard 9-inch dinner plate is divided into sections:
* One-half of the plate should be filled with non-starchy vegetables (greens, broccoli, peppers).
* One-quarter should be lean protein.
* One-quarter is reserved for carbohydrate foods, including rice.
Limiting rice to one-quarter of the plate ensures that the meal is voluminous and filling but relatively low in total carbohydrates.
Recommended Serving Sizes
For those who prefer precise measurements, the recommended serving size for cooked rice is typically 1/3 to 1/2 cup. This amount generally provides 15 to 30 grams of carbohydrates. It is important to note that restaurant portions of rice are often three to four times this amount. Diabetics should be vigilant about measuring portions at home to train their eye to recognize appropriate serving sizes when dining out.
Cooking Tips to Lower Blood Sugar Impact
Science has revealed that the way rice is cooked and treated can alter its chemical structure in a way that benefits diabetics. By utilizing food chemistry, you can lower the GI of the rice before it ever hits your plate.
The Benefits of Cooling (Resistant Starch)
One of the most effective methods to lower the glycemic impact of rice is to cook it and then cool it in the refrigerator for at least 12 to 24 hours. This process causes a phenomenon known as “starch retrogradation.” As the starch molecules cool, they recrystallize into a structure known as resistant starch.
Resistant starch functions like soluble fiber; it resists digestion in the small intestine and ferments in the large intestine. This means fewer calories and less glucose are absorbed into the bloodstream. Interestingly, reheating the rice does not reverse this process significantly, meaning leftovers are often healthier for diabetics than freshly cooked rice.
Adding Healthy Fats and Acids
The speed of digestion can also be manipulated by what is added to the pot.
* Healthy Fats: Adding a teaspoon of coconut oil or olive oil to the boiling water before adding the rice can coat the starch granules. This lipid barrier slows down the enzymes (amylase) responsible for breaking starch into sugar.
* Acids: Adding vinegar (such as rice vinegar or apple cider vinegar) or lemon juice to a rice dish can lower the meal’s GI by 20-30%. Acidity slows gastric emptying, keeping food in the stomach longer and flattening the glucose curve.
Pairing Rice for Better Balance
A diabetic diet focuses on the total composition of the meal rather than isolated ingredients. “Naked carbs”—eating carbohydrates on their own—should be avoided. Pairing rice with the right macronutrients can act as a buffer against blood sugar spikes.
Combining with High-Fiber Vegetables
Fiber is the ultimate regulator of blood sugar. When rice is eaten alongside fibrous vegetables like spinach, kale, broccoli, or green beans, the fiber creates a mesh in the digestive tract. This mesh slows the movement of food and the absorption of nutrients. For example, rather than having a bowl of plain rice, mixing it with an equal amount of sautéed vegetables can halve the effective glycemic load of the bite.
Adding Lean Proteins
Protein is complex to digest and requires energy to break down (the thermic effect of food). When you consume protein (chicken, fish, tofu, legumes) before or with your rice, it significantly slows down the rate at which carbohydrates are emptied from the stomach. This results in a much lower postprandial (post-meal) glucose peak compared to eating rice alone. Plant-based proteins like lentils or beans are excellent pairings, as they provide both protein and additional fiber.
Conclusion
Choosing the right rice involves selecting low-GI options like basmati or wild rice and strictly managing portion sizes to avoid hyperglycemia. While rice is a carbohydrate-dense food, it does not need to be completely forbidden. By utilizing cooking methods that increase resistant starch, such as cooling, and adhering to the “Plate Method,” individuals can navigate their diet safely. Most importantly, by pairing these grains with plenty of fiber and protein, you can enjoy rice as part of a balanced diabetes-friendly diet; always consult your healthcare provider or dietitian for personalized advice to ensure these choices align with your specific medical needs.
Frequently Asked Questions
Which type of rice has the lowest glycemic index (GI) for diabetics?
Black rice (often called “forbidden rice”) and wild rice generally have the lowest glycemic index scores, making them the safest options for blood sugar management. These varieties are rich in fiber, antioxidants, and protein, which helps slow down digestion and prevents rapid spikes in glucose levels compared to refined white rice. Many nutritionists also recommend red rice as a nutrient-dense alternative with a similarly low GI profile.
Is Basmati rice considered safe for people with diabetes?
Yes, whole-grain Basmati rice is considered one of the better options for diabetics because it has a lower to medium glycemic index (around 50-58) compared to short-grain white rice. The long grains of Basmati contain a specific type of starch called amylose, which takes longer for the body to break down, resulting in a slower release of sugar into the bloodstream. However, portion control remains essential, and it should ideally be paired with fiber-rich vegetables.
How does the “cooling method” make rice healthier for diabetics?
Cooking rice and then cooling it in the refrigerator for at least 12 to 24 hours increases its resistant starch content, which functions similarly to soluble fiber. This process changes the chemical structure of the starch so that it resists digestion in the small intestine, leading to a reduced glycemic response when you eat it. Interestingly, reheating the rice afterward does not destroy this beneficial resistant starch.
Is brown rice actually better than white rice for blood sugar control?
Brown rice is significantly better than standard white rice for blood sugar control because it retains the bran and germ layers, which are stripped away during the processing of white rice. These layers provide essential fiber and magnesium, nutrients that improve insulin sensitivity and slow the absorption of carbohydrates. Switching from white to brown rice can significantly lower the overall glycemic load of a meal.
What is the recommended portion size of rice for a diabetic meal plan?
While individual carbohydrate needs vary, most dietitians recommend limiting rice consumption to a portion size of roughly ½ cup to ¾ cup of cooked rice per meal. To minimize blood sugar spikes, this portion should never be eaten alone; it should always be balanced with lean proteins (like chicken or tofu) and healthy fats to further slow down digestion. Monitoring your post-meal glucose levels is the best way to determine your personal tolerance.
References
- News | Harvard T.H. Chan School of Public Health
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3024208/
- Glycaemic index and diabetes | Diabetes UK
- https://health.clevelandclinic.org/is-brown-rice-good-for-you
- https://www.healthhub.sg/live-healthy/why_whole_grains_are_the_smart_choice
- Diabetes diet: Create your healthy-eating plan – Mayo Clinic
- https://www.nutritionletter.tufts.edu/healthy-eating/health-benefits-of-black-rice/


